| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 17, Number 4, August 2024, pages 151-158
Pre-Cut Papillotomy Versus Endoscopic Ultrasound-Rendezvous for Difficult Biliary Cannulation: A Systematic Review and Meta-Analysis
Amna Iqbala, i , Zohaib Ahmadb, Muhammad Azizc, Abdulmajeed Alharbia, Hassam Alid, Ahmed Al-Chalabie, Manesh Kumar Gangwania, Dushyant Singh Dahiyaf, Wade Lee Smithg, Shailendra Singhh, Yaseen Alastalb, Abdallah Kobeissyb
aDepartment of Internal Medicine, University of Toledo, Toledo, OH, USA
bDepartment of Gastroenterology and Hepatology, University of Toledo, Toledo, OH, USA
cDivision of Gastroenterology, Bon Secours Mercy Health, Toledo, OH, USA
dDepartment of Gastroenterology and Hepatology, ECU Health Medical Center, Greenville, NC, USA
eDepartment of Gastroenterology, Creighton University, Omaha, NE, USA
fDivision of Gastroenterology, Hepatology and Motility, The University of Kansas School of Medicine, Kansas City, KS, USA
gUniversity of Toledo Libraries, Toledo, OH, USA
hDepartment of Gastroenterology and Hepatology, West Virginia University, Morgantown, WV, USA
iCorresponding Author: Amna Iqbal, Department of Internal Medicine, University of Toledo, OH, USA
Manuscript submitted May 3, 2024, accepted June 28, 2024, published online July 18, 2024
Short title: Pre-Cut Papillotomy Versus EUS-Rendezvous
doi: https://doi.org/10.14740/gr1738
| Abstract | ▴Top |
Background: Various endoscopic techniques are employed to achieve biliary cannulation when confronted with difficult biliary access. Every procedure carries its own risk in terms of bleeding, infection, pancreatitis, and cholangitis. Our meta-analysis aimed to compare pre-cut papillotomy and endoscopic ultrasound (EUS)-rendezvous in terms of technical success rates, and post-procedure pancreatitis and bleeding.
Methods: We conducted a systematic review and meta-analysis of studies that compared pre-cut papillotomy and EUS-rendezvous. The primary outcome was technical success by achieving biliary cannulation. Secondary outcomes were postoperative pancreatitis and bleeding. A random-effects model was used to calculate the risk ratios (RRs) and confidence intervals (CIs). A P value < 0.05 was considered statistically significant.
Results: Our meta-analysis included four studies comparing pre-cut papillotomy and EUS-rendezvous. The studies included 13,659 total endoscopic retrograde cholangiopancreatography (ERCP) procedures, of whom 1,004 patients underwent alternate biliary cannulation procedures due to difficult biliary cannulation. The mean age of the study population was noted to be 49.5 years and males represented 53.3% of the total participants. Both procedures were similar in terms of technical success (RR: 0.95, 95% CI (0.88, 1.02)). No difference was found between rates of post procedure pancreatitis (RR: 1.82, 95% CI (0.80, 4.15)) and post procedure bleeding (RR: 2.80, 95% CI (0.67, 11.66)).
Conclusions: There was no difference in technical success of procedure or post-procedure complications such as pancreatitis and bleeding between pre-cut papillotomy and EUS-rendezvous technique. More randomized controlled trials (RCTs) are needed to compare both procedural techniques and complications rates. However, currently, both procedures are equally effective and safe during difficult biliary cannulation in the hands of experienced endoscopists.
Keywords: Difficult biliary cannulation; Endoscopic ultrasound; Pre-cut papillotomy; EUS-rendezvous; Endoscopic retrograde cholangiopancreatography
| Introduction | ▴Top |
Endoscopic retrograde cholangiopancreatography (ERCP) is a commonly employed therapeutic procedure for hepatobiliary and pancreatic diseases [1]. Common indications for ERCP include obstructive jaundice, management or tissue sampling of biliary or pancreatic ductal system disease, investigation of pancreatic cancer, pancreatitis of unknown cause, biliary stenting for strictures and leakage, drainage of pancreatic pseudocysts, and balloon dilation of the duodenal papilla and ductal strictures, amongst others [2]. The American Society of Gastrointestinal Endoscopy (ASGE) recommends a rate of more than 80% for successful biliary cannulation by all endoscopists performing ERCP [3]. Differing rates of successful biliary cannulation are reported at various centers across the USA, with as high as 90% at high-volume tertiary centers with experienced endoscopists; however, failure rates are still high ranging from 5% to 10% with initial ERCP [4, 5].
