| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 5, October 2022, pages 253-262
Rates, Reasons, and Independent Predictors of Readmissions in Portal Venous Thrombosis Hospitalizations in the USA
Robert Kwei-Nsoroa, h, Pius Ojemolona, Hisham Laswia, Ebehiwele Ebhohonb, Abdultawab Shakac, Wasey Ali Mird, Abdul Hassan Siddiquie, Jobin Philiposef, Hafeez Shakag
aDepartment of Internal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, USA
bDepartment of Internal Medicine, Lincoln Medical Center, Bronx, NY, USA
cDepartment of Medicine, Windsor University School of Medicine, St. Kitts
dDepartment of Pulmonary and Critical Care, St. Elizabeth Medical Center, Brighton, MA, USA
eDepartment of Pulmonary and Critical Care, St. Joseph Hospital, London, KY, USA
fDepartment of Digestive Health, Mountain View Regional Medical Center, Las Cruces, NM, USA
gDivision of General Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, USA
hCorresponding Author: Robert Kwei-Nsoro, Department of Internal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL 60612, USA
Manuscript submitted August 5, 2022, accepted September 9, 2022, published online October 19, 2022
Short title: PVT Hospitalizations in the USA
doi: https://doi.org/10.14740/gr1561
| Abstract | ▴Top |
Background: Portal vein thrombosis (PVT), generally considered rare, is becoming increasingly recognized with advanced imaging. Limited data exist regarding readmissions in PVT and its burden on the overall healthcare cost. This study aimed to outline the burden of PVT readmissions and identify the modifiable predictors of readmissions.
Methods: The National Readmission Database (NRD) was used to identify PVT admissions from 2016 to 2019. Using the patient demographic and hospital-specific variables within the NRD, we grouped patient encounters into two cohorts, 30- and 90-day readmission cohorts. We assessed comorbidities using the validated Elixhauser comorbidity index. We obtained inpatient mortality rates, mean length of hospital stay (LOS), total hospital cost (THC), and causes of readmissions in both 30- and 90-day readmission cohorts. Using a multivariate Cox regression analysis, we identified the independent predictors of 30-day readmissions.
Results: We identified 17,971 unique index hospitalizations, of which 2,971 (16.5%) were readmitted within 30 days. The top five causes of readmissions in both 30-day and 90-day readmission cohorts were PVT, sepsis, hepatocellular cancer, liver failure, and alcoholic liver cirrhosis. The following independent predictors of 30-day readmission were identified: discharge against medical advice (AMA) (adjusted hazard ratio (aHR) 1.86; P = 0.002); renal failure (aHR 1.44, P = 0.014), metastatic cancer (aHR 1.31, P = 0.016), fluid and electrolyte disorders (aHR 1.20, P = 0.004), diabetes mellitus (aHR 1.31, P = 0.001) and alcohol abuse (aHR 1.31, P ≤ 0.001).
Conclusion: The readmission rate identified in this study was higher than the national average and targeted interventions addressing these factors may help reduce the overall health care costs.
Keywords: Portal vein thrombosis; Readmissions; Healthcare expenditure; Outcomes
| Introduction | ▴Top |
Portal vein thrombosis (PVT), generally considered rare in developed countries, is becoming increasingly recognized [1]. Reliable data on incidence and prevalence are lacking, and autopsy studies have reported a population prevalence of 1%; however, this increases to 24% in patients with liver cirrhosis. [2, 3]. The etiology of PVT is diverse, often with multiple concurrent factors [1, 4, 5]. Cirrhosis, hepatocellular carcinoma (HCC), and intra-abdominal infections remain the most common local predisposing factors [1, 4]. Myeloproliferative disorders, inherited and acquired thrombophilia are important systemic predisposing factors. The development of PVT is often insidious and is usually an incidental diagnosis in patients with cirrhosis [4, 5]. Anticoagulation is the cornerstone of treatment; however, the decision to initiate anticoagulation depends on the nature of the clot, the presence of predisposing conditions, and the patient’s comorbidities [6]. The Center for Medicare and Medicaid services labeled 30-day readmission rates as an indicator of healthcare quality and emphasized its reduction as a strategy to reduce healthcare costs while maintaining quality [7]. Readmissions have huge impacts on the overall cost of healthcare, and repeated hospitalization is harmful to patients and constitutes a burden to caregivers and healthcare systems [8]. The overall healthcare cost specific to PVT is unknown; however, costs for venous thromboembolism (VTE) are considerable and increasing faster than general inflation for medical care services with the cost of hospitalization being the primary cost driver [9]. Readmissions for VTE are generally more costly than the initial VTE admission [9]. Understanding and assessing the national trends in PVT readmissions would provide the keys to success for any given intervention intending to reduce readmission rates and healthcare costs in these patients.
