| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 16, Number 2, April 2023, pages 68-78
Transjugular Intrahepatic Portosystemic Shunt With or Without Gastroesophageal Variceal Embolization for the Prevention of Variceal Rebleeding: A Systematic Review and Meta-Analysis
Fouad Jabera, l, Azizullah Beranb, Saqr Alsakarneha, Khalid Ahmedc, Mohamed Abdallahd, Khaled Elferte, Mohammad Almeqdadif, Mohammed Jaberg, Wael T. Mohameda, Mohamd Ahmeda, Laith Al Momanih, Laith Numani, Thomas Biermanj, k, John H. Helzbergj, k, Hassan Ghozj, Wendell K. Clarkstonj, k
aDepartment of Internal Medicine, University of Missouri Kansas City, Kansas City, MO, USA
bDepartment of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN, USA
cDepartment of Internal Medicine, The Wright Medical Center for Graduate Medical Education, Scranton, PA, USA
dDivision of Gastroenterology and Hepatology, Department of Medicine, University of Minnesota, Minneapolis, MN, USA
eDepartment of Internal Medicine, SBH Health System, New York, NY, USA
fDepartment of Transplant Hepatobiliary Disease, Lahey Hospital and Medical Center, Burlington, MA, USA
gDepartment of Medical Education, Al-Azhar University, Gaza, Palestine
hDepartment of Gastroenterology and Hepatology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
iDepartment of Gastroenterology and Hepatology, Saint Louis University School of Medicine, Saint Louis, MO, USA
jDepartment of Gastroenterology and Hepatology, University of Missouri Kansas City, Kansas City, MO, USA
kDepartment of Gastroenterology and Hepatology, Saint Luke’s Hospital, Kansas City, MO, USA
lCorresponding Author: Fouad Jaber, Department of Internal Medicine, University of Missouri Kansas City, Kansas City, MO, USA
Manuscript submitted March 27, 2023, accepted April 14, 2023, published online April 28, 2023
Short title: TIPS With or Without VE for Variceal Rebleeding
doi: https://doi.org/10.14740/gr1618
| Abstract | ▴Top |
Background: The role of variceal embolization (VE) during transjugular intrahepatic portosystemic shunt (TIPS) creation for preventing gastroesophageal variceal rebleeding remains controversial. Therefore, we performed a meta-analysis to compare the incidence of variceal rebleeding, shunt dysfunction, encephalopathy, and death between patients treated with TIPS alone and those treated with TIPS in combination with VE.
Methods: We performed a literature search using PubMed, EMBASE, Scopus, and Cochrane databases for all studies comparing the incidence of complications between TIPS alone and TIPS with VE. The primary outcome was variceal rebleeding. Secondary outcomes include shunt dysfunction, encephalopathy, and death. Subgroup analysis was performed based on the type of stent (covered vs. bare metal). The random-effects model was used to calculate the relative risk (RR) with the corresponding 95% confidence intervals (CIs) of outcome. A P value < 0.05 was considered statistically significant.
Results: Eleven studies with a total of 1,075 patients were included (597: TIPS alone and 478: TIPS plus VE). Compared to the TIPS alone, the TIPS with VE had a significantly lower incidence of variceal rebleeding (RR: 0.59, 95% CI: 0.43 - 0.81, P = 0.001). Subgroup analysis revealed similar results in covered stents (RR: 0.56, 95% CI: 0.36 - 0.86, P = 0.008) but there was no significant difference between the two groups in the subgroup analysis of bare stents and combined stents. There was no significant difference in the risk of encephalopathy (RR: 0.84, 95% CI: 0.66 - 1.06, P = 0.13), shunt dysfunction (RR: 0.88, 95% CI: 0.64 - 1.19, P = 0.40), and death (RR: 0.87, 95% CI: 0.65 - 1.17, P = 0.34). There were similarly no differences in these secondary outcomes between groups when stratified according to type of stent.
Conclusions: Adding VE to TIPS reduced the incidence of variceal rebleeding in patients with cirrhosis. However, the benefit was observed with covered stents only. Further large-scale randomized controlled trials are warranted to validate our findings.
Keywords: Transjugular intrahepatic portosystemic shunt; Variceal bleeding; Variceal embolization; Embolotherapy
| Introduction | ▴Top |
Bleeding from gastroesophageal varices is a well-known and life-threatening complication of liver cirrhosis with a mortality rate up to 30% [1]. The transjugular intrahepatic portosystemic shunt (TIPS) has been used for secondary prophylaxis to prevent recurrent variceal bleeding [1, 2]. Even after placement of TIPS, there is a 20-30% risk of recurrent bleeding, mainly due to shunt dysfunction or fragile patent varices in an open shunt [3-5].
The additional use of esophagogastric variceal embolization (VE) with TIPS is thought to reduce the risk of variceal rebleeding, as well as the risk of hepatic encephalopathy compared to TIPS alone [6, 7]. A meta-analysis of six studies [8] suggested that combining embolic therapy with TIPS helps prevent variceal rebleeding. The finding of this meta-analysis [8] should be interpreted with caution since there was only one randomized controlled trial (RCT). Therefore, high-quality studies supporting this evidence were lacking. Furthermore, the stents used for TIPS placement in these studies were most commonly bare stents, which have a higher risk of rebleeding, and shunt dysfunction compared to polytetrafluoroethylene-coated stents [9-13]. Recent studies [14-16] found conflicting results, with a recent RCT [17] showing the incidence of rebleeding comparable between patients receiving TIPS alone compared to TIPS with concomitant VE. The RCT was a single study, and most of the included patients had hepatitis B virus (HBV)-related liver cirrhosis. The results can, therefore, only be generalized to a limited extent.
Due to these contradictory findings and the above-mentioned limitations, we performed a systematic review and meta-analysis to compare the incidence of post-TIPS complications between patients with liver cirrhosis and refractory variceal bleeding who were treated with TIPS alone versus patients treated with TIPS plus VE.
| Materials and Methods | ▴Top |
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions [18]. The Institutional Review Board approval was not required for this study. The study was registered at PROSPERO (ID: CRD42023396335) and conducted according to the Declaration of Helsinki statement.
