| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 17, Number 2, April 2024, pages 82-89
A Comprehensive Study on the Diagnostic Value of Multi-Slice Computed Tomography for Peripancreatic Infection in Elderly With Severe Acute Pancreatitis
Rui Haoa, c, Yu Sunb, Yang Hub
aDepartment of Emergency, Affiliated People’s Hospital of Ningbo University, Ningbo, China
bDepartment of Critical Care Medicine, The 964th Hospital of the Chinese People’s Liberation Army, Changchun, China
cCorresponding Author: Rui Hao, Department of Emergency, Affiliated People’s Hospital of Ningbo University, Ningbo 315040, Zhejiang Province, China
Manuscript submitted October 7, 2023, accepted January 5, 2024, published online April 30, 2024
Short title: Diagnostic MSCT in SAP
doi: https://doi.org/10.14740/gr1679
| Abstract | ▴Top |
Background: This study investigated the diagnostic efficacy of multi-slice spiral computed tomography (MSCT) perfusion imaging in evaluating peripancreatic infection in elderly patients with severe acute pancreatitis (SAP).
Methods: A retrospective analysis was conducted on the clinical data of 110 elderly SAP patients treated at our hospital from March 2018 to August 2019. The study correlated MSCT perfusion imaging characteristics with peripancreatic infection in elderly SAP patients. Additionally, receiver operating characteristic (ROC) curves were constructed to assess the diagnostic performance of MSCT perfusion imaging parameters in evaluating peripancreatic infection in elderly SAP patients.
Results: The results indicated that among all 110 elderly SAP patients, the incidence rate of peripancreatic infection was 20.91%, with a mortality rate of 0.91%. MSCT perfusion imaging revealed that after peripancreatic infection in elderly SAP patients, there was a decrease in pancreatic density, local enlargement of the pancreas, blurring of the pancreatic margins, and associated ascites. Compression/narrowing/occlusion of the splenic vein was observed in 22 patients, compression/narrowing/occlusion of the superior mesenteric vein in 17 patients, thickening/thrombosis of the portal vein in 19 patients, and collateral circulation in 21 patients. Compared to elderly SAP patients without peripancreatic infection, those with the infection showed prolonged peak times, reduced peak heights, and decreased blood flow. ROC analysis indicated that the combination of the three parameters (peak time, peak height, and blood flow) had higher specificity and area under the curve (AUC) than single parameters, with no significant difference in sensitivity between the combination and single parameters.
Conclusions: In conclusion, combining the three key MSCT perfusion imaging parameters (peak time, peak height, and blood flow) can significantly enhance the predictive efficacy for the risk of peripancreatic infection in elderly SAP patients.
Keywords: Elderly SAP patients; Peripancreatic infection; Multi-slice computed tomography; Diagnostic efficacy; Perfusion imaging; Predictive accuracy
| Introduction | ▴Top |
Severe acute pancreatitis (SAP) is a prevalent and serious medical condition, especially among the elderly, and represents a significant public health concern [1]. SAP is often complicated by the relatively high incidence of peripancreatic infections, which pose a substantial threat to patients’ quality of life and their chances of survival [2]. Consequently, early detection and assessment of infections around the pancreas play a pivotal role. Timely interventions based on accurate diagnoses can significantly improve the disease’s prognosis and reduce the risk of patient mortality [3].
Despite these critical clinical needs, traditional imaging diagnostic methods such as ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT) scans have been found to have limitations in the early detection of peripancreatic infections during actual clinical practice [4]. These modalities often fall short in both sensitivity and specificity, mainly when dealing with pancreatic lesions, especially those in their early stages. Additionally, they frequently struggle to determine the location and extent of such lesions precisely [5]. Consequently, there is a pressing need for an imaging diagnostic method to provide accurate, noninvasive, real-time, and reliable results to meet the clinical demand for early pancreatic infection diagnosis.
In recent years, the development and application of multi-slice spiral computed tomography (MSCT) perfusion imaging technology have offered new prospects [6]. MSCT perfusion imaging not only reveals the morphological characteristics of the pancreas but also provides vital hemodynamic information about pancreatic tissue. This comprehensive approach forms a robust foundation for diagnosing pancreatic lesions [7, 8]. Despite its significant potential for assessing pancreatic diseases [9, 10], a notable research gap exists regarding the systematic and comprehensive evaluation of peripancreatic infections in elderly SAP patients.