| Materials and Methods | ▴Top |
This was an observational retrospective study involving adults hospitalized for PVT in the USA from 2016 to 2019. We used data from the Nationwide Readmissions Database (NRD) for 2016, 2017, 2018, and 2019. The NRD is the largest publicly available all-payer inpatient healthcare readmission database in the USA, drawn from the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SID) containing verified patient linkage numbers that can be used to track a person across hospitals within a State, while adhering to strict privacy guidelines [10]. The NRD is an annual file constructed using one calendar year of discharge data. The NRD 2019 contains discharge data from 30 geographically dispersed states accounting for 59.7% of the total USA resident population and 61.9% of all USA hospitalizations. It comprises both patient- and hospital-level information. Up to 40 discharge diagnoses and 25 procedures are collected for each patient using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD10-CM/PCS). Diagnoses are classified as principal diagnosis, which is the reason for hospitalization, and secondary diagnosis which is any other discharge diagnosis. Hospitals are stratified according to ownership control, the number of beds, teaching status, urban/rural location, and geographic region. The NRD allows for weighted analysis to obtain 100% of the USA hospitalizations within a given year [11]. This manuscript conforms with the STROBE statement for reporting observational studies. The study involved hospitalizations with a principal diagnosis of PVT using ICD-10 codes (Code 181). We excluded hospitalizations involving patients less than 18 years old and elective hospitalizations as well as December hospitalizations for each year due to the lack of an adjoining 30-day period to assess 30-day readmission. To assess the 90-day readmission data, we excluded October through December hospitalizations for each year due to the lack of an adjoining 90-day period to assess 90-day readmission. For each patient, the first hospitalization for PVT within the year was marked as the index admission. Using the index admission and unique hospitalization identifiers available in the NRD, we identified one subsequent hospitalization within 30 and 90 days. This was tagged as readmission. The NRD contains variables on patient demographics, including age, sex, median household income (MHOI) by zip code (income quartiles referred to patients as 1 - low income, 2 - middle income, 3 - upper middle income, 4 - high income), and primary payer. It also contains hospital-specific variables including bed size, teaching status, and location. We assessed the comorbidity burden using the AHRQ Elixhauser comorbidity index (ECI) which is validated for HCUP database analysis as a measure of the comorbidity burden in a sample. We listed the Elixhauser 31 comorbidities and obtained a grouped ECI. The ECI incorporates the influence of comorbid conditions in models designed to assess the risk of in-hospital mortality and readmission using administrative data with limited clinical information, especially when small sample sizes are an issue [12]. This method has been well validated in database research on other medical conditions [13, 14]. The ECI has been shown to be superior to Deyo’s modification of the Charlson comorbidity index (CCI) as an overall measure of comorbid burden and healthcare cost utilization [12, 15, 16]. We compared the demographic data of PVT hospitalizations and readmissions. Outcomes included the top 10 reasons for 30-day and 90-day all-cause readmissions (ACRs), and rates of 30 ACR and 90 ACR following index hospitalization for PVT. Other outcomes included assessment of index and readmission mortality, mean length of hospital stay (LOS), total hospital cost (THC), and independent predictors of 30 ACR. We obtained the hospital cost for each admission using the HCUP cost-to-charge ratio files and adjusted for inflation using the Medical Expenditure Panel Survey index for hospital care, with 2019 as the reference point [17, 18]. We analyzed the data using Stata® Version 16 software (StataCorp, Texas, USA). We conducted all the analyses using the weighted samples for national estimates in accordance with HCUP regulations for using the NRD [11]. Age was grouped as 18 - 44 years representing young adults, 45 - 64 years representing middle-aged adults, and 65 years above representing elderly. We calculated comorbidities as proportions of the cohorts and used the Chi-square test to compare characteristics between index hospitalizations and readmissions. We employed a univariable pre-screening model to identify variables associated with readmission to obtain independent predictors of 30 ACR and 90 ACR. We screened age categories, sex, hospital location, hospital teaching status, hospital bed size, mean household income, and the 31 ECI comorbidities (Table 1). The use of Elixhauser comorbidities is similar to the validated model employed by Moore et al for assessing comorbidity burden in administrative databases [18]. We included those variables having a P-value less than 0.1 in the final multivariable regression analysis. Subsequently, we ran a multivariable Cox regression analysis to identify independent predictors of readmissions with P-values < 0.05 set as the threshold for statistical significance. The model included sex, age categories, primary payer, congestive heart failure, cardiac arrhythmias, valvular disease, pulmonary circulation disorders, peripheral vascular disorders, uncomplicated hypertension, uncomplicated, other neurologic disorders, complicated diabetes, renal failure, coagulopathy, weight loss, fluid and electrolyte disorders, drug abuse, psychosis, depression, and complicated hypertension. The NRD lacks patient identifiers. In keeping with other HCUP databases, the NRD does not require Cook County Health Institutional Review Board approval for analysis. The NRD is a large publicly available all-payer inpatient care database in the United States, containing data on more than 18 million hospital stays. Its large sample size provides sufficient data for analysis across hospital types and the study of readmissions for relatively uncommon disorders and procedures. This was a national database study that had no patient identifiers, and we had no direct contact with human/animal subjects.
