| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 3, June 2022, pages 127-135
Acute Upper Gastrointestinal Bleeding: Less Severe Bleeding in More Frail and Older Patients, Comparison Between Two Time Periods Fifteen Years Apart
Christos Sotiropoulosa, b , Konstantinos Papantonioua, Efthimios Tsounisa, Georgia Diamantopouloua, Christos Konstantakisa, Georgios Theocharisa, Christos Triantosa, Konstantinos Thomopoulosa
aDepartment of Gastroenterology-Hepatology, University General Hospital of Patras “Holy Mary the Help”, Patra, Greece
bCorresponding Author: Christos Sotiropoulos, Department of Gastroenterology-Hepatology, University General Hospital of Patras “Holy Mary the Help”, Patra, Greece
Manuscript submitted May 4, 2022, accepted June 10, 2022, published online June 22, 2022
Short title: AUGIB in More Frail and Older Patients
doi: https://doi.org/10.14740/gr1534
| Abstract | ▴Top |
Background: Acute upper gastrointestinal bleeding (AUGIB) remains a common medical emergency with considerable morbidity and mortality. The aim of this study was to describe the patient characteristics, diagnoses and clinical outcomes of patients presenting with AUGIB nowadays and compare these with those of patients 15 years ago.
Methods: This was a single-center survey of adults (> 16 years) presenting with AUGIB to a tertiary hospital. Data from 401 patients presenting with AUGIB in a tertiary hospital between January 1, 2019 and December 31, 2020 were analyzed and compared with data from 434 patients presenting with AUGIB at the same hospital between January 1, 2004 and December 31, 2005.
Results: Nowadays, patients were older, mean age was 69.5 (± 15.4) vs. 66.2 (± 16.0) years, they had more frequently coexisting diseases (83.5% vs. 72.8%), especially cardiovascular diseases (62.3% vs. 52.5%), and more individuals were inpatients at onset of bleeding (8.2% vs. 4.1%). In addition, more patients were under anticoagulants (18.5% vs. 6.2%), but less were under acetylsalicylic acid ± clopidogrel (36.9% vs. 33.9%). Carlson Comorbidity Index was higher nowadays (5.6 ± 6.4 vs. 3.4 ± 2.3). Moreover, a peptic ulcer was less frequently found as the cause of bleeding (38.4% vs. 56.9%), while more often nowadays endoscopy was negative (12.7% vs. 3.5%). In patients with peptic ulcer, active bleeding on endoscopy was less frequent (7.1% vs. 14.2%). Also, bleeding spots requiring hemostasis were less common on endoscopy (39.6% vs. 49.4%) and more patients were without spots of recent bleeding (49.4% vs. 38.9%). Finally, the rate of rebleeding statistically decreased (7.8% vs. 4.2%), while overall mortality remained relatively unchanged (5.0% vs. 6.2%).
Conclusions: AUGIB episodes nowadays are less severe with less peptic ulcer bleeding, but the patients are older and with more comorbidities.
Keywords: Upper gastrointestinal bleeding; Gastrointestinal hemorrhage; Peptic ulcers; Helicobacter pylori; Non-steroidal anti-inflammatory drugs; Antithrombotics
| Introduction | ▴Top |
Acute upper gastrointestinal bleeding (AUGIB), originating from a variety of lesions proximal to the ligament of Treitz, remains a relatively common emergency with considerable morbidity and mortality, despite advances in diagnosis and management. Peptic ulcer (gastric and duodenal ulcer) is the most prevalent cause of bleeding, with declining prevalence, but a variety of other lesions may be responsible with variable prognostic importance. Acid peptic disease is followed in prevalence by variceal bleeding, gastric and duodenal erosive disease, esophagitis, Mallory-Weiss tears and malignancies. Approximately, half of AUGIB episodes are caused by peptic ulcers according to previous studies around the world. In most cases, bleeding is self-limited without recurrence and without adverse outcome. In contrast, in less than 20% of patients, bleeding recurs and therapeutic intervention, mostly endoscopic, is needed to stop bleeding and/or prevent rebleeding [1-4].
Over the past decades, diagnosis and treatment of patients with peptic ulcer disease, cirrhosis and portal hypertension has been improved with the introduction of new management algorithms. Better handling of patients with peptic ulcer disease and portal hypertension might have reduced the number of patients suffering from bleeding complications from these causes [5-8]. On the other hand, the population is aging and due to increasing comorbidity, non-steroidal anti-inflammatory drugs (NSAIDs) are widely consumed leading to a parallel increase in bleeding complications. Acetylsalicylic acid and adenosine diphosphate P2Y12 receptor blockers are gradually more prescribed for primary and secondary prophylaxis of adverse cardiovascular events and ischemic attacks. Moreover, in recent years, not only vitamin K antagonists but also newer non-vitamin K oral anticoagulants (NOACs) have been increasingly used for the prevention of venous thromboembolic events [9, 10].
It has been shown that despite medical advances in both diagnostic and therapeutic approach of patients with AUGIB, mortality remained stable over the years around 5-10%. Also, the majority of deaths are not related directly to the bleeding event itself, but rather to coexisting diseases, especially cardiovascular [11].