Numerous factors may predict the failure of ERCP. Lobo et al found that the frequency of periampullary diverticula increases significantly in patients over 75 years of age, and the cannulation success rates decreases significantly due to the presence of periampullary diverticula with this increasing age [6]. Several other factors have also been recognized that affect biliary cannulation including duodenal diverticulum, adhesions due to prior abdominal surgeries, gastrointestinal diversions, and periampullary tumors [7].
Several techniques are used to achieve selective biliary cannulation, the most common being wire-guided cannulation technique [8]. Multiple and prolonged attempts at biliary cannulation increase risk for post-procedure pancreatitis [9]. In recent years, the European Society of Gastrointestinal Endoscopy (ESGE) has defined difficult biliary cannulation (DBC) as one of the following: more than five contacts with papilla when trying to cannulate, more than 5 min spent to cannulate after visualization of papilla, or more than one inadvertent cannulation or opacification of pancreatic duct [10, 11]. When selective biliary cannulation becomes difficult to achieve, several techniques can be employed to achieve cannulation. These include double guidewire cannulation, pre-cut papillotomy, pancreatic sphincterotomy, EUS-rendezvous and percutaneous transhepatic biliary drainage (PTBD) [12].
Pre-cut papillotomy involves the utilization of a pre-cut papillotome to slit open or unroof the papilla to expose the opening of distal common bile duct (CBD) [13]. Endoscopic ultrasound-guided biliary drainage (EUS-BD) may be categorized according to access method and the route of drainage. The bile duct may be accessed by either the intrahepatic or extrahepatic portions, typically with a 19- or 22-gauge fine needle aspiration (FNA) needle [14]. Intrahepatic access may be transgastric, transesophageal, or transjejunal (in surgically altered anatomy) with the typical initial puncture into the left hepatic lobe. Extrahepatic access is usually transduodenal and progresses into the CBD. Once accessed, biliary drainage methods include direct transmural or transluminal drainage, antegrade transpapillary placement of a biliary stent, or guide wire rendezvous with a duodenoscope allowing subsequent conventional ERCP management, known as endoscopic ultrasound (EUS)-guided rendezvous (EUS-RV).
Numerous clinical trials and multicentric studies have been reported highlighting the success rate of various techniques for successful biliary cannulation, but no definitive guidelines or algorithm is available for interventional gastroenterologists to employ when faced with DBC. We aimed to compare pre-cut papillotomy and EUS-RV, the two techniques which are becoming increasingly popular as methods for successful biliary access.
| Materials and Methods | ▴Top |
Search strategy
A comprehensive search strategy to identify reports of EUS-rendezvous after a failed ERCP was constructed in Embase (Elsevier) by an experienced health sciences librarian (WLS) using truncated keywords, phrases, proximity searching and subject headings. This strategy was translated to MEDLINE (PubMed platform, National Center for Biotechnology Information, National Library of Medicine), Cochrane Central Register of Controlled Trials (Wiley), and the Web of Science Core Collection (Web of Science platform, Clarivate) with all searches performed on October 1, 2023 (Supplementary Material 1, www.gastrores.org). No publication date or language limits were used. All results were exported to EndNote 20 citation management software (Clarivate, Philadelphia, PA, USA) and duplicates were removed by successive iterations of EndNote’s duplicate detection algorithms and manual inspection (Supplementary Material 1, www.gastrores.org).
The search strategy was created by an experienced librarian (WLS) and reviewed by another investigator (ZA). Detailed search strategy for Embase is provided here (Supplementary Material 1, www.gastrores.org). Screening of the articles was performed by two independent reviewers (AI and ZA), and discrepancy was resolved through mutual discussion. Preliminary screening was done using title and abstracts, and full texts of relevant articles were obtained. Bibliographies of the articles included were also checked to see if any additional articles fulfilled our study criteria. We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and no restriction to language was applied (Fig. 1) [15].