 Click to view | Table 1. Patient and Hospital Characteristics of PVT Index Hospitalizations and 30-Day Readmissions |
| Results | ▴Top |
We identified 17,971 unique index admissions discharges, of which 2,971 (16.5%) were readmitted within 30 days. Overall, most of the admissions were male and above the age of 45. The mean age was significantly higher in the 30-day readmission cohort compared to the index hospitalization. The demographic and clinical characteristics comparing index hospitalization with 30-day readmission are described in Table 1. We identified 14,696 unique index admissions discharges after applying the inclusion and exclusion criteria for the 90-day readmission cohort. Of these hospitalizations, 3,737 (25.4%) were readmitted within 90 days. The demographic and clinical characteristics comparing index hospitalization and the 90-day readmission cohort are described in Table 2. The most common cause of readmissions in both readmission cohorts was PVT. Sepsis, HCC, and liver failure were the second, third, and fourth most common causes of readmission respectively in both readmission cohorts. Details of the principal causes of readmission, hospitalization costs, and outcomes for PVT hospitalization are described in Table 3. The inpatient mortality rate was 7.7% in the 30-day readmission cohort compared to 7.2% in the 90-day readmission cohort (Table 4). The total LOS and THC were higher in the 30-day readmission cohort compared to the 90-day readmission cohort (Table 4). Results of multivariable Cox regression analysis to identify independent predictors of 30-day ACRs are shown in the Forrest plot (Fig. 1). Discharge against medical advice (AMA) (adjusted hazard ratio (aHR) 1.86, P = 0.002), renal failure (aHR 1.44, P = 0.014), liver failure (aHR 1.34, P = 0.000), metastatic cancer (aHR 1.31, P = 0.016), rheumatoid arthritis and collagen vascular disease (aHR 1.48, P = 0.006), fluid and electrolyte disorders (aHR 1.20, P = 0.004), and alcohol abuse (aHR 1.31, P = 0.000) were associated with increased 30-day readmission risk. The presence of obesity during index admission was associated with a reduced likelihood of readmission within 30 days of index hospitalization (aHR 0.8, P = 0.006). Figures 2 and 3 show the Kaplan-Meier readmission curves for 30- and 90-day readmissions by sex.