To address this knowledge gap, we undertook this study to assess and explore the effectiveness of MSCT perfusion imaging in diagnosing peripancreatic infections in elderly SAP patients. This study involved a retrospective analysis of clinical and radiographic data from 110 elderly SAP patients to scrutinize the relationship between radiographic features observed through MSCT perfusion imaging and peripancreatic infections. Additionally, we employed receiver operating characteristic (ROC) curves to comprehensively evaluate the sensitivity and specificity of MSCT perfusion imaging parameters for diagnosing peripancreatic infections in elderly SAP patients.
Our study focuses on three key parameters: pancreatic peak time, height, and blood flow volume. These parameters serve as critical indicators for assessing pancreatic blood perfusion, and changes in pancreatic blood perfusion are often closely associated with peripancreatic infections. Through our in-depth analysis of the relationship between these parameters and peripancreatic infections, we aimed to identify specific MSCT perfusion imaging parameters or parameter combinations that can enhance predicting and diagnosing peripancreatic infections in elderly SAP patients.
This study aimed to enrich and advance the application of MSCT perfusion imaging in diagnosing pancreatic diseases, particularly in improving its efficacy in diagnosing peripancreatic infections in elderly SAP patients. By measuring the peak time, peak height, and blood flow rate of the pancreas using MSCT perfusion imaging, we ultimately hope to achieve early and accurate diagnosis and prediction of the risk of peripancreatic infections in elderly SAP patients. This will provide valuable references and evidence for clinical practice, enabling timely and effective treatment to improve patient's quality of life and prognosis.
| Materials and Methods | ▴Top |
Subjects
This study was approved by the Clinical Ethics Committee of Ningbo University Affiliated People’s Hospital (approval number: 201802). A retrospective analysis was conducted on the clinical data of 110 elderly SAP patients admitted to the hospital from March 2018 to August 2019. All patients were admitted within 24 h after the onset of SAP. The inclusion criteria for eligible patients were as follows: 1) Elderly patients aged 60 years and above; 2) Diagnosed with acute pancreatitis according to the “Guidelines for the Diagnosis and Treatment of Acute Pancreatitis”, confirmed by imaging examinations such as abdominal ultrasound and abdominal CT scans, as well as laboratory tests including blood amylase and serum lipase, and accompanied by persistent (> 48 h) organ dysfunction [11]; 3) Patients who underwent MSCT perfusion imaging examination; 4) Patients with necessary data available. Exclusion criteria included: 1) Patients with trauma; 2) Patients who had undergone pancreatic surgery; 3) Patients who voluntarily gave up diagnosis and treatment; 4) Transferred patients; 5) Patients with other acute or chronic diseases such as malignant tumors, cardiovascular diseases.
The study was conducted in full compliance with the ethical standards of the responsible institution regarding human subjects and in accordance with the principles of the Declaration of Helsinki. We obtained the necessary approvals from the Institutional Review Board (IRB) of the institution prior to the commencement of the study.
SAP management program
According to the “2014 Chinese Guidelines for the Diagnosis and Treatment of Pancreatitis” and the “Consensus on Multidisciplinary Diagnosis and Treatment (MDT) of Acute Pancreatitis in China”, treatment is conducted based on the recommended foundational treatment plan. This plan includes intensive care, critical care, fasting, bowel examination, fluid resuscitation, sedation, pancreatic secretion inhibition, acid suppression, and antimicrobial therapy. Organ support is also provided to maintain organ function [12, 13].