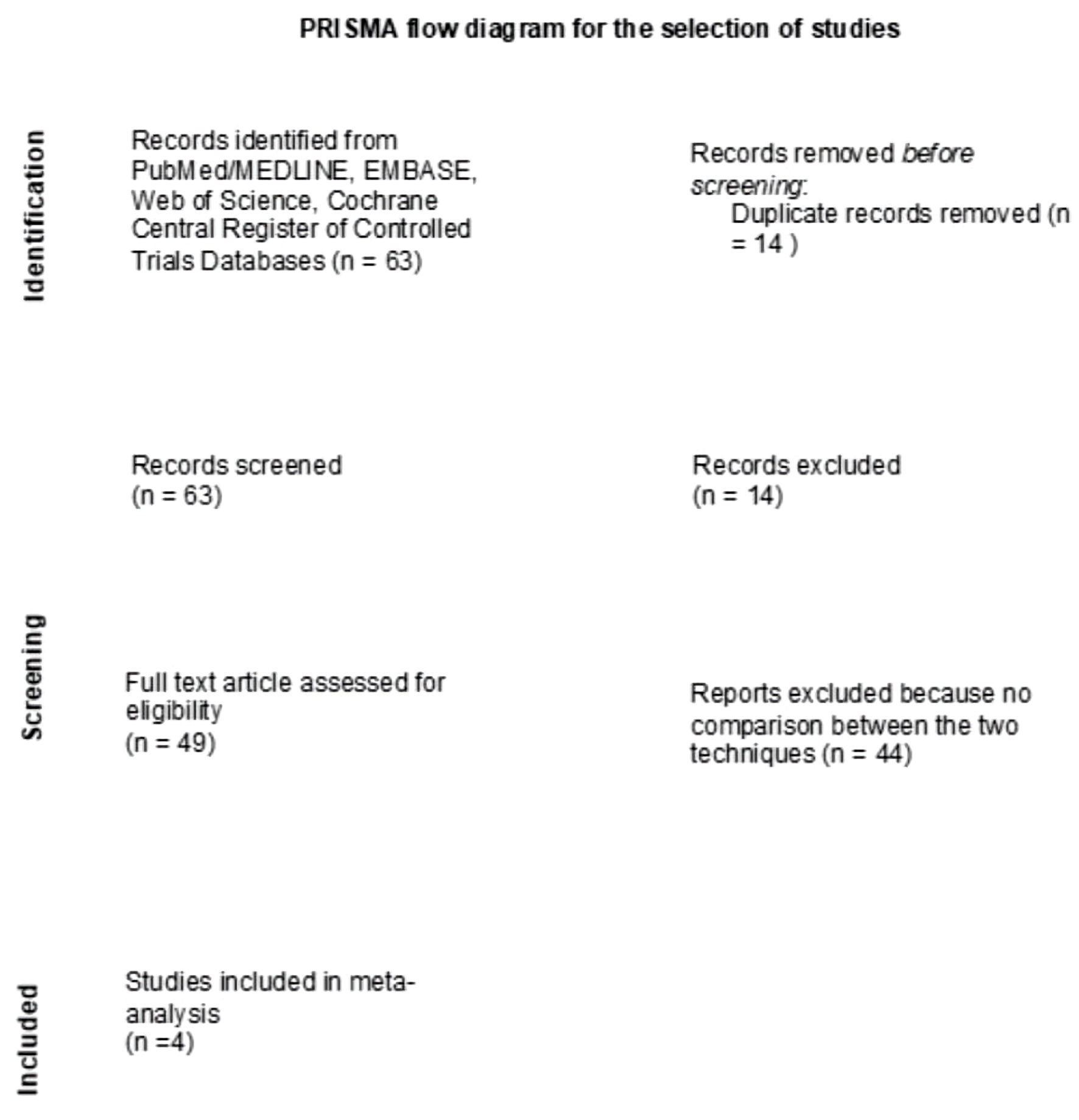 Click for large image | Figure 1. The PRISMA flow chart illustrating how the final studies were selected. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses. |
Inclusion and exclusion criteria
We included full studies and abstracts that met the following criteria: 1) Randomized controlled trials (RCTs); 2) Prospective or retrospective cohort studies, which compared pre-cut papillotomy and EUS-rendezvous to each other and reported outcomes of interest. Case reports and literature reviews were excluded. We included all pre-cut techniques for our meta-analysis including pre-cutting performed with pre-cut papillotome, pre-cut sphincterotome and pre-cut fistulotomy. No studies reported any impact of individual pre-cut techniques on procedure success rate and adverse effect profile of any specific pre-cut technique. We included all studies comparing pre-cut papillotomy and EUS-RV, for all included studies both procedures were fully performed. Outcomes of interest included technical success rate between pre-cut papillotomy and EUS-RV, and rates of post-procedure pancreatitis and bleeding between the two groups.