 Click to view | Table 2. Patient and Hospital Characteristics of PVT Index Hospitalizations and 90-Day Readmissions |
 Click to view | Table 3. Top 10 Principal Diagnoses of Readmissions for PVT Hospitalizations |
 Click to view | Table 4. Outcomes in PVT 30-Day and 90-Day Readmissions |
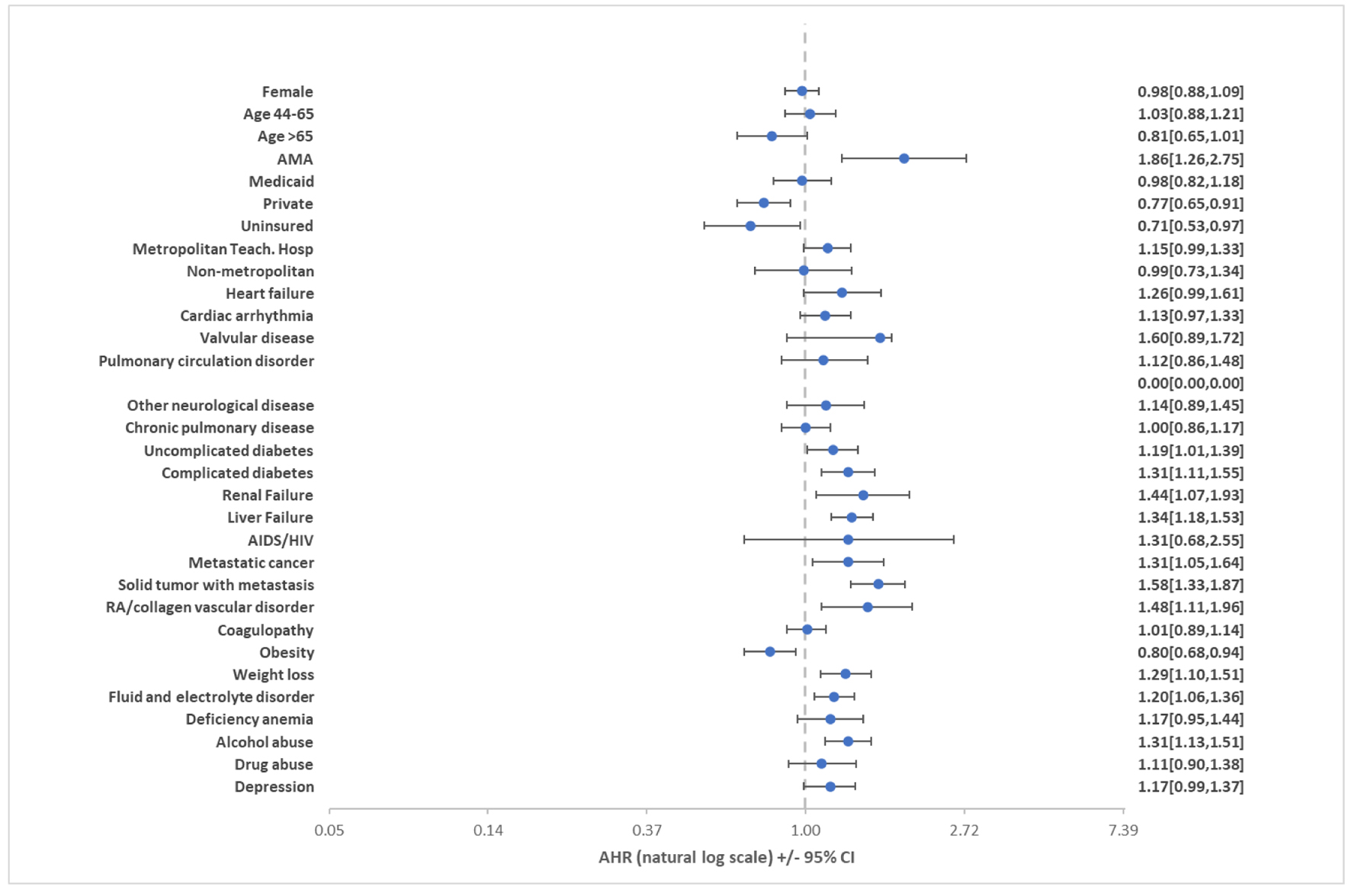 Click for large image | Figure 1. Predictors of 30-day all-cause readmissions of PVT, showing the adjusted hazard ratio with their confidence intervals for the predictors of 30-day all-cause readmissions for PVT hospitalizations. PVT: portal vein thrombosis. |
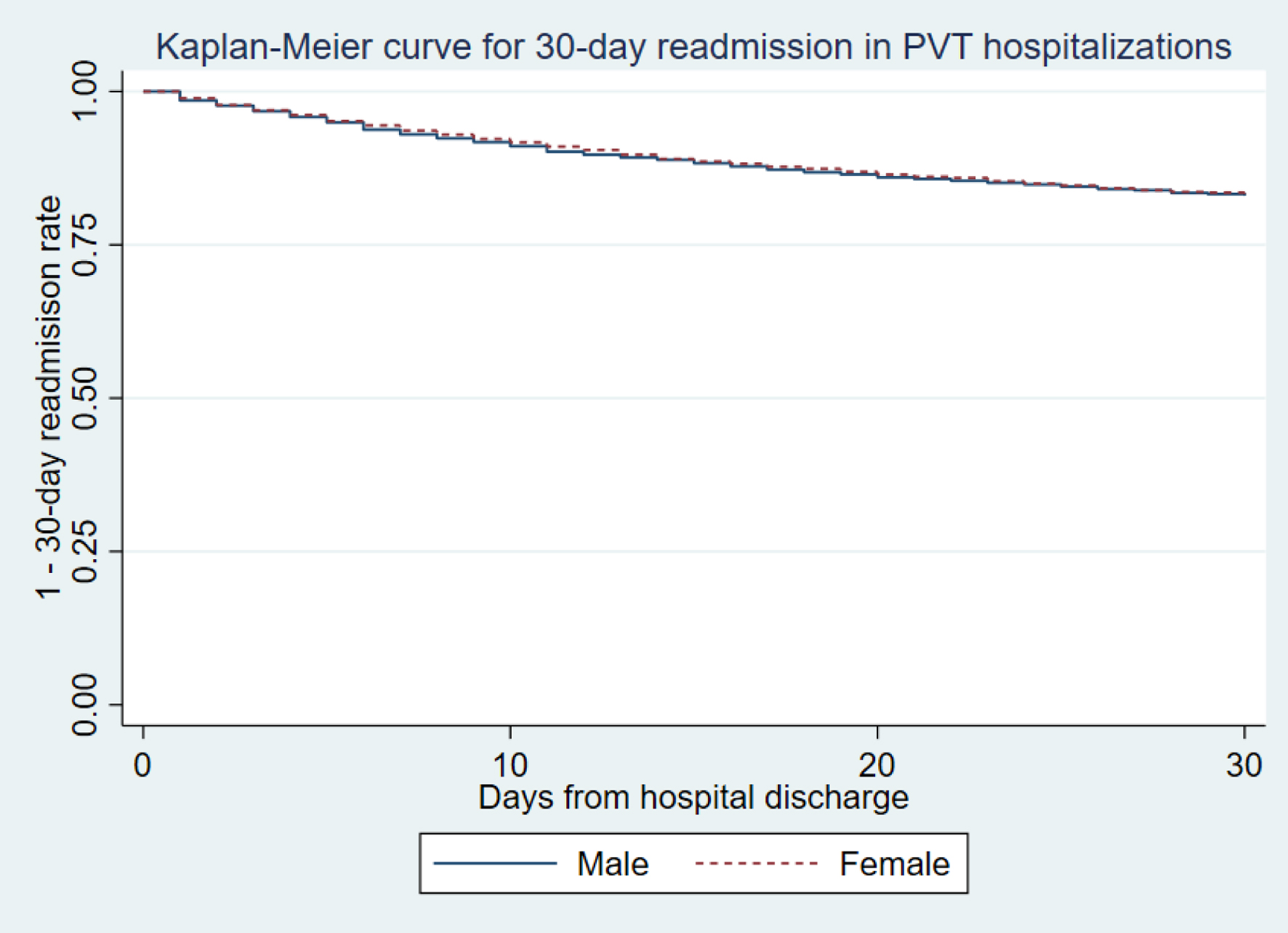 Click for large image | Figure 2. Kaplan-Meier graph for 30-day all-cause readmissions of PVT hospitalizations by sex, showing almost similar distribution by sex in the Kaplan-Meier curve for 30-day readmissions in PVT hospitalizations. PVT: portal vein thrombosis. |
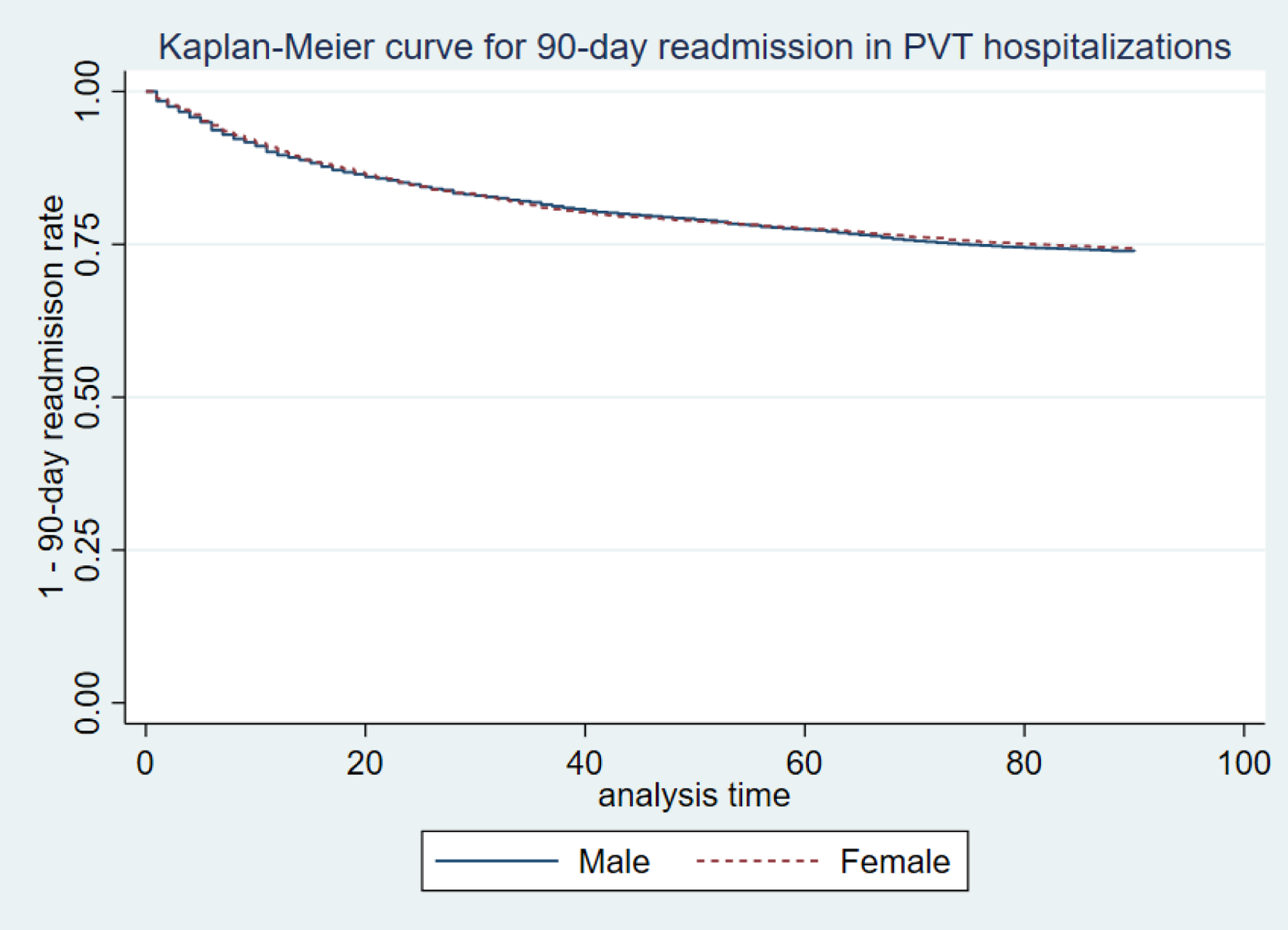 Click for large image | Figure 3. Kaplan-Meier graph for 90-day all-cause readmissions of PVT hospitalizations by sex, showing almost similar distribution by sex in the Kaplan-Meier curve for 90-day readmissions in PVT hospitalizations. PVT: portal vein thrombosis. |
| Discussion | ▴Top |
This study focused on the demographic and clinical characteristics of patients admitted with a primary diagnosis of PVT as well as factors that predict readmission using NRD. We identified a 30-day ACR rate of 16.5% and a 90-day ACR rate of 25.4%. There are no comparison data available on PVT readmissions worldwide; however, this likely represents the actual readmission rates in the United States given the large sample size and representative distribution of hospitals and states included in the NRD. Readmissions have an impact on the overall