Literature search
We performed a literature search from inception to November 5, 2022, using PubMed, EMBASE, Scopus, and Cochrane databases for all studies comparing the incidence of complications between TIPS alone and TIPS with VE. The following keywords: “transjugular intrahepatic portosystemic shunt”, “TIPS”, “embolization”, “embolotherapy”, were used in various combinations to identify studies reporting post-TIPS alone or post-TIPS plus embolization complications in patients with liver cirrhosis. We also hand-searched the reference lists of all included studies as well as previous meta-analyses (backward snowballing) to find articles that may have been missed in the literature search. The search was not limited to restrictions of region or publication type. Notably, the non-English language papers were also included in our meta-analysis to minimize language bias. Two authors independently conducted the literature search in consultation with an experienced medical librarian.
Eligibility criteria
Inclusion criteria were as follows: 1) patients who had a history of gastroesophageal variceal bleeding and underwent TIPS, with or without VE; 2) the incidence of shunt dysfunction, variceal rebleeding, encephalopathy, or death was compared between the two groups; 3) either RCTs or non-randomized comparative studies. We excluded studies that 1) provided insufficient information about the outcomes of TIPS or their outcome to calculate event rate for our main results; 2) case studies, editorials, opinions, letters to the editor, book chapters, animal studies, or meta-analysis.
Data extraction
We first searched the databases for studies performed in human subjects describing post-TIPS alone with post-TIPS plus embolization complications in patients with variceal bleeding. Relevant studies were screened based on title and abstract by two investigators independently, then studies meeting our inclusion criteria were selected after performing an electronic search. Thereafter, all studies that passed the initial filtering process were thoroughly reviewed and evaluated. Data from eligible studies were extracted into a standardized table for analysis. The entire content of each article was independently assessed by two researchers using predetermined selection criteria and scoring methods. We extracted the following data from included studies: the first author, publication year, the country where the study was conducted, period of enrollment, study design, type of TIPS stent, embolization technique, type of embolic agents, number of patients per group, age, sex, follow-up duration, and number of events (shunt dysfunction, variceal rebleeding, encephalopathy, and death).
Quality and publication bias assessment
Using the Newcastle-Ottawa scale (NOS) [19] for cohort studies and Jadad scale for reporting RCTs [20], the methodological quality of the included studies was assessed independently by two investigators. A third author addressed any discrepancy. Points (maximum 9 points) were awarded for each cohort based on a developed checklist for the cohort studies. Studies with more than 6 points were considered to be of good quality; those with 5 - 6 points were considered studies of reasonable quality, and those with < 5 points were studies of poor quality. Points (maximum 8) were awarded for RCTs based on the modified Jadad scale. In the modified Jadad score, the study was considered as high quality for the total Jadad score of ≥ 3 if blinding was feasible. Study designs in which blinding was not feasible, a score of ≥ 2 was considered high quality. For primary outcome (variceal rebleeding), publication bias was assessed qualitatively by visually assessing the funnel plot and quantitively using Egger’s regression analysis. If the P value of Egger regression was < 0.10, the publication bias was considered significant.
Data synthesis and statistical analysis
A random-effects model within the Mantel-Haenszel method was used to assess the outcomes. The outcomes were summarized as a pooled risk ratio (RR) with the corresponding 95% confidence intervals (CIs). P values < 0.05 were considered statistically significant. Heterogeneity was evaluated using the I2 statistic, as outlined in the Cochrane handbook for systematic reviews, and I2 value of 50% or more was considered significant heterogeneity. All statistical analyses were conducted by Review Manager 5.4 and Comprehensive Meta-Analysis 3.3. To confirm the robustness of our results, we conducted a leave-one-out sensitivity analysis for the primary outcome (variceal bleeding). We also conducted subgroup analysis based on the stent type (covered vs. bare vs. mixed).
| Results | ▴Top |
Study selection
Overall, 3,043 articles were initially identified by our search strategy. Among them, 13 studies [9-17, 21-24] initially met eligibility criteria, but then two were removed, leaving 11 in the final analysis [9-17, 21, 22] (Fig. 1). Notably, two studies were conducted by Gaba et al, and were based on the same database [12, 23]. Because the study published in 2010 had more comprehensive information than that published in 2012, the latter study was excluded from our meta-analysis. In addition, two studies were conducted in the same institution [10, 24]. As the period of enrollment was May 2007 to June 2010 in the study of Wei et al [24], and May 2007 to July 2011 in the study of Chen et al [10], the former study was excluded from our meta-analysis. Thus, a total of eleven studies were included in our meta-analysis. A summary of the study characteristics included is presented in Table 1 [9-17, 21, 22].