Data extraction and study outcomes
The following data were extracted from the studies: author name, publication year, country of origin, study design, gender, and age of patients, total ERCP procedures, total pre-cut papillotomies, and total EUS-rendezvous procedures. Outcome measures were retrieved, including rates of overall procedure success and post-procedure pancreatitis and bleeding. Data were collected and tabulated on Microsoft Excel (Microsoft, Redmond, Wash, USA) by two independent reviewers (AI and ZA). Any discrepancy in data collection was resolved through mutual discussion and third reviewer (AK).
Data synthesis and statistical analysis
The meta-analysis was performed using Review Manager 5.4 (Cochrane Collaboration, Copenhagen, The Nordic Cochrane Center). A random-effects model was used to calculate the weighted pooled risk ratios (RRs), and 95% confidence intervals (CIs) of our desired outcomes. A P value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index, where I2 values > 50% implied the presence of substantial heterogeneity [16].
Bias assessment
The bias assessment for included studies was evaluated using Newcastle-Ottawa scale for observational studies [17]. The Cochrane risk-of-bias tool was used to assess bias in included RCTs subjectively [18]. Publication bias was visually assessed using funnel plots as well as quantitatively assessed using Egger’s regression analysis. A P value < 0.05 was indicative of substantial publication bias.
The ethics approval and declaration of human ethics do not apply to our study.
| Results | ▴Top |
Study selection
Using the search strategy above, a total of 63 studies were screened, duplicates were removed, and ultimately four studies were included in the final analysis (Fig. 1). All included studies were observational studies. A total of 1,004 patients were included which also corresponded to the total number of pre-cut papillotomy and EUS-RV procedures.
Study characteristics
Table 1 [19-22] shows the characteristics of the four studies included in our meta-analysis [19-22]. Table 2 [19-22] demonstrates ERCP indications in the population. The studies included 13,659 total ERCP procedures, of whom 1,004 patients underwent alternate biliary cannulation procedures due to DBC. Of the included studies, three were retrospective cohort, and one was prospective cohort. Furthermore, two studies were full-text publications, and two were abstracts. The mean age of the study population was noted to be 49.5 years, and males represented 53.3% of the total participants.
 Click to view | Table 1. Baseline Study Characteristics and Demographics |
 Click to view | Table 2. ERCP Indications |
Direct meta-analysis
Outcomes for individual studies are summarized in Table 3 [19-22]. Figure 2 demonstrates the forest plot that compares technical success of procedure, post-procedure pancreatitis and post-procedure bleeding between pre-cut papillotomy and EUS-RV. We found no statistical difference between the two procedures in terms of technical success rates (RR: 0.95, CI: 0.88 - 1.02, P = 0.14, I2 = 71%) (Fig. 2a). Furthermore, the rates of post-procedure pancreatitis (RR: 1.82, CI: 0.80 - 4.15, P = 0.15, I2 = 0%) (Fig. 2b), post-procedure bleeding (RR: 2.80, CI: 0.67 - 11.66, P = 0.16, I2 = 0%) (Fig. 2c) and overall complications were similar for both procedures (RR: 0.87, CI: 0.23 - 3.26, P = 0.84, I2 = 89%) (Fig. 2d).