MSCT perfusion imaging
A total of 110 patients included in this study underwent immediate MSCT examination upon admission, with no patients excluded due to refusal of MSCT scanning. The GE LightSpeed 128-slice MSCT scanner was utilized for perfusion scanning. Each patient wore an abdominal strap and received training for steady breathing. Initially, a routine CT scan was performed to establish the perfusion layer, followed by a 5-mm-thick perfusion scan in the lesion area. A nonionic contrast agent of 50 mL was administered at a rate of 4.0 mL/s through the median cubital vein, with a scan delay of 6.0 s and a scan duration of 60 s, using a matrix of 512 × 512. The imaging speed of the axial scan was one frame per second, with a tube voltage of 120 kV, a tube current of 60 mA, and a field of view of 26 cm. Perfusion analysis was conducted using pancreatic perfusion software on a workstation, with efforts made to avoid selecting vascular regions of interest. The abdominal aorta was chosen as the arterial site for perfusion, and a deconvolution model was used to calculate perfusion parameters such as time to peak, peak height, and blood flow. Each patient underwent a single MSCT scan.
Diagnosis and treatment of peripancreatic infection
In order to facilitate early diagnosis and prevention of peripancreatic infection, as well as to provide timely treatment, we performed percutaneous punctures on suspicious lesions around the pancreas under ultrasound or CT guidance, followed by drainage and continuous irrigation. The location and size of the abscess were identified through ultrasound or CT scans, and the optimal puncture angle, plane, and needle entry point were selected. The needle position was observed and adjusted under the guidance of ultrasound or CT, and then the needle tip was withdrawn from the abscess and placed with a drainage tube. If the fluid obtained after drainage or irrigation tested positive for bacterial cultures, it confirmed the presence of peripancreatic infection. All patients received nutritional support, gastrointestinal decompression, fasting, oxygen therapy, anti-inflammatory treatment, and continuous fluid protein infusion. If symptoms did not improve, additional treatments such as percutaneous drainage under CT guidance, laparoscopic cholecystectomy, common bile duct incision drainage, and surgical debridement for peripancreatic infection were performed promptly.
Clinical outcomes
This study compared the MSCT perfusion imaging parameters between elderly SAP patients with and without peripancreatic infection. It analyzed the value of MSCT perfusion imaging parameters in assessing the risk of peripancreatic infection. The optimal cut-off value for evaluating peripancreatic infection was recorded for each parameter, and the sensitivity, specificity, area under the curve (AUC), and 95% confidence interval (95% CI) for evaluating peripancreatic infection were calculated for each parameter.
Statistical analysis
This study utilized SPSS 25.0 software for data statistical analysis. The measured data followed a normal distribution with equal variances. It was described using the mean plus or minus the standard deviation, and a group-based t-test is performed. Count data were described using percentages and subjected to a Chi-square test. To assess the value of MSCT perfusion imaging parameters in evaluating the risk of peripancreatic infection in elderly SAP patients, ROC curve analysis was performed, and the AUC was compared using a nonparametric rank-sum test. When the P value is less than 0.05, the difference is statistically significant.
| Results | ▴Top |
The incidence and prognosis of pancreatic/peripancreatic infection in 110 elderly patients with systemic inflammatory response syndrome (SIRS)
This study included a total of 110 elderly patients with SAP, including 69 males and 41 females, with a mean age of 74.52 ± 5.16 years (ranging from 60 to 86 years). The average length of hospital stay was 15.60 ± 4.10 days (ranging from 8 to 20 days). The mean Acute Physiology and Chronic Health Evaluation (APACHE II) score was 15.56 ± 2.60. Among the 110 elderly SAP patients, the incidence of peripancreatic infection was 20.91% (23/110), and the case fatality rate was 0.91% (1/110). Of the 23 elderly SAP patients with concomitant peripancreatic infection, 11 received conservative treatment, seven underwent percutaneous drainage guided by CT, four underwent laparoscopic cholecystectomy and drainage, and one received a combination of percutaneous drainage and laparoscopic cholecystectomy guided by CT. These patients showed improvement in symptoms and signs after treatment, with gradual reduction of abdominal pain, normalization of serum amylase and C-reactive protein (CRP) levels, and decreased peripancreatic exudate observed on CT scans, indicating resolution of peripancreatic infection. Only one patient died due to disease progression and multi-organ dysfunction.
In 87 elderly SAP patients with no pancreatic infection, 44 received conservative treatment, 29 received percutaneous catheter drainage under CT guidance, 11 underwent laparoscopic cholecystectomy + gallbladder drainage, and three received percutaneous catheter drainage under CT guidance + laparoscopic cholecystectomy. These patients have all been discharged after their condition improved due to symptomatic treatment.