The aim of this study was to analyze demographic characteristics, laboratory and endoscopic findings and clinical outcome of patients with AUIGB treated in a tertiary hospital over the previous 2 years and to compare these data with those collected 15 years ago in the same hospital over a 2-year period.
| Materials and Methods | ▴Top |
We conducted a prospective wide audit of adults presenting to our hospital with AUGIB for a 2-year period and a retrospective study of patients presenting with AUGIB in the same hospital 15 years ago. The methodology of this study was similar to previously conducted national audits on AUGIB. The study protocol was approved by the ethics committee of University General Hospital of Patras and written informed consent was obtained from all the patients or their next of kin. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Participants
Data from all patients treated in our hospital with AUGIB in 2-year period of time, from January 1, 2019 to December 31, 2020, were prospectively collected. These data were compared with data from a historical control group in the same hospital 15 years ago, from January 1, 2004 to December 31, 2005. We included all patients over 16 years of age with AUGIB treated in our hospital during these two periods. No patients were excluded because of age, comorbidity or presentasion of bleeding during hospitalization for other reason.
Definitions
AUGIB was defined as the presence of melena and/or hematemesis, as well as any other clinical or laboratory evidence of acute bleeding proximal to the ligament of Treitz. The clinical outcomes were analyzed according to the number of blood units transfused per patient, the hospitalization days, the rebleeding and emergency surgery rates and mortality. Mortality was defined as death within the hospitalization period either due to bleeding itself or any other reason.
The management of patients with AUGIB was in general the same during the two periods. Emergency endoscopy during the first 24 h of admission, in the majority of patients, was the standard practice in both periods. In patients with massive bleeding, urgent endoscopy immediately after resuscitation was performed. All patients underwent endoscopy except two (0.5%) in each period. Endoscopy was performed under sedation with midazolam and local pharyngeal anaesthesia with xylocaine spray. Forrest classification was used to classify stigmata of active or recent bleeding: Ia, active spurting bleeding; Ib, active oozing bleeding; IIa, non-bleeding protruding visible vessel; IIb, adherent clot on the bleeding site; IIc, red or black spots. A non-bleeding visible vessel (NBVV) was defined as a resistant to washing protruding red spot. In both periods, endoscopic hemostasis was performed in all patients having active spurting or oozing bleeding, NBVV and adherent clot during emergency endoscopy. Combination of adrenaline injection with a thermal or mechanical method was the standard of care in both periods while argon plasma coagulation (APC) was used in special cases like angiodysplasias.
All patients with non-variceal AUGIB were treated with standard doses of proton pump inhibitors, intravenously on the admission to the hospital. Variceal bleedings were managed with somatostatin intravenously for 5 days and additionally variceal band ligation for esophageal varices and histoacryl injection for gastric varices. Sengstaken-Blakemore tube was rarely used as a bridge to endoscopy.
Data collection
Patients’ data on age, gender, co-existing illnesses, laboratory tests on admission, endoscopic findings and clinical outcome were registered in standardized database categories. Previous or current treatment with aspirin, NSAIDs, adenosine diphosphate P2Y12 receptor blockers, vitamin K antagonists and newer NOACs were registered. Charlson Comorbidity Index was calculated according to patients’ history.
Statistical analysis
Continuous variables were described as mean ± standard deviation and were compared by using Student’s t-test. Categorical variables were expressed as percentages and differences between groups were tested for significance by using the χ2 test. The criterion for statistical significance was P < 0.05. All other analyses were performed with the Statistical Package for the Social Sciences (SPSS) version 20 (SPSS, Chicago, IL).
| Results | ▴Top |
A total of 401 patients hospitalized with AUGIB in the recent period (January 1, 2019 to December 31, 2020) and 434 in the former period (January 2004 through December 2005) were analyzed. Patient characteristics including comorbidity impact, degree of hemodynamic disturbance, laboratory findings and Charlson Comorbity Index are summarised in Table 1.
 Click to view | Table 1. Characteristics of Patients With AUGIB |
Mean age of patients increased from 66 to 70 years (P = 0.003) and most patients were men in both time periods (74.2% vs. 69.6%). Coexisting illnesses were more common in the recent period (335/401, 83.5% vs. 316/434, 72.8%, P = 0.03) and cardiovascular disease was the most common comorbitity in both periods with increased frequency in the recent (62.3% vs. 52.5%, P = 0.004). Charlson Comorbidity Index was higher nowadays (6 points vs. 3 points, P = 0.01). Also, more bleeding events occurred in the recent period in already hospitalized patients for other causes (33/401, 8.2% vs. 18/434, 4.1%, P = 0.0001).
One-third of the patients were under acetylsalicylic acid ± adenosine diphosphate (P2Y12) receptor inhibitors treatment and almost one-fifth under warfarin or NOACs. The percentage of patients under anticoagulation treatment, either with warfarin or NOACs on admission, was higher in the recent period (74/401, 18.5% vs. 27/434, 6.2%, P = 0.0001), while treatment with acetylsalicylic acid ± clopidogrel was common and not different between the two periods (160/434, 36.9% vs. 136/401, 33.9%). Peptic ulcer remains (in period 2019 - 2020) the most common cause of bleeding (38.4%) followed by varices (13.2%), vascular malformations (8.5%), tumors/polyps (7.3%) and gastroduodenal erosions (6%) (Fig. 1).