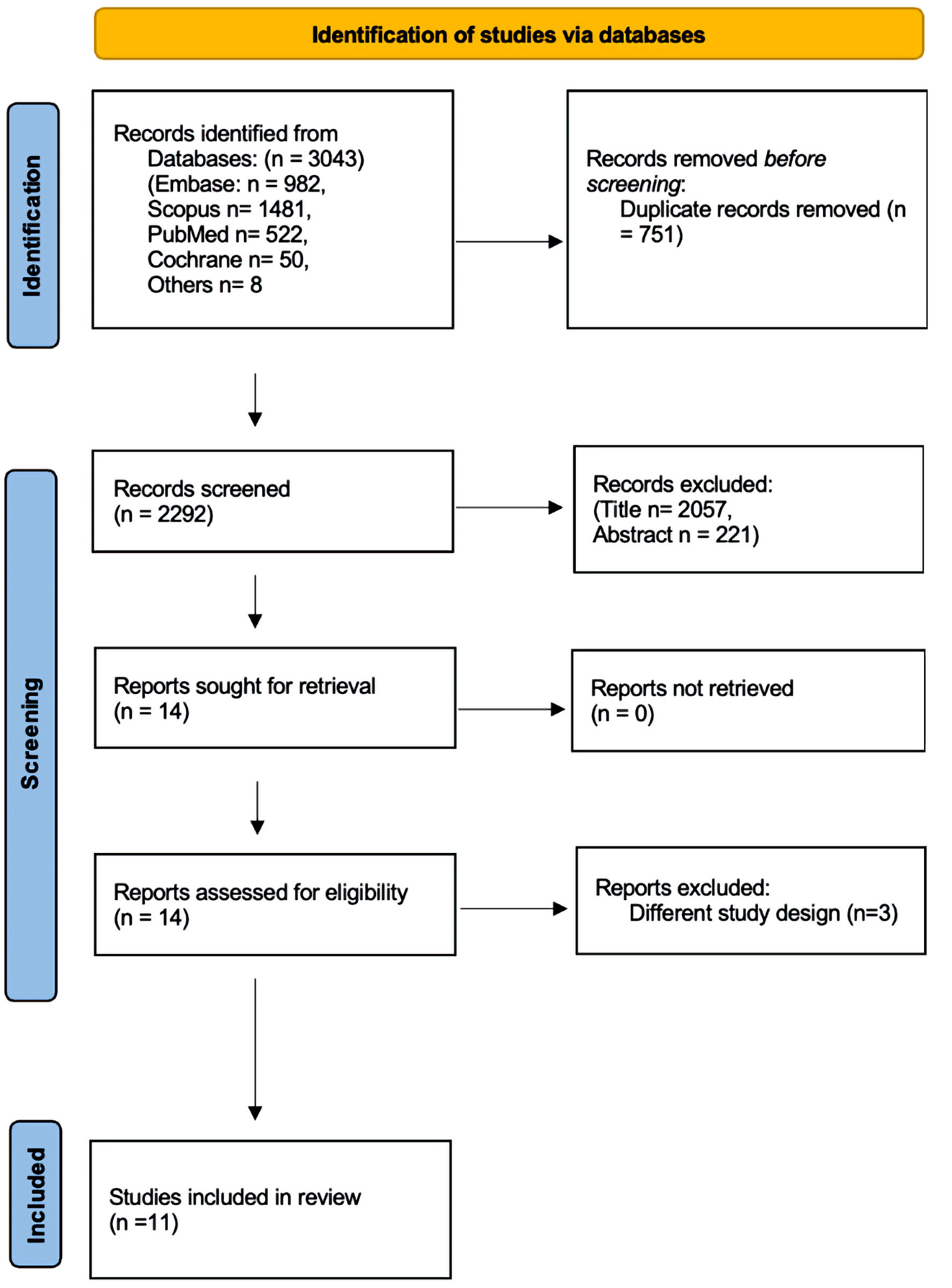 Click for large image | Figure 1. PRISMA flowchart for the selection process. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses. |
 Click to view | Table 1. Baseline Characteristics of the Included Studies |
Baseline characteristics of studies
All included studies were published between 2004 and 2022. Of these, two were RCTs [10, 17], and nine [9, 11-16, 21, 22] were non-randomized studies (Table 1) [9-17, 21, 22]. A total of 1,075 patients were included: 597 (50.5%) in the TIPS alone group and 478 (49.5%) in the TIPS plus VE group (Table 1) [9-17, 21, 22]. VE was performed after TIPS in eight studies, before TIPS in two studies and unspecified in one study (Table 2) [9-17, 21, 22]. Subgroup analyses were performed according to the type of stents. The type of stents was covered stent alone in six studies [10, 12, 14-17], bare stent alone in two studies [9, 11], combined (both bare and covered stent) in two studies [13, 21], and unknown in one study [22]. Varices were angiographically embolized by coils with or without liquids agents or vascular plugs in 10 studies, with one study using sclerosing agents only [16]. Liquid agents were employed in six studies, including α-cyanoacrylate (n = 1), ethanol (n = 1), and sclerosing agents (n = 4).
 Click to view | Table 2. Baseline Patients Characteristics of the Included Studies |
Variceal rebleeding
Eleven studies reported data regarding the incidence of variceal rebleeding. The TIPS with VE was associated with a significantly lower incidence of variceal rebleeding than the TIPS alone (RR: 0.59, 95% CI: 0.43 - 0.81, P = 0.001, I2 = 18%) (Fig. 2). The results remained consistent on the leave-one-out sensitivity analysis (Supplementary Material 1, www.gastrores.org).