Comparison of MSCT perfusion imaging parameters in elderly SAP patients with combined peripancreatic infection and without peripancreatic infection
MSCT perfusion imaging shows that after peripancreatic infection in 23 elderly SAP patients, the pancreatic density decreases, the pancreatic region enlarges, the pancreatic margins become blurred, and the presence of abdominal fluid. Among them, 22 patients experienced splenic vein compression/narrowing/occlusion, 17 experienced superior mesenteric vein compression/narrowing/occlusion, 19 had portal vein dilatation/thrombosis, and 21 had collateral circulation. Figure 1 shows the perfusion CT images of an elderly SAP patient with a combined pancreatic infection and another without a pancreatic infection.
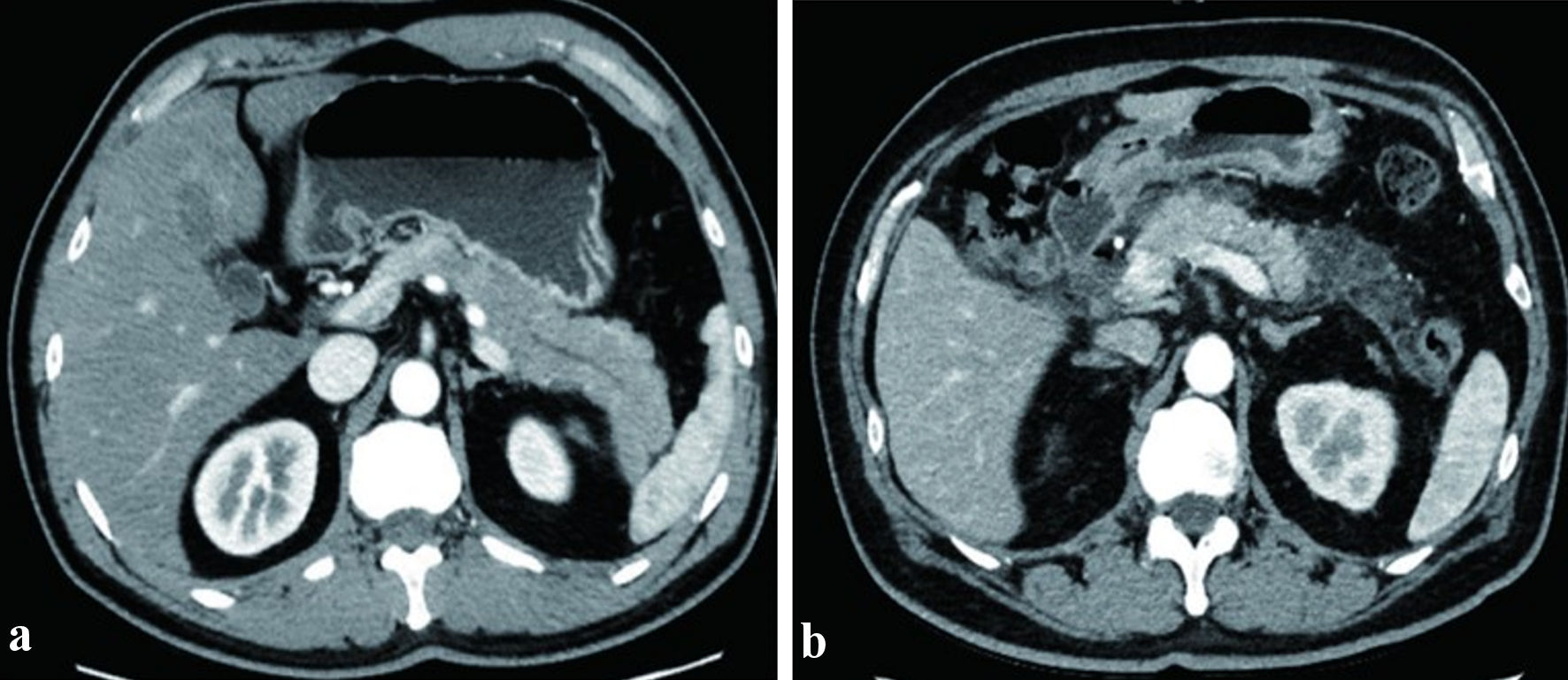 Click for large image | Figure 1. Representative MSCT perfusion imaging of elderly SAP patients. (a) MSCT perfusion imaging of a 67-year-old male SAP patient without peripancreatic infection. (b) MSCT perfusion imaging of a 65-year-old male SAP patient with concurrent peripancreatic infection. SAP: severe acute pancreatitis; MSCT: multi-slice spiral computed tomography. |
As shown in Table 1, compared with elderly patients with SAP without peripancreatic infection, elderly SAP patients with concomitant peripancreatic infection had a prolonged time to peak and decreased peak height, and reduced blood flow (all P < 0.05).