cost of healthcare and are usually considered an indicator of hospital quality and performance measures which we demonstrated in this study as readmissions significantly cost more than the index hospitalization [8]. The cost of hospitalization was significantly higher in the 30-day readmission group compared to the 90-day group. The reason for this observation is unclear but may be related to the higher mean LOS in the 30-day readmission cohort. Due to the inherent data limitation of the NRD, we were unable to determine the severity of PVT which may have played a role in the cost of hospitalization. We also postulate that the difference in the reasons for readmission may have played a role in the cost burden. The mean age of hospitalizations was similar to a study done in Sweden on patients with PVT where the mean age was shown to be 57 [19]. The number one cause of readmission in both readmission cohorts was PVT. The reason for this observation is unclear but may be due to persistently symptomatic or recurrent PVT. The inpatient mortality rate was significantly higher in the readmission cohorts compared to the index hospitalization. This is likely due to the higher comorbidity burden identified in both readmission cohorts. Higher ECI in readmissions has been shown to be associated with higher mortality [13, 14]. The most significant predictor of 30-day readmission was being discharged AMA. Individuals who leave the hospital AMA form 1-2% of all hospital discharges and are at high risk for readmission [20, 21]. Patients leaving the hospital AMA are more often younger, male, undomiciled, and more likely to have mental illness, alcohol, and drug use [20-22]. Prior studies have shown that patients discharged AMA have higher rates of 30-day ACR rates [20, 22, 23]. In a nationally representative study, individuals discharged AMA had higher 30-day readmission at a tremendous cost to the healthcare system [24]. Patients discharged AMA are also more likely to be readmitted for mental health and substance use disorders and have