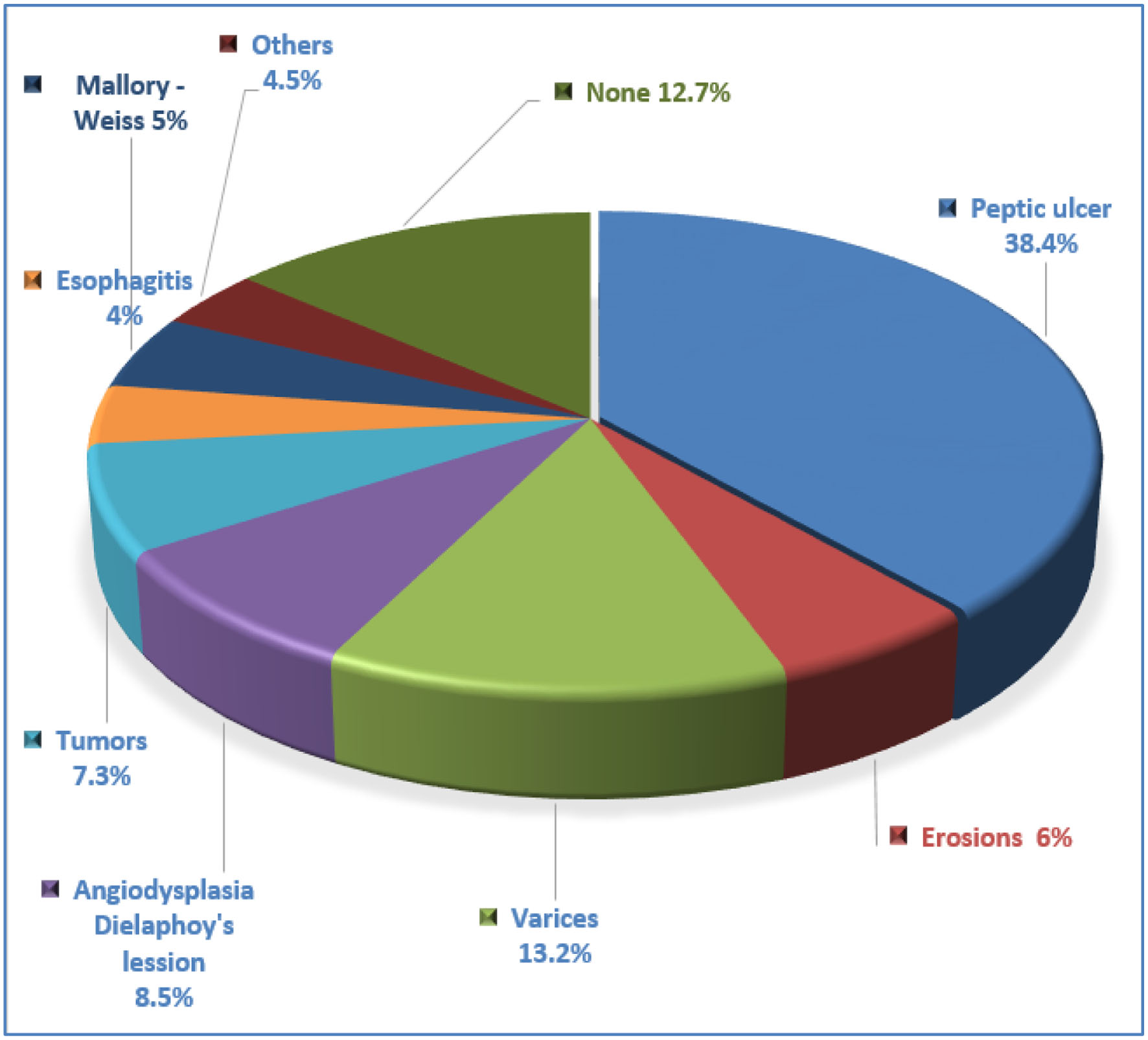 Click for large image | Figure 1. Causes of bleeding (%) during period 2019 - 2020. |
A peptic ulcer was less frequently the cause of bleeding (154/401, 38.4% vs. 247/434, 56.9%, P = 0.0001), as well as gastroduodenal erosions (24/401, 6.0% vs. 43/434, 9.9%, P = 0.0001) in comparison between the two time periods (Table 2).
 Click to view | Table 2. Causes of AUGIB |
In contrast, more frequent causes of bleeding were varices (53/401, 13.2% vs. 32/434, 7.4%, P = 0.043) and vascular malformations (34/401, 8.5% vs. 13/434, 3%, P = 0.0004). Also, more often nowadays upper gastrointestinal endoscopy was negative, without any identifiable source of bleeding (51/401, 12.7% vs. 15/434, 3.5%, P = 0.011) (Fig. 2).