 Click to view | Table 1. Comparison of MSCT Perfusion Imaging Parameters Between Elderly SAP Patients with and Without Peripancreatic Infection |
Efficiency analysis of MSCT perfusion imaging parameters for evaluating the risk of peripancreatic infection in elderly patients with SAP
As shown in Figure 2 and Table 2, the results of ROC analysis indicated that when evaluating the risk of peripancreatic infection in elderly SAP patients, the specificity and AUC of the combination of three parameters (peak time, peak height, and blood flow) were higher than those of a single parameter (all P < 0.05). There was no significant difference in sensitivity between the combination of three parameters and a single parameter (all P > 0.05).
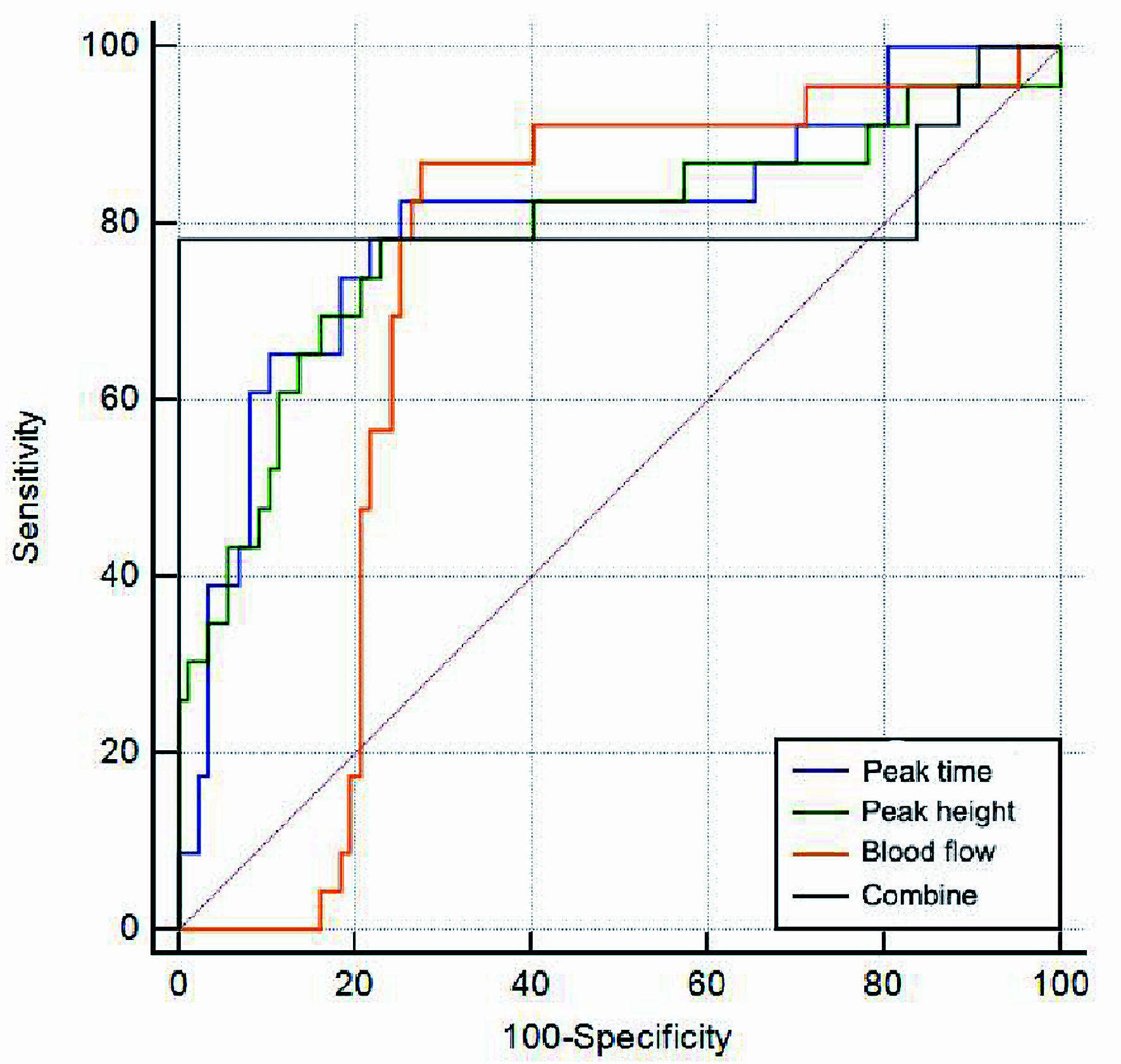 Click for large image | Figure 2. ROC curves for evaluating the risk of peripancreatic infection in elderly SAP patients using MSCT perfusion imaging parameters. SAP: severe acute pancreatitis; MSCT: multi-slice spiral computed tomography; ROC: receiver operating characteristic. |
 Click to view | Table 2. Evaluation of the Efficacy of Predicting the Risk of Peripancreatic Infection in Elderly SAP Patients Using Time to Peak, Peak Height, and Blood Flow Volume, Either Individually or in Combination, From MSCT Perfusion Imaging |
| Discussion | ▴Top |
SAP is a complex condition with various etiological factors, including obstruction, alcohol-induced inflammation, vascular embolisms, metabolic disorders (e.g., hypercalcemia and hyperlipidemia), and trauma. These factors can trigger inflammatory exudation and infection in the pancreatic tissues, significantly increasing mortality risk [14]. Currently, clinical diagnosis of SAP in elderly individuals primarily relies on imaging modalities, notably CT and MRI [15]. CT utilizes precise collimated X-ray beams, gamma rays, and ultrasound for rapid, slice-by-slice scans of specific body areas, offering clear images and