 Click to view | Table 3. Outcomes for Individual Studies |
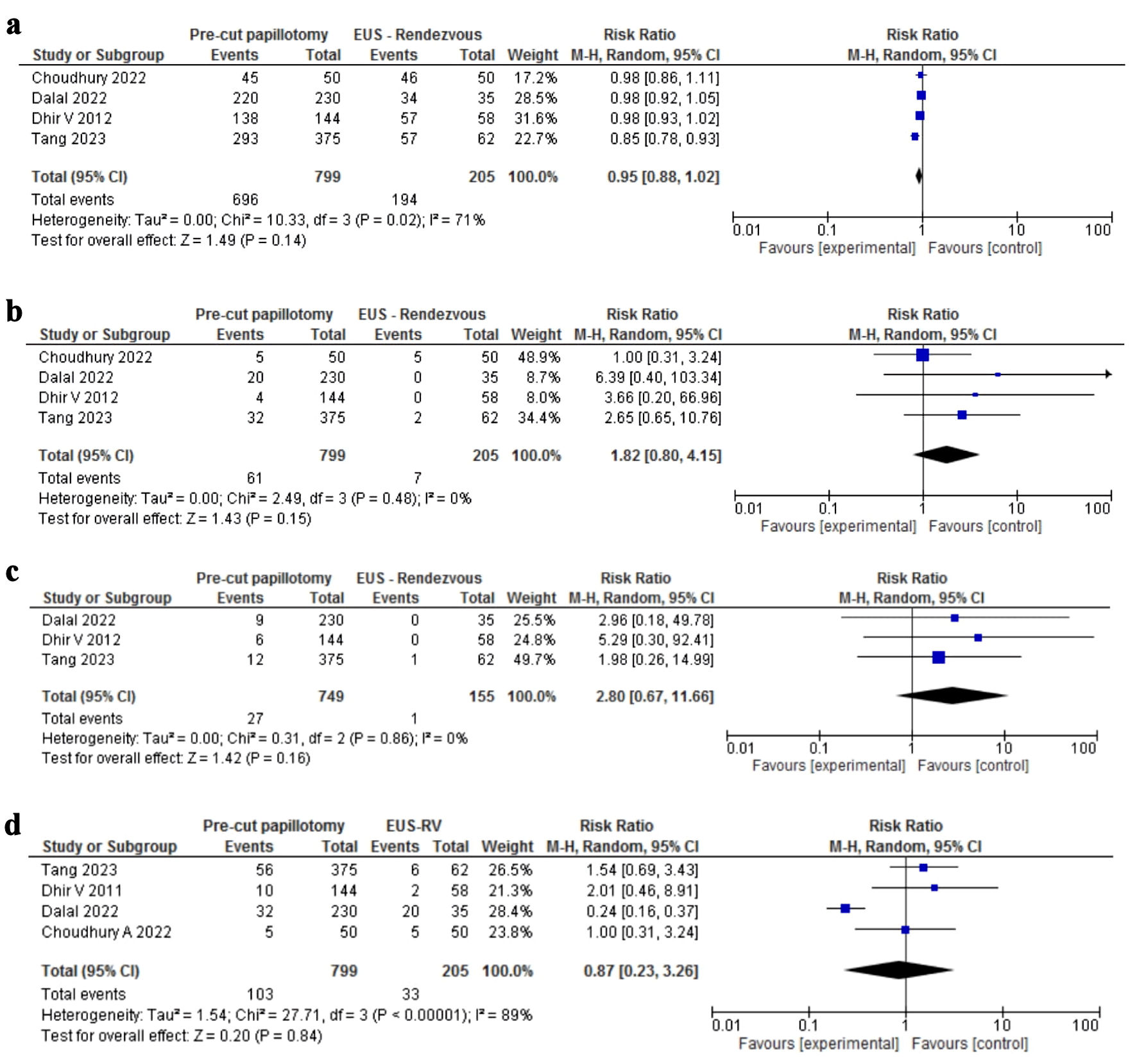 Click for large image | Figure 2. Forrest plot results of meta-analysis. (a) Forrest plot comparing technical success rate of pre-cut papillotomy and EUS-rendezvous. (b) Forrest plot comparing post-procedure pancreatitis rate between pre-cut papillotomy and EUS-rendezvous. (c) Forrest plot comparing bleeding rate between pre-cut papillotomy and EUS-rendezvous. (d) Forrest plot comparing overall complications rate between pre-cut papillotomy and EUS-rendezvous. |
Bias assessment
Bias assessment of included observational studies using Newcastle-Ottawa scale showed a score of 6 - 8 for all studies (Supplementary Material 2, www.gastrores.org). The publication bias was difficult to assess both qualitatively and quantitatively due to lack of adequate number of studies.
| Discussion | ▴Top |
To our knowledge, this is the first systematic review and meta-analysis performed comparing pre-cut papillotomy and EUS-RV technique. Our results demonstrated that there was no difference in the technical success rates for both procedures. Additionally, we noted no difference in the rates of post-procedure pancreatitis and bleeding for both techniques, highlighting a similar safety profile.