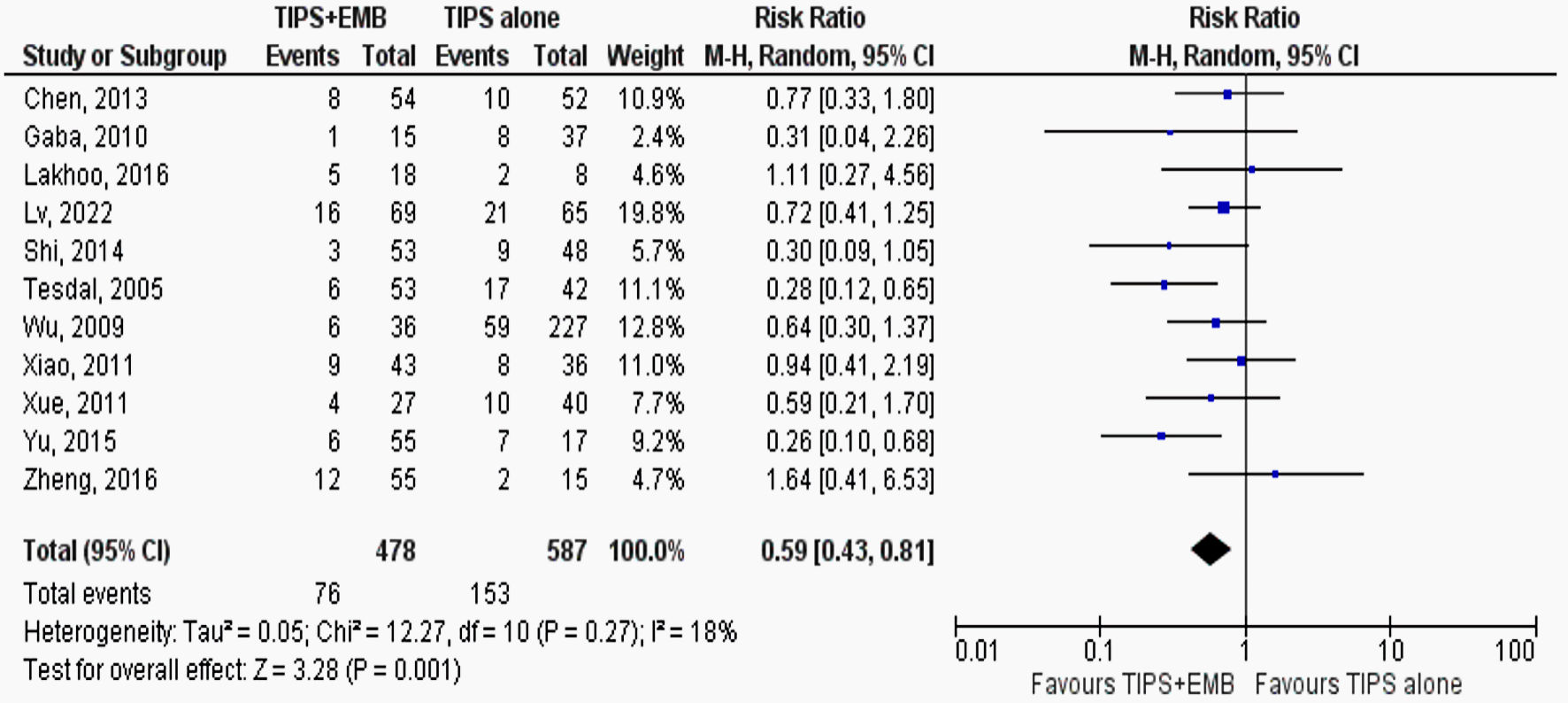 Click for large image | Figure 2. Forest plots of meta-analyses comparing the incidence of variceal rebleeding between the TIPS alone groups and TIPS combined with variceal embolization group (TIPS + EMB). TIPS: transjugular intrahepatic portosystemic shunt; EMB: embolization; CI: confidence interval. |
Subgroup analysis based on stent type showed consistent results favoring TIPS with VE over TIPS alone with covered stents (RR: 0.56, 95% CI: 0.36 - 0.86, P = 0.008, I2 = 15%) (Fig. 3), but there was no significant difference between the two groups with bare stents or mixed stents (Fig. 3).
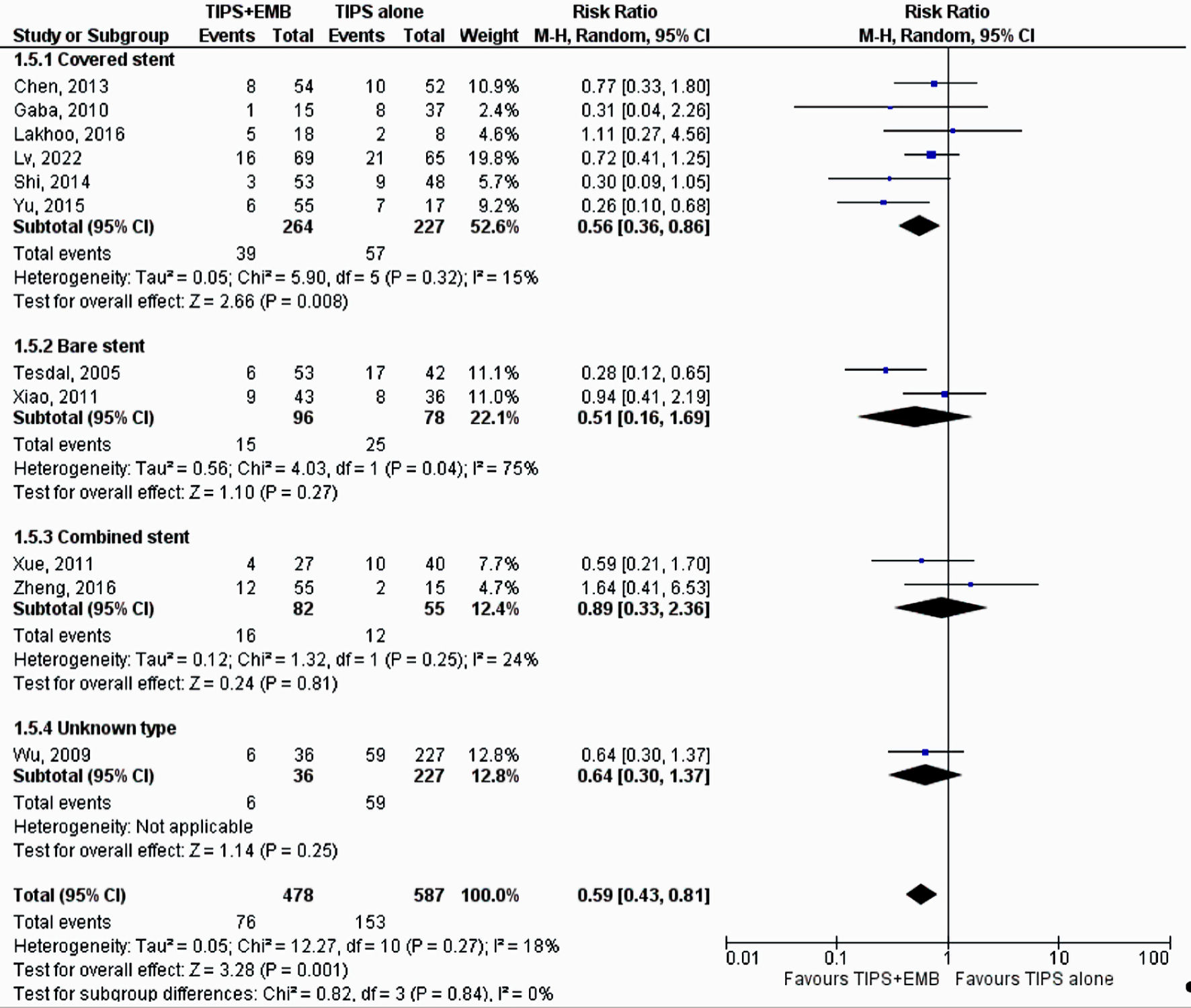 Click for large image | Figure 3. Forest plots of meta-analyses comparing the incidence of variceal rebleeding between the TIPS alone groups and TIPS combined with variceal embolization group (TIPS + EMB) based on stent types (covered vs. bare vs. combined vs. unknown). TIPS: transjugular intrahepatic portosystemic shunt; EMB: embolization; CI: confidence interval. |
Encephalopathy
Eight studies reported the incidence of encephalopathy [9, 10, 13, 14, 16, 17, 21, 22]. There was no difference between the two group in the incidence of encephalopathy (RR: 0.84, 95% CI: 0.66 - 1.06, P = 0.13, I2 = 5%) (Fig. 4a). The results remained consistent in the subgroup analysis based on stent type (Supplementary Material 2, www.gastrores.org).