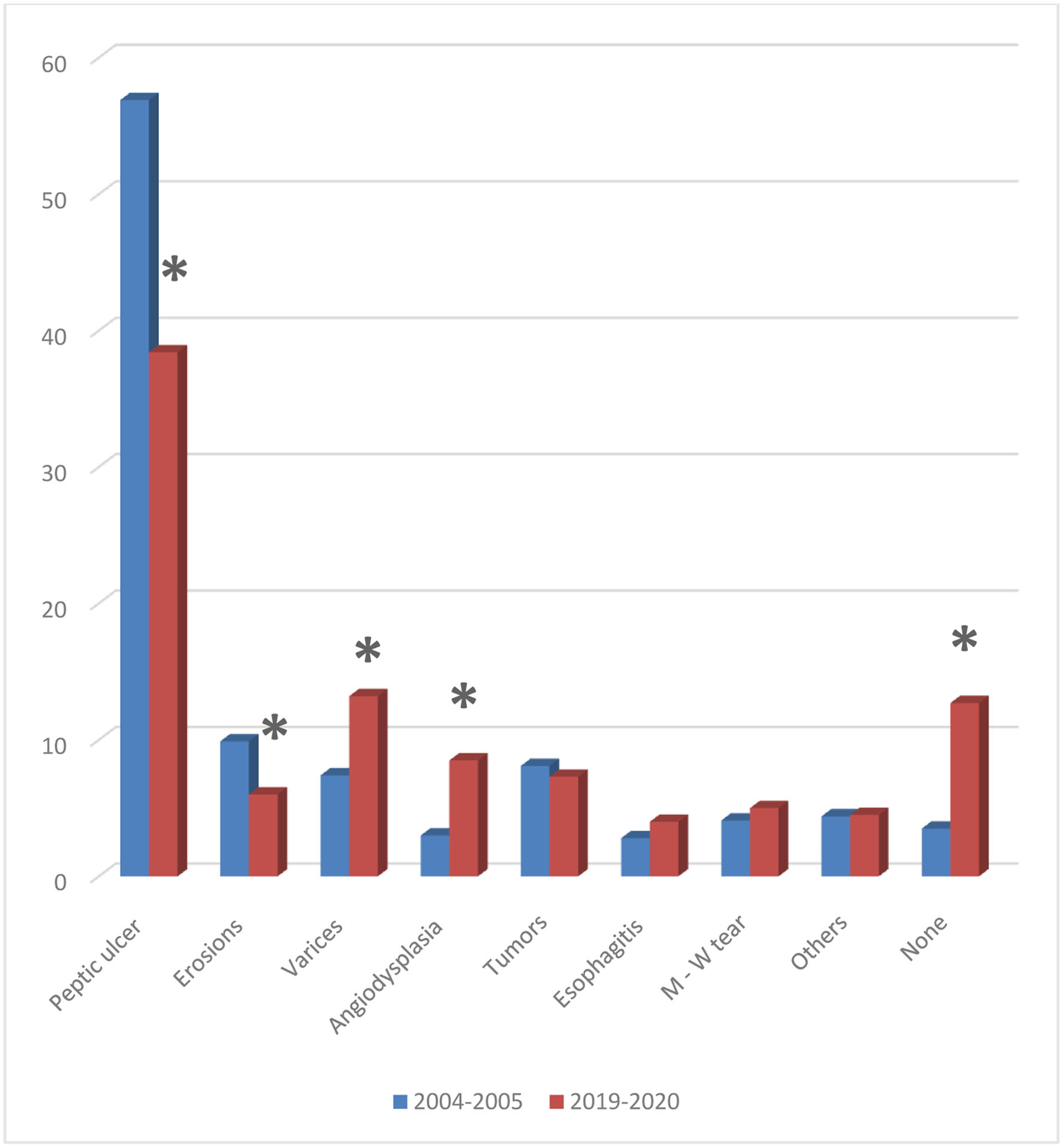 Click for large image | Figure 2. Causes of bleeding (%) in comparison between the two time periods (*P < 0.05). |
Recently, in peptic ulcer bleeding patients, active bleeding on endoscopy was less frequent (11/154, 7.1% vs. 35/247, 14.2%, P = 0.03), as well as stigmata of recent bleeding requiring hemostasis (61/54 vs. 122/247, P = 0.055). Conversely, more patients were without spots of recent bleeding (76/154, 49.4% vs. 96/247, 38.9%, P = 0.04) (Table 3, Fig. 3).