Angsuwatcharakon et al report a successful biliary cannulation rate of 81% with pre-cut sphincterotomy [23]. Recent publications suggest that pre-cut sphincterotomy is an independent risk factor for adverse events including post-procedure pancreatitis, bleeding, and cholangitis [24]. However, the high rates of adverse events may be due to the fact that the technique is a last resort after multiple failed attempts of cannulation [25]. Cennamo et al denoted in their recent meta-analysis that early implementation of pre-cut and persistent cannulation attempts have similar overall cannulation rates, but early pre-cut implementation reduces the rate of post-ERCP pancreatitis compared to persistent attempts at cannulation (odds ratio (OR): 0.47; 95 % CI: 0.24 - 0.91) [26]. Although pre-cut papillotomy is a safe and effective option for DBC, the complication rate is relatively higher when compared to standard papillotomy as demonstrated in the prospective study by Figueiredo et al, but this increase in the complication rate is acceptable as the procedure also increases the rate of biliary cannulation by up to 25% [27].
With the increasing popularity and availability of EUS, EUS-RV is being employed increasingly at high-volume tertiary healthcare centers as an alternate technique for DBC [28]. Maranki et al reported that cholangiography was successful in 84% of 49 cases of EUS-guided cholangiography and that EUS-RV was successful in 65%, concluding that EUS-guided cholangiography is a feasible alternative to percutaneous transhepatic cholangiography in patients with obstructive jaundice for whom ERCP has failed [29]. Dhir et al compared the transhepatic (TH) and extrahepatic (EH) route for EUS-rendezvous technique and found no difference in the technical success rates (94.1% vs. 100%) between the two. However, the TH route had a higher incidence of post-procedure pain (44.1% vs. 5.5%; P = 0.017), and a significantly longer length of hospital stay (2.52 vs. 0.17 days; P = 0.015) [30]. Iwashita et al [31] reported that puncture via the second part of the duodenum (D2) using a short position is the first-line transduodenal route for extrahepatic route of the EUS-rendezvous technique. Their results show that access to the extrahepatic biliary drainage (EHBD) from the D2 was possible only in 50% of the patients (10/20) with a EUS-RV; however, the success rate was a 100% in all these attempts. In the remaining 10 patients, the biliary duct was accessed from the D1 via the EHBD (five patients) or from the stomach via the intrahepatic biliary drainage (IHBD) (four patients). The success rate of EUS-RV attempts for these access sites was noted be 66.7% (6/9) [31]. One of the distinct advantages of EUS-RV is reduction in pancreatitis rate [32]. Two studies [21, 22] reported pancreatitis as one of the adverse effects for both procedures. Few reasons for pancreatitis cases with EUS-RV in both studies include crossover to pre-cut papillotomy group after EUS failure and previous selective cannulation attempts. EUS-RV does involve extra expertise in the procedure and also involves additional resources due to the fact that it is not a single working channel and needs biliary access first, then guidewire manipulation and finally exchanging the echoendoscope with duodenoscope. This is one of the major considerations when employing this technique and requires experienced endoscopists. Studies included in our meta-analysis did not differentiate based on EUS-RV technique. This is one of the potential areas of study for the future.
The studies included in our meta-analysis were observational studies and as shown in Table 2 [19-22], there were different indications and protocols for both procedures. In the retrospective study of Dhir et al (2011) [19], all patients underwent EUS-RV and were compared with comparative cohort of pre-cut papillotomy patients. DBC patients with difficult to locate papilla/tumor underwent EUS-RV in the study by Dalal et al (2022) [20]. In the study by Choudhury et al (2022) [21], patients were randomized into both groups, patients with failure in either group were crossed over to the other group. In the study by Tang et al (2023) [22], all patients had naive papilla, patients with inaccessible papilla were excluded. There is a possibility of beta error in adverse effect profile for both procedures (Fig. 2b, c) as the studies involved cross-over of patients, previous attempts at cannulation.
There is currently no standardized algorithm for endoscopic techniques for DBC. Complex decision making and careful personalized patient selection by experienced therapeutic endoscopists can lead to high success rates of selective biliary cannulation with both pre-cut papillotomy and EUS-rendezvous technique.
We do acknowledge all the limitations associated with our study. First, the sample size is small with only 1,004 patients. Second, No RCTs were available comparing pre-cut papillotomy to EUS-RV procedure, and our results were based on observational studies with their inherent bias. Hence, we advocate for the need for high-quality RCTs comparing both techniques in terms of their efficacy, risks, and complications. Third, due to the low number of full studies we included abstracts that are limited in terms of methodology assessment. Fourth, the experience of endoscopists cannot be disregarded. Lastly, the procedures were performed in high volume tertiary centers, limiting generalizability. However, despite these limitations we performed a robust systematic review with stringent inclusion and exclusion criteria.