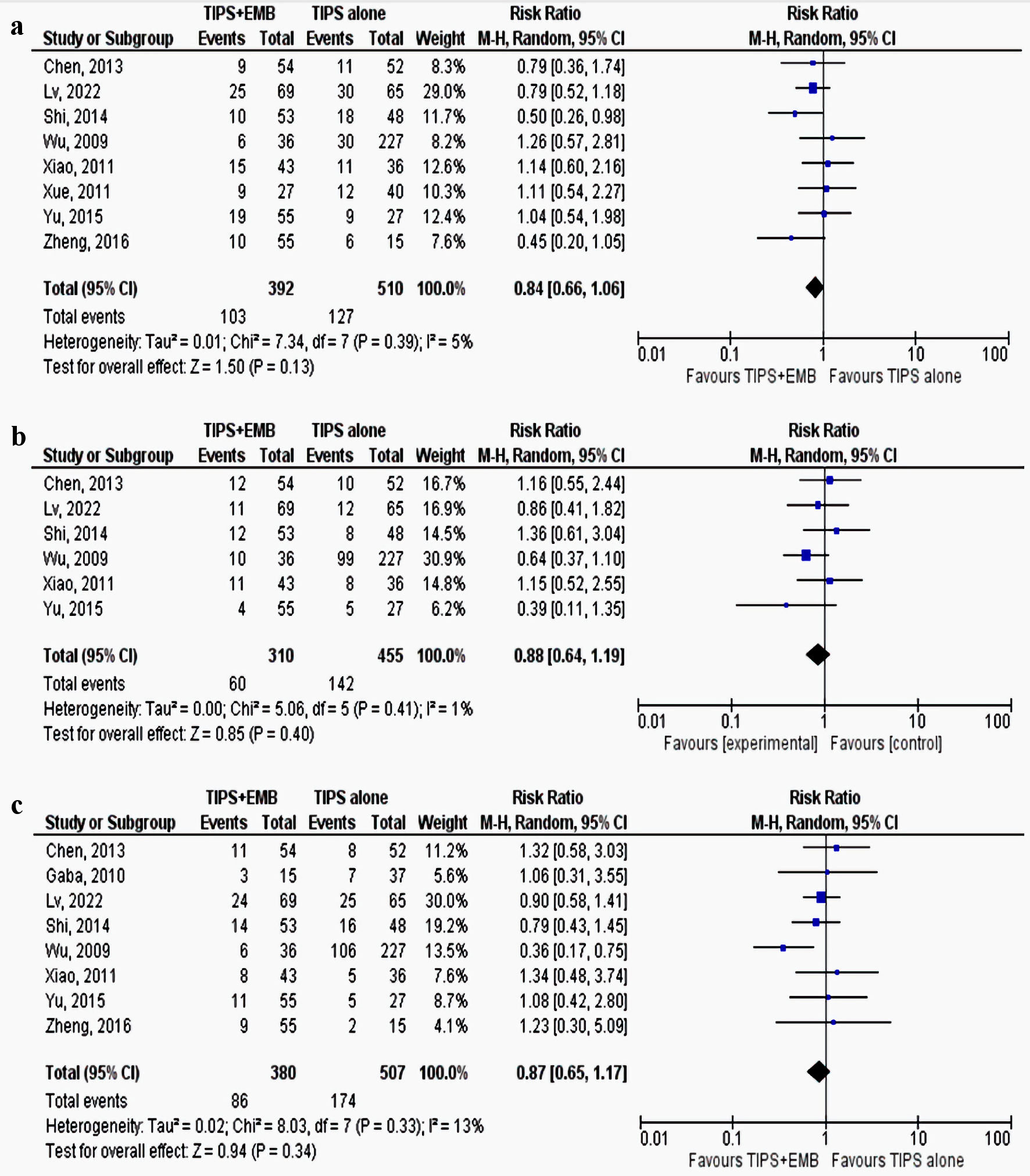 Click for large image | Figure 4. Forest plots of meta-analyses comparing the incidence of (a) encephalopathy, (b) shunt dysfunction, and (c) mortality between the TIPS alone groups and TIPS combined with variceal embolization group (TIPS + EMB). TIPS: transjugular intrahepatic portosystemic shunt; EMB: embolization; CI: confidence interval. |
Shunt dysfunction
Six studies reported the incidence of shunt dysfunction [9, 10, 14, 16, 17, 22]. Shunt dysfunction was similar between TIPS with VE and TIPS alone groups (RR: 0.88, 95% CI: 0.64 - 1.19, P = 0.40, I2 = 1%) (Fig. 4b). The results were also consistent in the subgroup analysis based on stent type (Supplementary Material 3, www.gastrores.org).
Death
The death rate was similar between TIPS with VE and TIPS alone groups (RR: 0.87, 95% CI: 0.65 - 1.17, P = 0.34, I2 = 13%) (Fig. 4c). The results also remained consistent in the subgroup analysis based on stent type (Supplementary Material 4, www.gastrores.org).