 Click to view | Table 3. Stigmata of Recent Bleeding in Peptic Ulcer Bleeding Patients |
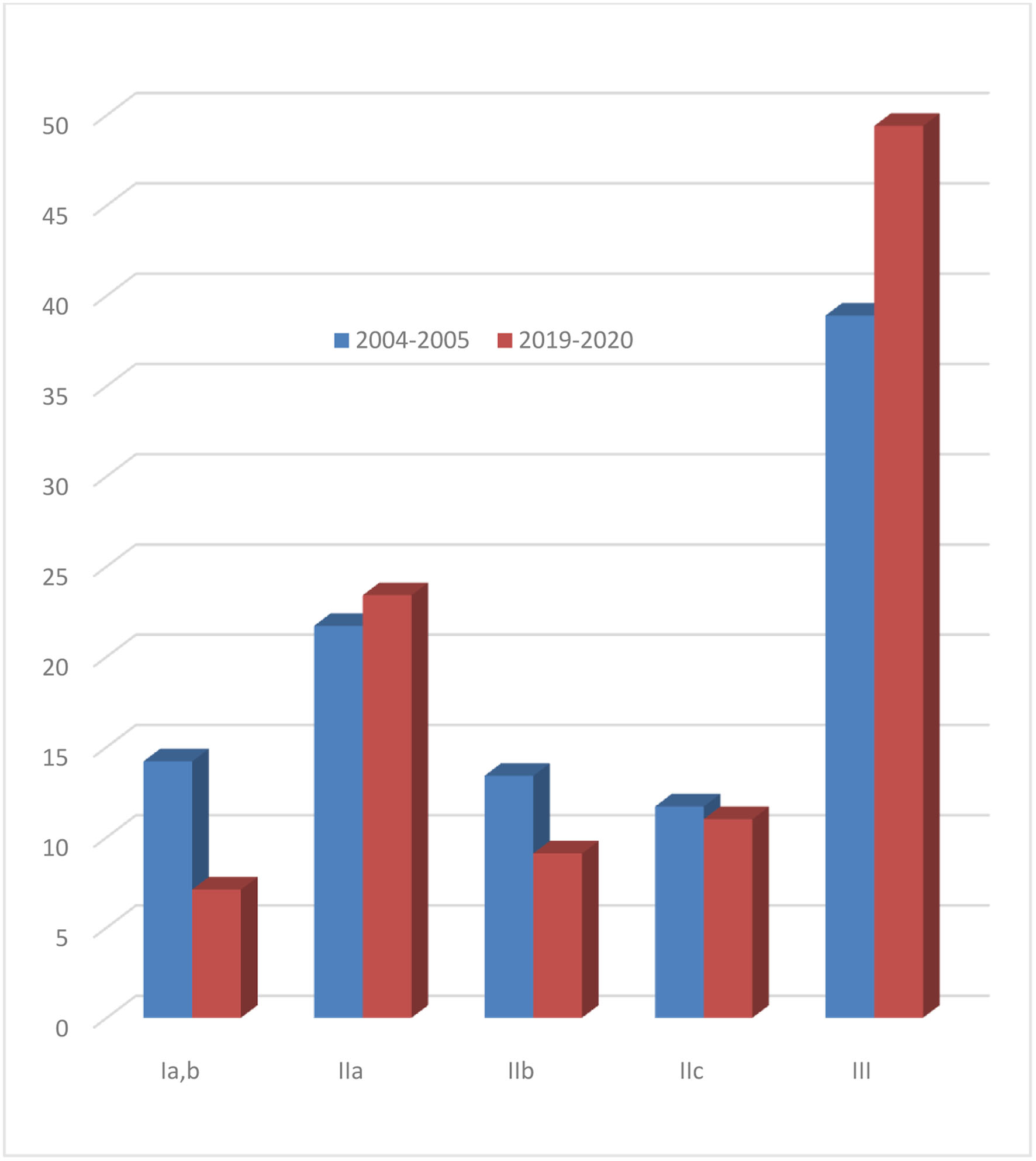 Click for large image | Figure 3. Active bleeding or stigmata of recent bleeding in patients with peptic ulcer bleeding (%) in comparison with the two time periods. |
Seventeen out of 401 patients rebled (4.2%) and 11/401 (3%) underwent emergency surgery. The rate of rebleeding statistically decreased (from 34/434, 7.8% to 17/401, 4.2%, P = 0.03), while rates of emergency surgical hemostasis were low and not different between the two periods (2.7% vs. 3.0%). Also, hospitalization days and transfused blood units were not different between the two periods. A total of 20 patients died during the period of hospitalization giving an overall mortality of 5% and remained unchanged between the two periods (20/401, 5.0% vs. 27/434, 6.2%) (Table 4).
 Click to view | Table 4. Clinical Outcome of Patients With AUGIB |
| Discussion | ▴Top |
In this study, we analyzed clinico-epidemiological characteristics and clinical outcomes of patients with AUGIB treated in our hospital over the previous 2 years. We also compared these data with those collected 15 years ago in the same hospital over a 2-year period. We found that nowadays, patients are older with more comorbidities, especially cardiovascular and more often under antithrombotic treatment. Peptic ulcer remains the most frequent cause of bleeding, but with less frequency, while varices and vascular malformations presented with increased frequency. Moreover, increased percentage of patients was without an identifiable source of bleeding. Active bleeding peptic ulcers are less common and rebleeding is less frequent. However, overall mortality remained unchanged.
The reduction in the prevalence of peptic ulcer as cause of bleeding is due to the declining incidence of peptic ulcer disease in developed countries, the cure of patients with chronic duodenal ulcers with the eradication of Helicobacter pylori (H. pylori) and the prevention of aspirin and NSAIDs-related ulcer bleeding.