Conclusions
Our meta-analysis is the first to compare pre-cut papillotomy to EUS-rendezvous technique for DBC. We noted no statistical difference in the technical success rates, post-procedure pancreatitis and post-procedure bleeding between the two endoscopic techniques. Hence, both procedures are equally safe and effective for DBC in the hands of experienced therapeutic endoscopists. High quality RCTs are needed to further compare both procedural techniques.
Learning points
Various techniques are employed by interventional endoscopists when facing DBC based on technical skills and expertise of each endoscopist.
There is no standardized algorithm for interventional endoscopists for DBC. Our study found no difference in terms of technical success rates, post-procedure pancreatitis and post-procedure bleeding between EUS-rendezvous and pre-cut papillotomy techniques.
More robust RCTs are needed to further recommend guidelines or direct workflow for endoscopists. Future considerations include comparing safety and efficacy of various pre-cut and EUS-RV techniques in large RCTs.
| Supplementary Material | ▴Top |
Suppl 1. Full search strategies.
Suppl 2. Newcastle-Ottawa scale.
Acknowledgments
We are grateful to all of those with whom we have had the pleasure to work on this project.
Financial Disclosure
No funding was received for the preparation of this manuscript.
Conflict of Interest
No conflict of interests to report.
Informed Consent
This does not apply to our study.
Author Contributions
Three authors (AI, ZA, MKG) conceptualized the study. Authors (AI, MA, HA, DSD, AK) wrote and proofread the manuscript. Authors (AI, WLS, AA, AC) developed search study. Authors (AI, MA, SS) performed statistical analysis. Authors (AI, YA, SS) proofread the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article. Supplementary data are included in the manuscript. No other supporting data are available.
| References | ▴Top |
- Sanders DJ, Bomman S, Krishnamoorthi R, Kozarek RA. Endoscopic retrograde cholangiopancreatography: Current practice and future research. World J Gastrointest Endosc. 2021;13(8):260-274.
doi pubmed pmc - Meseeha M, Attia M. Endoscopic retrograde cholangiopancreatography. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, Hoffman B, et al. Quality indicators for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc. 2006;63(4 Suppl):S29-S34.
doi pubmed - Ramirez FC, Dennert B, Sanowski RA. Success of repeat ERCP by the same endoscopist. Gastrointest Endosc. 1999;49(1):58-61.
doi pubmed - Schlup MM, Williams SM, Barbezat GO. ERCP: a review of technical competency and workload in a small unit. Gastrointest Endosc. 1997;46(1):48-52.
doi pubmed - Lobo DN, Balfour TW, Iftikhar SY. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl. 1998;80(5):326-331.
pubmed pmc - Balik E, Eren T, Keskin M, Ziyade S, Bulut T, Buyukuncu Y, Yamaner S. Parameters that may be used for predicting failure during endoscopic retrograde cholangiopancreatography. J Oncol. 2013;2013:201681.
doi pubmed pmc - Aziz M, Iqbal A, Ahmed Z, Saleem S, Lee-Smith W, Goyal H, Kamal F, et al. Impact of guidewire caliber on ERCP outcomes: Systematic review and meta-analysis comparing 0.025- and 0.035-inch guidewires. Endosc Int Open. 2022;10(7):E990-E997.
doi pubmed pmc - Ribeiro IB, do Monte Junior ES, Miranda Neto AA, Proenca IM, de Moura DTH, Minata MK, Ide E, et al. Pancreatitis after endoscopic retrograde cholangiopancreatography: A narrative review. World J Gastroenterol. 2021;27(20):2495-2506.
doi pubmed pmc - Lee YS, Cho CM, Cho KB, Heo J, Jung MK, Kim SB, Kim KH, et al. Difficult Biliary Cannulation from the Perspective of Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis: Identifying the Optimal Timing for the Rescue Cannulation Technique. Gut Liver. 2021;15(3):459-465.
doi pubmed pmc - Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Deviere J, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(7):657-683.
doi pubmed - Chen Q, Jin P, Ji X, Du H, Lu J. Management of difficult or failed biliary access in initial ERCP: A review of current literature. Clin Res Hepatol Gastroenterol. 2019;43(4):365-372.