Quality and publication bias assessment
The two RCTs were considered of high quality using the modified Jadad scale (Supplementary Material 5, www.gastrores.org). Six of the remaining studies were high quality using the NOS, while the remaining three were of medium quality (Supplementary Material 6, www.gastrores.org). There was no evidence of publication bias for the primary outcome (variceal rebleeding) as shown here (Supplementary Material 7, www.gastrores.org).
| Discussion | ▴Top |
The effectiveness of VE during the TIPS procedure in reducing variceal rebleeding and other post-TIPS complications remains controversial. In this meta-analysis, we systemically examined outcomes after TIPS alone compared to TIPS plus VE. We found that simultaneous VE at the time of TIPS is associated with fewer rebleeding episodes than TIPS alone. In addition, the significant difference between the two groups could be only observed in the subgroup meta-analysis of studies with covered stents alone, but not that with bare stents alone or with the combined type of stents. Furthermore, we found no evidence that concomitant VE is beneficial regarding shunt dysfunction, encephalopathy, and mortality between the two groups.
It is assumed that persistent patency of the varices after TIPS and shunt closure are possible causes of recurrent variceal bleeding after placement of TIPS [10]. It has been hypothesized that patent collateral vessels, if embolized, would increase flow in TIPS, thereby reducing the likelihood of shunt dysfunction that can lead to variceal rebleeding [10]. In addition, elevated systemic venous pressure greater than 15 mm Hg represents a risk of variceal rebleeding after TIPS [12, 25]. Our meta-analysis, which included 11 studies, found that the rate of variceal rebleeding was significantly lower in the TIPS-plus VE group compared to the TIPS-only group (RR: 0.621, 95% CI: 0.47 - 0.819, P < 0.001). Qi et al [8] performed a meta-analysis on six studies and found similar results. A previous RCT by Chen et al [10] supported our results by reporting a lower 6-month rebleeding rate in patients receiving VE plus TIPS (6%) versus TIPS alone (20%). These results differ from a recent RCT by Lv et al [17], who reported no significant difference in variceal and all-cause rebleeding between the two cohorts. In this RCT [17], the authors suggested that the lack of reduction in rebleeding from all causes was probably due to achieving less than 12 mm Hg portacaval pressure gradient (PPG; measured as the difference between the portal vein and the inferior vena cava pressures in most patients), in addition to the favorable shunt patency due to the use of covered stents [17].
According to the type of TIPS stents, subgroup analysis showed similar results of reducing variceal bleeding when using covered stents but not with bare stents or combined stents. This could be explained by the fact that the diameter of bare stents tends to decrease over time. Thus, there is no sustainability in the decrease in PPG attained after TIPS, and this is progressively lost until TIPS revision is required. The resultant shunt dysfunction is the main reason for variceal rebleeding. It is worth noting that covered stents have a higher patency (80-90%) [26-29] and have resulted in reduction of recurrent variceal bleeding to < 10% after TIPS [27, 29, 30]. However, other considerations have been explored to further reduce post-TIPS bleeding due to the significant morbidity and mortality associated with gastrointestinal variceal bleeding [31]. Elevation of systemic venous pressure greater than 15 mm Hg and stent dysfunction were found to be risk factors for recurrent bleeding after TIPS. Adjunctive gastroesophageal VE could potentially address these risk factors by occluding venous collateral channels, which can recanalize in the presence of elevated systemic venous pressure or stenotic or occluded shunts. The combined benefits of covered stents and adjunctive VE might explain our results of the statistically significant reduction in variceal bleeding with the setting of covered stents, but not with the bare or combined stents.
Studies have shown that failure of varices resolution after TIPS could be due to various etiologies. These include shunt dysfunction, which may be secondary to thrombosis, or collapse of the TIPS tract due to stent retraction into the liver parenchyma [10, 16, 17]. Our analysis showed no significant difference in shunt dysfunction and encephalopathy between patients who underwent TIPS plus VE compared to TIPS only. Similarly, Lv et al [17] found no difference in shunt dysfunction rates between patients with TIPS plus VE vs. TIPS alone. Lv et al [17] hypothesized that better shunt patency, which was achieved through optimal stent placement, might partially explain the nonsignificant difference in rebleeding rates since shunt dysfunction is a cause of recurrent variceal bleeding after TIPS placement [17]. In addition, it is unclear whether shunt diameter contributes to the risks of hepatic encephalopathy, but the data suggest that a larger shunt diameter may be the culprit behind the development of this complication [12, 25, 32]. Higher encephalopathy rates were observed after TIPS in patients who only had large (> 6 mm) spontaneous portosystemic shunts, while no significant worsening of hepatic encephalopathy was reported in patients with small spontaneous portosystemic shunts [33]. In addition, Shi et al [16] showed that patients with recurrent encephalopathy who underwent shunt diameter reduction showed an improvement in their symptoms.
Our study is not free from limitations. Most included studies were observational retrospectives with variations in patients’ characteristics, the stage of liver cirrhosis, MELD score, and Child-Pugh scores. In addition, other reasons contribute to the limitations of our meta-analysis and warrant cautious interpretation of the finding. First, the location of the varices was inconsistent between studies (Table 2) [9-17, 21, 22]. The level of the varices can interfere with the effectiveness of VE. Second, the degree of embolization could influence recurrent variceal bleeding. While proximal afferent vessel embolization using coils alone could potentially allow sustained variceal perfusion via collaterals, distal embolization via fluid agents helps occlude the variceal space or cause thrombosis [8]. A combination of coils and liquid agents, such as cyanoacrylate and ethanol, may be recommended to achieve long-acting embolization proximally and distally to prevent new collaterals formation [8]. The variability in embolic agents makes it difficult to determine which embolic agent or combination of agents would produce a better outcome. Third, while the indication for TIPS was variceal bleeding in all studies, the indication for VE was variable. Adjunctive VE was performed as needed in retrospective studies; persistent varices with a pressure gradient greater than 12 mm Hg after TIPS. Fourth, follow-up period for primary and secondary outcomes in the studies varied from few months to few years. This could have introduced heterogeneity and potential bias in the study. In addition, the timing of embolization may differ in the included studies. Some may perform embolization after TIPS when the risk of rebleeding was high, rather than performing truly simultaneous embolization. This could lead to a selection bias that excludes patients with a higher risk for embolization. Finally, heterogeneity in the technique used to perform the TIPS procedure and VE technique may have influenced the results. Further studies with large sample sizes and consistent embolic therapy agents and techniques are warranted to confirm our results.