earlier readmissions as well [24]. Tailored interventions that address the challenges that these patients face, such as communication barriers, mental health/substance use comorbidities, and lack of established primary care, should be considered to improve outcomes after initial hospital discharge [24]. Age, gender, and teaching hospital status had no significant effect on readmission in the multivariable Cox regression analysis. We found solid tumors with metastasis, rheumatoid arthritis, and collagen vascular diseases to be significant independent predictors of 30-day readmission. Chronic inflammatory conditions such as rheumatoid arthritis and malignancies have been shown to increase the risk of venous thromboembolism [25, 26]. The increased risk of 30-day readmission seen in these groups of patients may be related to recurrent PVT or their underlying comorbid conditions. Another significant predictor of 30-day readmission we identified was alcohol abuse. Patients with alcohol abuse have significantly higher rates of readmissions independent of underlying comorbid conditions [27, 28]. The 30-day readmission rates for hospitalized patients with diabetes mellitus are estimated to range from 14.4% to 22.7%, much higher than the rate for all hospitalized patients [29-31]. We found the presence of diabetes to be an independent predictor of readmissions in our 30-day readmission study which is congruent with other studies on diabetes and readmissions [29, 30]. In a cohort of about 10,000 general medicine discharges, weight loss was identified as one of the significant predictors of 30-day readmissions, which was consistent with the finding in our 30-day readmission study [32]. Obesity has been shown to increase the risk of readmissions in some conditions such as heart failure and acute myocardial infarction [33, 34]. In our study, however, we found obesity to be a protective factor for 30-day readmission. The reason for this observation remains unclear and more studies are needed to throw more light on this apparent paradox.