Several studies have shown that the incidence and complication rates of peptic ulcers around the world have been decreased during the last three decades [12-15]. The reduction in the incidence of H. pylori infection worldwide is the main reason for these changes as it is the main causative agent for peptic ulcer disease [13, 16]. Improvement in the socio-sanitary conditions in developed countries explains the low acquisition rate of the organism. Also in peptic ulcer patients, ulcer recurrences as well as ulcer bleeding and rebleeding rates are rare following successful eradication of H. pylori, which can be achieved in over 90% of patients with peptic ulcer [17, 18].
However, despite a decreasing incidence of H. pylori infection and the widespread use of successful H. pylori eradication regimens, peptic ulcer disease remains the most common cause of AUGIB [19]. Guo et al in a previously published study on the reduction in peptic ulcer disease-related hospitalizations from 2005 to 2014 in USA found that the rate of decline decreased from -7.2% per year before 2008 to -2.1% per year after 2008 [20]. This may be explained by the increasing use of aspirin and/or NSAIDs especially in older patients. Prescriptions for NSAIDs in the UK had been increased by about 13% and aspirin 75 mg by 460% in the general population in a previous study [21]. In our study, one-third of patients were under treatment with aspirin and this percentage was similar to that observed 15 years ago. Gastric ulcers in contrast to duodenal ulcers are more likely due to aspirin and/or NSAIDs use than to H. pylori infection. Although gastroprophylaxis with proton pump inhibitors in patients receiving NSAIDs especially in the elderly is the current practice, expanding indications for aspirin and/or NSAIDs use may counteract the beneficial effect of prophylactic treatment on the prevention of peptic ulcer formation and bleeding in patients taking NSAIDs [22, 23]. In this study, patients are older nowadays and about two-thirds suffered of some type of cardiovascular disease. Moreover, over-the-counter use of these medications even for not appropriate indications and inadequate access to medical services may contribute. Cyclooxygenase-2 (COX-2) selective inhibitors are associated with significantly fewer gastroduodenal errosions and complications but are contrainticated in patients with cardiovascular diseases and cannot substitute NSAIDs in general.
On the other hand, we observed a higher use of oral anticoagulants, either warfarin or NOACs, in our patients with AUGIB recently and probably use of these medications will expand in the future due to the increasing indications of oral anticoagulantion in a variety of diseases, especially in the elderly population. Orlowski and colleagues compared the time periods of 2011 - 2014 versus 2014 - 2017 in the UK, using National Health Service data, and demonstrated a dramatic increase (over 85%) in oral anticoagulation prescribing, mostly due to the increased use of NOACs [24]. NOACs, which are increasingly prescribed, are associated with the same risk of major gastrointestinal bleeding compared with conventional vitamin K antagonists [25]. Especially, dabigatran due to tartaric acid coating has been proposed to directly affect the intestinal lumen, therefore enhancing the bleeding risk [26, 27]. Increased use of anticoagulation may explain the increased frequency of angiodysplasias as cause of bleeding as well as the substantial number of patients with no obvious cause of bleeding [28, 29]. Usually, these agents are not ulcerogenic and produce AUGIB from minor pre-existing lesions like angiodysplasias. Also patients with undiagnosed cancers and/or polyps are at increased risks of acute bleeding [30]. Augustson et al in a recent study found that oral anticoagulant users were more likely to bleed from polyps, mucosal erosions and angiodysplasias compared to those not on oral anticoagulants [31].
Rebleeding rates were lower recently in comparison with the previous period. Most rebleedings in AUGIB patients occur in patients with peptic ulcer and varices. Endoscopic hemostasis today may be more efficient either due to better experience of the endoscopists or to the availability of more sophisticated methods like clips and bands. Also, peptic ulcers in the second period might be more suitable for endoscopic hemostasis compared with the previous period. Actively bleeding peptic ulcers which are more difficult for successful endoscopic hemostasis were less frequent recently. This may be due to reduced prevalence of chronic ulcers which in contrast to acute ulcers produce deformation of the duodenal and gastric wall and erode deeper and larger vessels which give rise to more severe bleeding and make endoscopic hemostasis difficult or even impossible [32-34].
Overall mortality rates in our patients were similar in both periods in our area. It is known that the majority of deaths in patients with AUGIB are not related to exsanguination but rather to coexisting diseases, especially cardiovascular due to inability of these patients to recover from rebleeding or surgery [11]. A recent meta-analysis reported UGIB secondary to peptic ulcer bleeding patients with comorbidities were at several-fold higher risk of overall mortality when compared to patients without comorbidities [34]. Although patients are older and have more comorbidities, rebleeding rate which is associated with mortality was lower in the second period. Lower rebleeding rates may counteract the increased deaths due to comorbidities because less frequently the patients are exposed to blood loss which is poorly tolerated by these patients and so they are less vulnerable to destabilization and death. Also, AUGIB under anticoagulation had similar clinical outcome or even better in previous studies [28, 29]. Pannach et al in a previous study found that patients under NOACs had shorter hospitalization and in-hospital mortality (1.6%) compared with those under warfarin (5.6%) and those under antiplatelet agents (11.9%).