Despite the limitation, our meta-analysis includes pooling a larger sample size, a total of 1,075 patients, to provide evidence for an important clinical question. In addition, we analyzed the post-TIPS outcomes based on the type of stents, given recent evidence demonstrating that covered stents have better shunt patency than bare stents [9-13].
To conclude, our meta-analysis suggests that simultaneous VE at the time of TIPS in patients with gastroesophageal variceal bleeding is associated with fewer rebleeding episodes than TIPS alone. The difference was observed only in studies with covered stents, supporting that these stents could have better outcomes in reducing variceal rebleeding. In addition, rates of shunt dysfunction, encephalopathy, and mortality were similar in patients treated with TIPs plus VE compared to TIPS alone. Nevertheless, the individual risk-benefit balance should be implemented when considering adding VE during TIPS. Given the different indications for VE, stent type, embolic agent, and location of the varices, additional well-designed RCTs with a larger sample size are warranted to validate whether there is a meaningful difference in therapeutic efficacy.
| Supplementary Material | ▴Top |
Suppl 1. Leave-one-out sensitivity analysis for studies comparing variceal rebleeding between the TIPS alone group and TIPS combined with variceal embolization group.
Suppl 2. Forest plots of meta-analyses comparing the incidence of encephalopathy between the TIPS alone group and TIPS combined with variceal embolization group based on stent types (covered vs. bare vs. combined vs. unknown).
Suppl 3. Forest plots of meta-analyses comparing the incidence of shunt dysfunction between the TIPS alone group and TIPS combined with variceal embolization group based on stent types (covered vs. bare vs. combined vs. unknown).
Suppl 4. Forest plots of meta-analyses comparing the incidence of mortality between the TIPS alone group and TIPS combined with variceal embolization group based on stent types (covered vs. bare vs. combined vs. unknown).
Suppl 5. Quality assessment of the included studies in the meta-analysis using Newcastle-Ottawa scale.
Suppl 6. Quality assessment of the included RCTs in the meta-analysis using modified Jadad scale.
Suppl 7. Funnel plot for the primary outcome (rebleeding).
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
All other authors have no conflict of interest to disclose.
Informed Consent
Not applicable.
Authors Contributions
Conception and design: Fouad Jaber, Azizullah Beran, Saqr Alsakarneh, Khalid Ahmed, Mohamed Abdallah. Provision of study materials or patients: Fouad Jaber, Azizullah Beran, Saqr Alsakarneh, Khalid Ahmed. Collection and assembly of data: Fouad Jaber, Saqr Alsakarneh, Mohamed Abdallah, Khaled Elfert, Mohammad Almeqdadi, Mohammed Jaber. Data analysis and interpretation: Azizullah Beran, Fouad Jaber, Mohamed Abdallah, Khaled Elfert, Mohammad Almeqdadi. Manuscript writing: all authors. Final approval of manuscript: all authors.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362(9):823-832.
doi pubmed - Boike JR, Thornburg BG, Asrani SK, Fallon MB, Fortune BE, Izzy MJ, Verna EC, et al. North American practice-based recommendations for transjugular intrahepatic portosystemic shunts in portal hypertension. Clin Gastroenterol Hepatol. 2022;20(8):1636-1662.e1636.
doi pubmed pmc - Zheng M, Chen Y, Bai J, Zeng Q, You J, Jin R, Zhou X, et al. Transjugular intrahepatic portosystemic shunt versus endoscopic therapy in the secondary prophylaxis of variceal rebleeding in cirrhotic patients: meta-analysis update. J Clin Gastroenterol. 2008;42(5):507-516.
doi pubmed - Wang Q, Lv Y, Bai M, Wang Z, Liu H, He C, Niu J, et al. Eight millimetre covered TIPS does not compromise shunt function but reduces hepatic encephalopathy in preventing variceal rebleeding. J Hepatol. 2017;67(3):508-516.
doi pubmed - Lv Y, Yang Z, Liu L, Li K, He C, Wang Z, Bai W, et al. Early TIPS with covered stents versus standard treatment for acute variceal bleeding in patients with advanced cirrhosis: a randomised controlled trial. Lancet Gastroenterol Hepatol. 2019;4(8):587-598.
doi pubmed - Takase Y, Shibuya S, Chikamori F, Orii K, Iwasaki Y. Recurrence factors studied by percutaneous transhepatic portography before and after endoscopic sclerotherapy for esophageal varices. Hepatology. 1990;11(3):348-352.
doi pubmed - Smith-Laing G, Scott J, Long RG, Dick R, Sherlock S. Role of percutaneous transhepatic obliteration of varices in the management of hemorrhage from gastroesophageal varices. Gastroenterology. 1981;80(5 pt 1):1031-1036.
pubmed - Qi X, Liu L, Bai M, Chen H, Wang J, Yang Z, Han G, et al. Transjugular intrahepatic portosystemic shunt in combination with or without variceal embolization for the prevention of variceal rebleeding: a meta-analysis. J Gastroenterol Hepatol. 2014;29(4):688-696.
doi pubmed - Xiao T, Chen L, Chen W, Xu B, Long Q, Li R, Li L, et al. Comparison of transjugular intrahepatic portosystemic shunt (TIPS) alone versus TIPS combined with embolotherapy in advanced cirrhosis: a retrospective study. J Clin Gastroenterol. 2011;45(7):643-650.
doi pubmed - Chen S, Li X, Wei B, Tong H, Zhang MG, Huang ZY, Cao JW, et al. Recurrent variceal bleeding and shunt patency: prospective randomized controlled trial of transjugular intrahepatic portosystemic shunt alone or combined with coronary vein embolization. Radiology. 2013;268(3):900-906.