immediate results [16]. Conversely, MRI employs external magnetic field gradients to detect emitted electromagnetic waves, enabling precise lesion detection and assessment of lesion extent and edema [17]. In cases of severe pancreatitis, CT typically reveals diffuse or localized pancreatic enlargement with reduced density and thickening of the surrounding fascial area, often accompanied by localized exudation. In contrast, MRI predominantly shows localized or widespread pancreatic enlargement with indistinct contours, accompanied by peripancreatic features such as exudation, bleeding, and mixed long T1 and T2 signal intensities [18]. However, the diagnostic accuracy of CT and MRI may be compromised by the presence of typical symptoms in severe pancreatitis, including bleeding and exudation, as well as anatomical complexities such as the pseudo-pancreatic head and tail [19]. Consequently, CT and MRI may have limited utility in diagnosing severe pancreatitis and providing guidance for clinical treatment [19]. Additionally, the Ranson score and APACHE II score are commonly used in clinical practice to diagnose the condition of patients with SAP. However, these scoring systems require a prolonged time of 48 h or more, lacking practicality in early diagnosis. Furthermore, elderly SAP patients are at increased risk of developing complications, notably pancreatic infection, which can be life-threatening [20]. Thus, exploring innovative techniques to enhance the assessment accuracy of pancreatic/peripancreatic infection in elderly SAP patients is essential [20]. Currently, MSCT is not a widely used diagnostic or management method for SAP. However, a considerable body of research has shown that MSCT perfusion imaging can clearly visualize the characteristics of lesions and vascular changes in cases of pancreatitis. MSCT has a certain value in assessing the severity of SAP and diagnosing complications such as acute kidney injury [21].