In conclusion, patients with AUGIB nowadays, despite being older, more often with comorbidities and under anticoagulation therapy, suffer from less severe bleeding with less rebleedings and without increased in-hospital mortality.
Acknowledgments
Throughout the conduction of this study, I have received a great deal of support and assistance. I would first like to thank the co-authors of this study for valuable assistance in designing, data collection and analysis of this clinical survey. I would also like to acknowledge my colleagues from the Department of Gastroenterology-Hepatology in University General Hospital of Patras, for their wonderful collaboration.
Financial Disclosure
No funding was received for this work.
Conflict of Interest
The authors declare that there is no conflict of interest.
Informed Consent
Data collection from patients’ records was held by obtaining a written informed consent from all participants or their next of kin.
Author Contributions
Christos Sotiropoulos, Konstantinos Papantoniou, Efthimios Tsounis, Georgia Diamantopoulou, Christos Konstantakis, George Theocharis, Christos Triantos and Konstantinos Thomopoulos confirmed sole responsibility for the following: study conception and design, data collection, analysis and manuscript preparation. All authors of this manuscript have directly participated in the planning, execution, or analysis of this study and are the only ones responsible for the originality of the scientific content of the manuscript. Finally, all authors have read and approved the manuscript.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to restrictions (they are containing information that could compromise the privacy of research participants).
Abbreviations
AUGIB: acute upper gastrointestinal bleeding; UGIB: upper gastrointestinal bleeding; NSAIDs: non-steroidal anti-inflammatory drugs; NOACs: newer non-vitamin K oral anticoagulants; NBVV: non-bleeding visible vessel; APC: argon plasma coagulation; SPSS: Statistical Package for the Social Sciences; COX-2: cyclooxygenase-2
| References | ▴Top |
- Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995;90(2):206-210.
- Rockall TA, Logan RF, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ. 1995;311(6999):222-226.
doi pubmed - van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22(2):209-224.
doi pubmed - Falcao D, Alves da Silva J, Pereira Guedes T, Garrido M, Novo I, Pedroto I. The current portrayal of non-variceal upper gastrointestinal bleeding in a portuguese tertiary center. GE Port J Gastroenterol. 2021;28(6):392-397.
doi pubmed - Oakland K. Changing epidemiology and etiology of upper and lower gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2019;42-43:101610.
doi pubmed - Mullady DK, Wang AY, Waschke KA. AGA Clinical practice update on endoscopic therapies for non-variceal upper gastrointestinal bleeding: expert review. Gastroenterology. 2020;159(3):1120-1128.
doi pubmed - Lau LHS, Sung JJY. Treatment of upper gastrointestinal bleeding in 2020: New techniques and outcomes. Dig Endosc. 2021;33(1):83-94.
doi pubmed - Pfisterer N, Unger LW, Reiberger T. Clinical algorithms for the prevention of variceal bleeding and rebleeding in patients with liver cirrhosis. World J Hepatol. 2021;13(7):731-746.
doi pubmed - Paternoster M, Steichen O, Lapeyre-Mestre M, Blanchon T, Rossignol L, Vilcu AM, Launay T, et al. Risk of bleeding associated with nonsteroidal anti-inflammatory drug use in patients exposed to antithrombotic therapy: a case-crossover study. J Clin Pharmacol. 2022;62(5):636-645.
doi pubmed - Verso M, Giustozzi M, Vinci A, Franco L, Vedovati MC, Marchesini E, Becattini C, et al. Risk factors and one-year mortality in patients with direct oral anticoagulant-associated gastrointestinal bleeding. Thromb Res. 2021;208:138-144.
doi pubmed - Sung JJ, Tsoi KK, Ma TK, Yung MY, Lau JY, Chiu PW. Causes of mortality in patients with peptic ulcer bleeding: a prospective cohort study of 10,428 cases. Am J Gastroenterol. 2010;105(1):84-89.
doi pubmed - Lassen A, Hallas J, Schaffalitzky de Muckadell OB. Complicated and uncomplicated peptic ulcers in a Danish county 1993-2002: a population-based cohort study. Am J Gastroenterol. 2006;101(5):945-953.
doi pubmed - Perez-Aisa MA, Del Pino D, Siles M, Lanas A. Clinical trends in ulcer diagnosis in a population with high prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther. 2005;21(1):65-72.
doi pubmed - Feinstein LB, Holman RC, Yorita Christensen KL, Steiner CA, Swerdlow DL. Trends in hospitalizations for peptic ulcer disease, United States, 1998-2005. Emerg Infect Dis. 2010;16(9):1410-1418.
doi pubmed - Malmi H, Kautiainen H, Virta LJ, Farkkila N, Koskenpato J, Farkkila MA. Incidence and complications of peptic ulcer disease requiring hospitalisation have markedly decreased in Finland. Aliment Pharmacol Ther. 2014;39(5):496-506.