doi pubmed - Tesdal IK, Filser T, Weiss C, Holm E, Dueber C, Jaschke W. Transjugular intrahepatic portosystemic shunts: adjunctive embolotherapy of gastroesophageal collateral vessels in the prevention of variceal rebleeding. Radiology. 2005;236(1):360-367.
doi pubmed - Gaba RC, Bui JT, Cotler SJ, Kallwitz ER, Mengin OT, Martinez BK, Berkes JL, et al. Rebleeding rates following TIPS for variceal hemorrhage in the Viatorr era: TIPS alone versus TIPS with variceal embolization. Hepatol Int. 2010;4(4):749-756.
doi pubmed pmc - Xue H, Yuan J, Chao-Li Y, Palikhe M, Wang J, Shan-Lv L, Qiao W. Follow-up study of transjugular intrahepatic portosystemic shunt in the treatment of portal hypertension. Dig Dis Sci. 2011;56(11):3350-3356.
doi pubmed - Yu J, Wang X, Jiang M, Ma H, Zhou Z, Yang L, Li X. Comparison of transjugular intrahepatic portosystemic shunt (TIPS) alone and combined with embolisation for the management of cardiofundal varices: a retrospective study. Eur Radiol. 2019;29(2):699-706.
doi pubmed - Lakhoo J, Bui JT, Lokken RP, Ray CE, Jr., Gaba RC. Transjugular intrahepatic portosystemic shunt creation and variceal coil or plug embolization ineffectively attain gastric variceal decompression or occlusion: results of a 26-patient retrospective study. J Vasc Interv Radiol. 2016;27(7):1001-1011.
doi pubmed - Shi Y, Tian X, Hu J, Zhang J, Zhang C, Yang Y, Qin C. Efficacy of transjugular intrahepatic portosystemic shunt with adjunctive embolotherapy with cyanoacrylate for esophageal variceal bleeding. Dig Dis Sci. 2014;59(9):2325-2332.
doi pubmed - Lv Y, Chen H, Luo B, Bai W, Li K, Wang Z, Xia D, et al. Transjugular intrahepatic portosystemic shunt with or without gastro-oesophageal variceal embolisation for the prevention of variceal rebleeding: a randomised controlled trial. Lancet Gastroenterol Hepatol. 2022;7(8):736-746.
doi pubmed - Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-269.
doi pubmed - Wells GA, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12.
doi pubmed - Zheng H, et al. Transjugular intrahepatic portosystemic shunt combined with gastric coronary vein embolization in treatment of gastroesophageal varices bleeding. Chinese Journal of Interventional Imaging and Therapy. 2016;13(2):85-89.
- Wu XJ, Cao JM, Han JM, Li JS. [Long-term results of TIPS, TIPS with CVO and combined TIPS and portal azygous disconnection for the treatment of portal hypertension]. Zhonghua Wai Ke Za Zhi. 2009;47(6):446-449.
pubmed - Gaba RC, Omene BO, Podczerwinski ES, Knuttinen MG, Cotler SJ, Kallwitz ER, Berkes JL, et al. TIPS for treatment of variceal hemorrhage: clinical outcomes in 128 patients at a single institution over a 12-year period. J Vasc Interv Radiol. 2012;23(2):227-235.
doi pubmed - Wei B, Chen S, Li X, Tang CW. [Prevention of variceal rebleeding by TIPS combined with embolization of gastric coronary veins: a clinical controlled study]. Zhonghua Gan Zang Bing Za Zhi. 2011;19(7):494-497.
doi pubmed - Sanyal AJ, Freedman AM, Luketic VA, Purdum PP, 3rd, Shiffman ML, DeMeo J, Cole PE, et al. The natural history of portal hypertension after transjugular intrahepatic portosystemic shunts. Gastroenterology. 1997;112(3):889-898.
doi pubmed - Vignali C, Bargellini I, Grosso M, Passalacqua G, Maglione F, Pedrazzini F, Filauri P, et al. TIPS with expanded polytetrafluoroethylene-covered stent: results of an Italian multicenter study. AJR Am J Roentgenol. 2005;185(2):472-480.
doi pubmed - Hausegger KA, Karnel F, Georgieva B, Tauss J, Portugaller H, Deutschmann H, Berghold A. Transjugular intrahepatic portosystemic shunt creation with the Viatorr expanded polytetrafluoroethylene-covered stent-graft. J Vasc Interv Radiol. 2004;15(3):239-248.
doi pubmed - Angermayr B, Cejna M, Koenig F, Karnel F, Hackl F, Gangl A, Peck-Radosavljevic M, et al. Survival in patients undergoing transjugular intrahepatic portosystemic shunt: ePTFE-covered stentgrafts versus bare stents. Hepatology. 2003;38(4):1043-1050.
doi pubmed - Charon JP, Alaeddin FH, Pimpalwar SA, Fay DM, Olliff SP, Jackson RW, Edwards RD, et al. Results of a retrospective multicenter trial of the Viatorr expanded polytetrafluoroethylene-covered stent-graft for transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol. 2004;15(11):1219-1230.
doi pubmed - Tripathi D, Ferguson J, Barkell H, Macbeth K, Ireland H, Redhead DN, Hayes PC. Improved clinical outcome with transjugular intrahepatic portosystemic stent-shunt utilizing polytetrafluoroethylene-covered stents. Eur J Gastroenterol Hepatol. 2006;18(3):225-232.
doi pubmed - Burroughs AK, Triantos CK, O'Beirne J, Patch D. Predictors of early rebleeding and mortality after acute variceal hemorrhage in patients with cirrhosis. Nat Clin Pract Gastroenterol Hepatol. 2009;6(2):72-73.
doi pubmed - Wang L, Xiao Z, Yue Z, Zhao H, Fan Z, Zhao M, He F, et al. Efficacy of covered and bare stent in TIPS for cirrhotic portal hypertension: A single-center randomized trial. Sci Rep. 2016;6:21011.
doi pubmed pmc - He C, Lv Y, Wang Z, Guo W, Tie J, Li K, Niu J, et al. Association between non-variceal spontaneous portosystemic shunt and outcomes after TIPS in cirrhosis. Dig Liver Dis. 2018;50(12):1315-1323.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