Although this was a comprehensive study using data from the entire country, there were some limitations in our study. Firstly, this was an observational analysis of NRD administrative data and thus our findings cannot establish causation. Secondly, the database reports information on hospitalizations and not on individual patients. Thirdly, data regarding post-discharge clinic follow-up and adherence with anticoagulation were not available, which may have impacted readmission rates. Finally, the NRD uses ICD-10 codes to report hospitalizations and diagnoses; hence we could not ascertain the extent and severity of PVT and its associated complications. Despite the aforementioned limitations, the study has strength in its scientific questions, analysis techniques, and large sample size. The strengths of this study allow it to shed light on a relatively under-studied subject to influence discussions to reduce readmission rates and healthcare costs in patients with PVT.
The readmission rates identified in this study were higher than the national average and targeted interventions addressing these factors may help reduce the overall healthcare costs.
Acknowledgments
The completion of this research work could not have been possible without the help of my mentors, Bashar Attar MD and Hemant Mutneja MD.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
This was a National Readmission Database study hence informed consent does not apply to this study.
Author Contributions
Robert Kwei-Nsoro participated in the study design, writing and review on this manuscript. Pius Ojemolon participated in writing and review of the manuscript. Hisham Laswi participated in writing and review of this manuscript. Ebehiwele Ebhohon participated in writing and review of this manuscript. Abdultawab Shaka participated in writing and review of this manuscript. Wasey Ali Mir participated in the data analysis and review of this manuscript. Abdul Hassan Siddiqui contributed to study design and data analysis. Jobin Philipose contributed to study design and data analysis. Hafeez Shaka contributed to the study design and review of this manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Caiano LM, Riva N, Carrier M, Gatt A, Ageno W. Treatment of portal vein thrombosis: an updated narrative review. Minerva Med. 2021;112(6):713-725.
doi pubmed - Almdal TP, Sorensen TI. Incidence of parenchymal liver diseases in Denmark, 1981 to 1985: analysis of hospitalization registry data. The Danish Association for the Study of the Liver. Hepatology. 1991;13(4):650-655.
doi pubmed - Ogren M, Bergqvist D, Bjorck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12(13):2115-2119.
doi pubmed - Webster GJ, Burroughs AK, Riordan SM. Review article: portal vein thrombosis — new insights into aetiology and management. Aliment Pharmacol Ther. 2005;21(1):1-9.
doi pubmed - Denninger MH, Chait Y, Casadevall N, Hillaire S, Guillin MC, Bezeaud A, Erlinger S, et al. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31(3):587-591.
doi pubmed - Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, development, and treatment of portal vein thrombosis in patients with and without cirrhosis. Gastroenterology. 2019;156(6):1582-1599.e1581.
doi pubmed - Kocher RP, Adashi EY. Hospital readmissions and the affordable care act: paying for coordinated quality care. JAMA. 2011;306(16):1794-1795.
doi pubmed - Chirapongsathorn S, Poovorawan K, Soonthornworasiri N, Pan-Ngum W, Phaosawasdi K, Treeprasertsuk S. Thirty-day readmission and cost analysis in patients with cirrhosis: a nationwide population-based data. Hepatol Commun. 2020;4(3):453-460.
doi pubmed - Fernandez MM, Hogue S, Preblick R, Kwong WJ. Review of the cost of venous thromboembolism. Clinicoecon Outcomes Res. 2015;7:451-462.
doi pubmed - HCUP Nationwide Readmission Database (NRD). 2018. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
- Barrett M, Steiner C, Andrews R, Kassed C, Nagamine M. Methodological Issues when Studying Readmissions and Revisits Using Hospital Administrative Data. 2011. HCUP Methods Series Report # 2011-01. Online March 9, 2011. U.S. Agency for Healthcare Research and Quality. Available: http://www.hcupus.ahrq.gov/reports/methods/methods.jsp.
- Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55(7):698-705.
doi pubmed - Kumar A, Karmarkar A, Downer B, Vashist A, Adhikari D, Al Snih S, Ottenbacher K. Current risk adjustment and comorbidity index underperformance in predicting post-acute utilization and hospital readmissions after joint replacements: implications for comprehensive care for joint replacement model. Arthritis Care Res (Hoboken). 2017;69(11):1668-1675.
doi pubmed - Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472(9):2878-2886.
doi pubmed - Molto A, Dougados M. Comorbidity indices. Clin Exp Rheumatol. 2014;32(5 Suppl 85):S131-S134.
- Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42(4):355-360.
doi pubmed - HCUP Cost-to-Charge Ratio (CCR). 2008 - 2019. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/db/ccr/costtocharge.jsp.
- Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53(1):175-196.
doi pubmed - Rajani R, Bjornsson E, Bergquist A, Danielsson A, Gustavsson A, Grip O, Melin T, et al. The epidemiology and clinical features of portal vein thrombosis: a multicentre study. Aliment Pharmacol Ther. 2010;32(9):1154-1162.
doi pubmed - Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012;125(6):594-602.
doi pubmed - Kraut A, Fransoo R, Olafson K, Ramsey CD, Yogendran M, Garland A. A population-based analysis of leaving the hospital against medical advice: incidence and associated variables. BMC Health Serv Res. 2013;13:415.
doi pubmed - Yong TY, Fok JS, Hakendorf P, Ben-Tovim D, Thompson CH, Li JY. Characteristics and outcomes of discharges against medical advice among hospitalised patients. Intern Med J. 2013;43(7):798-802.
doi pubmed - Garland A, Ramsey CD, Fransoo R, Olafson K, Chateau D, Yogendran M, Kraut A. Rates of readmission and death associated with leaving hospital against medical advice: a population-based study. CMAJ. 2013;185(14):1207-1214.
doi pubmed - Tan SY, Feng JY, Joyce C, Fisher J, Mostaghimi A. Association of hospital discharge against medical advice with readmission and in-hospital mortality. JAMA Netw Open. 2020;3(6):e206009.
doi pubmed - Matta F, Singala R, Yaekoub AY, Najjar R, Stein PD. Risk of venous thromboembolism with rheumatoid arthritis. Thromb Haemost. 2009;101(1):134-138.
doi pubmed - Johannesdottir SA, Schmidt M, Horvath-Puho E, Sorensen HT. Autoimmune skin and connective tissue diseases and risk of venous thromboembolism: a population-based case-control study. J Thromb Haemost. 2012;10(5):815-821.
doi pubmed - Chavez LJ, Liu CF, Tefft N, Hebert PL, Clark BJ, Rubinsky AD, Lapham GT, et al. Unhealthy alcohol use in older adults: Association with readmissions and emergency department use in the 30 days after hospital discharge. Drug Alcohol Depend. 2016;158:94-101.
doi pubmed - Clark BJ, Rubinsky AD, Ho PM, Au DH, Chavez LJ, Moss M, Bradley KA. Alcohol screening scores and the risk of intensive care unit admission and hospital readmission. Subst Abus. 2016;37(3):466-473.
doi pubmed - Kim H, Ross JS, Melkus GD, Zhao Z, Boockvar K. Scheduled and unscheduled hospital readmissions among patients with diabetes. Am J Manag Care. 2010;16(10):760-767.
- Jiang HJ, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421-1426.
doi pubmed - American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033-1046.
doi pubmed - Allaudeen N, Vidyarthi A, Maselli J, Auerbach A. Redefining readmission risk factors for general medicine patients. J Hosp Med. 2011;6(2):54-60.
doi pubmed - Schuller KA. Is obesity a risk factor for readmission after acute myocardial infarction? J Healthc Qual Res. 2020;35(1):4-11.
doi pubmed - Cox ZL, Lai P, Lewis CM, Lindenfeld J. Body mass index and all-cause readmissions following acute heart failure hospitalization. Int J Obes (Lond). 2020;44(6):1227-1235.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