doi pubmed - Xia HH, Phung N, Altiparmak E, Berry A, Matheson M, Talley NJ. Reduction of peptic ulcer disease and Helicobacter pylori infection but increase of reflux esophagitis in Western Sydney between 1990 and 1998. Dig Dis Sci. 2001;46(12):2716-2723.
doi pubmed - Rokkas T, Karameris A, Mavrogeorgis A, Rallis E, Giannikos N. Eradication of Helicobacter pylori reduces the possibility of rebleeding in peptic ulcer disease. Gastrointest Endosc. 1995;41(1):1-4.
doi - Labenz J, Borsch G. Role of Helicobacter pylori eradication in the prevention of peptic ulcer bleeding relapse. Digestion. 1994;55(1):19-23.
doi pubmed - Manuel D, Cutler A, Goldstein J, Fennerty MB, Brown K. Decreasing prevalence combined with increasing eradication of Helicobacter pylori infection in the United States has not resulted in fewer hospital admissions for peptic ulcer disease-related complications. Aliment Pharmacol Ther. 2007;25(12):1423-1427.
doi pubmed - Guo H, Lam AY, Shaheen AA, Forbes N, Kaplan GG, Andrews CN, Laffin M, et al. Urban-rural disparities and temporal trends in peptic ulcer disease epidemiology, treatment, and outcomes in the United States. Am J Gastroenterol. 2021;116(2):296-305.
doi pubmed - Higham J, Kang JY, Majeed A. Recent trends in admissions and mortality due to peptic ulcer in England: increasing frequency of haemorrhage among older subjects. Gut. 2002;50(4):460-464.
doi pubmed - Hawkey CJ. Non-steroidal anti-inflammatory drugs: who should receive prophylaxis? Aliment Pharmacol Ther. 2004;20(Suppl 2):59-64.
doi pubmed - Scally B, Emberson JR, Spata E, Reith C, Davies K, Halls H, Holland L, et al. Effects of gastroprotectant drugs for the prevention and treatment of peptic ulcer disease and its complications: a meta-analysis of randomised trials. Lancet Gastroenterol Hepatol. 2018;3(4):231-241.
doi - Orlowski A, Gale CP, Ashton R, Petrungaro B, Slater R, Nadarajah R, Cowan JC, et al. Clinical and budget impacts of changes in oral anticoagulation prescribing for atrial fibrillation. Heart. 2021;107(1):47-53.
doi pubmed - Burr N, Lummis K, Sood R, Kane JS, Corp A, Subramanian V. Risk of gastrointestinal bleeding with direct oral anticoagulants: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2017;2(2):85-93.
doi - Miller CS, Dorreen A, Martel M, Huynh T, Barkun AN. Risk of gastrointestinal bleeding in patients taking non-vitamin k antagonist oral anticoagulants: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2017;15(11):1674-1683.e1673.
doi pubmed - Sharma M, Cornelius VR, Patel JP, Davies JG, Molokhia M. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: systematic review and meta-analysis. Circulation. 2015;132(3):194-204.
doi pubmed - Bozic D, Vukovic J, Mustapic I, Vrebalov Cindro P, Bozic J, Kardum G, Puljiz Z, et al. Characteristics and clinical outcomes of patients with acute gastrointestinal bleeding related to anticoagulant or antiplatelet therapy: a retrospective study. Croat Med J. 2021;62(5):488-494.
doi pubmed - Pannach S, Goetze J, Marten S, Schreier T, Tittl L, Beyer-Westendorf J. Management and outcome of gastrointestinal bleeding in patients taking oral anticoagulants or antiplatelet drugs. J Gastroenterol. 2017;52(12):1211-1220.
doi pubmed - Chen Y, Mao M, Chang J, Yan J, Yang T, Liu Y, Luo M, et al. Safety and efficacy of new oral anticoagulants compared to those of warfarin in AF patients with cancer: a meta-analysis of randomized clinical trials and observational studies. Eur J Clin Pharmacol. 2021;77(6):849-857.
doi pubmed - Agustsson AS, Ingason AB, Rumba E, Palsson D, Reynisson IE, Hreinsson JP, Bjornsson ES. Causes of gastrointestinal bleeding in oral anticoagulant users compared to non-users in a population-based study. Scand J Gastroenterol. 2022;57(2):239-245.
doi pubmed - Thomopoulos KC, Mitropoulos JA, Katsakoulis EC, Vagianos CE, Mimidis KP, Hatziargiriou MN, Nikolopoulou VN. Factors associated with failure of endoscopic injection haemostasis in bleeding peptic ulcers. Scand J Gastroenterol. 2001;36(6):664-668.
doi pubmed - Brullet E, Calvet X, Campo R, Rue M, Catot L, Donoso L. Factors predicting failure of endoscopic injection therapy in bleeding duodenal ulcer. Gastrointest Endosc. 1996;43(2 Pt 1):111-116.
doi - Leontiadis GI, Molloy-Bland M, Moayyedi P, Howden CW. Effect of comorbidity on mortality in patients with peptic ulcer bleeding: systematic review and meta-analysis. Am J Gastroenterol. 2013;108(3):331-345; quiz 346.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