In our study, we utilized MSCT perfusion imaging to assess its diagnostic potential. The elderly SAP patients in our study exhibited typical radiological features during the MSCT perfusion imaging process, consistent with prior reports from domestic and international sources [22]. In our study, the incidence of peripancreatic infection was 20.91%, with one patient succumbing to it, resulting in a mortality rate of 0.91%. Earlier studies have reported peripancreatic infection incidence rates of approximately 30% in SAP patients, with mortality rates around 8% [23]. Our study’s lower incidence and mortality rates of pancreatic infection in elderly SAP patients could be attributed to variations in baseline patient characteristics, treatment strategies, and intervention measures.
MSCT perfusion imaging is an advanced technique that relies on contrast agent diffusion principles and mathematical modeling to calculate perfusion parameters [22]. It assesses tissue perfusion by quantifying the difference between arterial inflow and venous outflow rates in terms of contrast agent accumulation in tissues and organs [24]. This principle can be utilized to measure perfusion parameters of tissues, effectively and quantitatively reflecting changes in local tissue blood perfusion, particularly in pancreatic and liver tissues. Consequently, it can be employed to evaluate tissue pathological changes and inflammatory infiltration [25]. Prior studies have indicated significant inflammatory exudate presence in patients with SAP-related pancreatic infection, affecting tissue perfusion, blood supply, and increasing the risk of pancreatic necrosis [26]. In our study, elderly SAP patients with concurrent peripancreatic infection exhibited prolonged time to peak, reduced peak height, and decreased blood flow compared to those without infection during MSCT perfusion imaging. These findings suggest that these three MSCT perfusion imaging parameters could serve as valuable indicators for assessing the risk of pancreatic/peripancreatic infection in elderly SAP patients.
Additionally, in our study, we determined specific threshold values for peak time, peak height, and critical blood flow in elderly SAP patients with peripancreatic infection, measuring at 24.15 s, 62.03 Hounsfield units, and 916.82 mL/min/g, respectively. These parameters demonstrated excellent predictive value, with respective AUC values of 0.804, 0.787, and 0.719. Importantly, peak time primarily reflects the time elapsed from the initiation of dynamic contrast agent injection to the point at which the signal reaches its zenith, offering insights into vascular resistance, blood volume, and blood flow [27]. Peak height, on the other hand, represents the maximal enhancement value within the lesion, aiding in characterizing the lesion’s nature [28]. Blood flow provides critical information about blood supply to pathological tissues and serves as a key parameter for assessing the lesion’s condition [29]. In elderly SAP patients with concurrent peripancreatic infection, the severity of tissue damage due to infection likely increases vascular resistance, reduces peak enhancement, and compromises blood flow [20].
Furthermore, in our study, we evaluated the sensitivity of combined parameters for assessing peripancreatic infection in elderly SAP patients, which was found to be equivalent to that of single parameters. However, the specificity and AUC of combined parameters, namely peak time, peak height, and blood flow rate, were significantly higher than those of single parameters. These results underscore the diagnostic efficacy of combining these parameters derived from MSCT perfusion imaging in assessing the risk of peripancreatic infection in elderly SAP patients [30].
The scientific significance of our study lies in its exploration of the diagnostic potential of MSCT perfusion imaging for evaluating peripancreatic infection in elderly SAP patients. While peripancreatic infection is a common complication in SAP, conventional imaging approaches often fall short of enabling early diagnosis. By harnessing MSCT perfusion imaging, our study identified characteristic features of peripancreatic infection, including decreased pancreatic density, pancreatic enlargement, blurred pancreatic contours, and the presence of ascites. Moreover, we established correlations between MSCT perfusion imaging parameters and the occurrence of peripancreatic infection. Through ROC analysis, we demonstrated that combining the parameters of peak time, peak height, and blood flow significantly improves predictive accuracy for the risk of peripancreatic infection.
From a clinical standpoint, the findings of our study hold substantial clinical value in enhancing the precision of diagnosis and intervention outcomes for elderly SAP patients. Early detection of peripancreatic infection enables the timely implementation of interventions, including antibiotic therapy, drainage procedures, and surgical interventions, thereby reducing the risk of infection spread and associated complications. With its noninvasive and reproducible nature, MSCT perfusion imaging offers an effective means to diagnose peripancreatic infection accurately. It provides a foundation for personalized treatment strategies by evaluating the perfusion kinetic parameters of the pancreas.