doi pubmed - Shakoor T, Geenen JE. Pre-cut papillotomy. Gastrointest Endosc. 1992;38(5):623-627.
doi pubmed - Tang Z, Igbinomwanhia E, Elhanafi S, Othman MO. Endoscopic Ultrasound Guided Rendezvous Drainage of Biliary Obstruction Using a New Flexible 19-Gauge Fine Needle Aspiration Needle. Diagn Ther Endosc. 2016;2016:3125962.
doi pubmed pmc - Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
doi pubmed pmc - Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560.
doi pubmed pmc - Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7(27).
doi pubmed - Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
doi pubmed pmc - Dhir V, Bhandari S, Bapat M, Maydeo A. Comparison of EUS-guided rendezvous and precut papillotomy techniques for biliary access (with videos). Gastrointest Endosc. 2012;75(2):354-359.
doi pubmed - Dalal A, Gandhi C, Patil G, Kamat N, Vora S, Maydeo A. Safety and efficacy of different techniques in difficult biliary cannulation at endoscopic retrograde cholangiopancreatography. Hosp Pract (1995). 2022;50(1):61-67.
doi pubmed - Choudhury A, Samanta J, Muktesh G, Dhar J, Kumar A, Shah J, Gupta P, et al. EUS- guided rendezvous technique versus precut papillotomy as salvage technique in patients of benign biliary disease with difficult biliary cannulation: a randomized controlled trial. Endoscopy. 2022;54(S 01):S6.
doi - Tang R, Chan TT, Lo V, Lao BC, Chew M, Chan S, Teoh A, et al. EUS-guided rendezvous vs precut papillotomy in patients with difficult biliary access in ercp for benign and malignant conditions. Gastrointestinal Endoscopy. 2023;97(6 Supplement):AB838.
doi - Angsuwatcharakon P, Rerknimitr R, Ridtitid W, Ponauthai Y, Kullavanijaya P. Success rate and cannulation time between precut sphincterotomy and double-guidewire technique in truly difficult biliary cannulation. J Gastroenterol Hepatol. 2012;27(2):356-361.
doi pubmed - Testoni PA, Testoni S, Giussani A. Difficult biliary cannulation during ERCP: how to facilitate biliary access and minimize the risk of post-ERCP pancreatitis. Dig Liver Dis. 2011;43(8):596-603.
doi pubmed - Lopes L, Dinis-Ribeiro M, Rolanda C. Early precut fistulotomy for biliary access: time to change the paradigm of "the later, the better"? Gastrointest Endosc. 2014;80(4):634-641.
doi pubmed - Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, et al. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy. 2010;42(5):381-388.
doi pubmed - Figueiredo FA, Pelosi AD, Machado L, Francioni E, Freitas G, Hatum PB, de Mello Perez R. Precut papillotomy: a risky technique not only for experts but also for average endoscopists skilled in ERCP. Dig Dis Sci. 2010;55(5):1485-1489.
doi pubmed - Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: Report of 6 cases. Gastrointest Endosc. 2004;59(1):100-107.
doi pubmed - Maranki J, Hernandez AJ, Arslan B, Jaffan AA, Angle JF, Shami VM, Kahaleh M. Interventional endoscopic ultrasound-guided cholangiography: long-term experience of an emerging alternative to percutaneous transhepatic cholangiography. Endoscopy. 2009;41(6):532-538.
doi pubmed - Dhir V, Bhandari S, Bapat M, Joshi N, Vivekanandarajah S, Maydeo A. Comparison of transhepatic and extrahepatic routes for EUS-guided rendezvous procedure for distal CBD obstruction. United European Gastroenterol J. 2013;1(2):103-108.
doi pubmed pmc - Iwashita T, Yasuda I, Mukai T, Iwata K, Ando N, Doi S, Nakashima M, et al. EUS-guided rendezvous for difficult biliary cannulation using a standardized algorithm: a multicenter prospective pilot study (with videos). Gastrointest Endosc. 2016;83(2):394-400.
doi pubmed - Swahn F, Regner S, Enochsson L, Lundell L, Permert J, Nilsson M, Thorlacius H, et al. Endoscopic retrograde cholangiopancreatography with rendezvous cannulation reduces pancreatic injury. World J Gastroenterol. 2013;19(36):6026-6034.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