However, this study has several limitations. Firstly, it is a single-center retrospective study with a relatively small sample size. Further multicenter, large-scale prospective studies are still needed to validate the results of this study. Secondly, this study focused only on elderly patients with SAP, and whether the findings are applicable to patients in other age groups requires further investigation. Furthermore, although MSCT perfusion imaging has demonstrated good efficacy in the diagnosis of peripancreatic infection, the widespread application of this technique needs to consider factors such as cost-effectiveness, radiation dose, and technical difficulty. Additionally, this study only included patients who received MSCT perfusion imaging, which may introduce some selection bias. Therefore, before implementing this technique in clinical practice, further evaluation of the balance between risks and benefits is necessary.
Future research endeavors should delve deeper into the potential of MSCT perfusion imaging in assessing peripancreatic infection in elderly SAP patients. Comparative assessments with alternative imaging methods, including ultrasound and MRI, could substantiate its accuracy and feasibility. Additionally, exploring the integration of MSCT perfusion imaging with clinical markers and other diagnostic modalities, such as inflammatory biomarkers, could further enhance the comprehensiveness and accuracy of peripancreatic infection diagnosis. Moreover, efforts should be directed toward standardizing MSCT perfusion imaging parameters and establishing universally accepted thresholds, thereby facilitating its widespread adoption across diverse healthcare institutions and clinical contexts.
In conclusion, our study findings strongly suggest that MSCT perfusion imaging harbors significant diagnostic potential for evaluating peripancreatic infection in elderly SAP patients (Fig. 3). However, continued research is indispensable to validate and optimize its practical utility while addressing pertinent limitations and challenges. Through ongoing endeavors, we anticipate that MSCT perfusion imaging will emerge as a valuable tool, providing enhanced support for the diagnosis and management of elderly SAP patients, thereby improving patient prognosis and enhancing their quality of life.
 Click for large image | Figure 3. Efficacy of predicting the risk of peripancreatic infection in elderly patients with severe acute pancreatitis using MSCT perfusion imaging. MSCT: multi-slice spiral computed tomography; AUC: area under the curve. |
Acknowledgments
Not applicable.
Financial Disclosure
Not applicable.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
For this study, the IRB adopted the requirements for patient consent for publication. The study posed minimal risk to participants and used deidentified data in accordance with the guidelines established by this IRB.
Author Contributions
Rui Hao and Yu Sun designed the study. Rui Hao, Yu Sun and Yang Hu collated the data, designed and developed the database, carried out data analyses and produced the initial draft of the manuscript. Rui Hao and Yu Sun contributed to drafting the manuscript. All authors have read and approved the final submitted manuscript.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
SAP: severe acute pancreatitis; MSCT: multi-slice spiral computed tomography; AUC: area under the curve; SIRS: systemic inflammatory response syndrome
| References | ▴Top |
- Szatmary P, Grammatikopoulos T, Cai W, Huang W, Mukherjee R, Halloran C, Beyer G, et al. Acute pancreatitis: diagnosis and treatment. Drugs. 2022;82(12):1251-1276.
doi pubmed pmc - Jablonska B, Mrowiec S. Nutritional support in patients with severe acute pancreatitis-current standards. Nutrients. 2021;13(5):1498.
doi pubmed pmc - Valverde-Lopez F, Martinez-Cara JG, Redondo-Cerezo E. Acute pancreatitis. Med Clin (Barc). 2022;158(11):556-563.
doi pubmed - Gomes CA, Di Saverio S, Sartelli M, Segallini E, Cilloni N, Pezzilli R, Pagano N, et al. Severe acute pancreatitis: eight fundamental steps revised according to the 'PANCREAS' acronym. Ann R Coll Surg Engl. 2020;102(8):555-559.
doi pubmed pmc - McCarty TR, Garg R, Rustagi T. Pancreatic cyst fluid glucose in differentiating mucinous from nonmucinous pancreatic cysts: a systematic review and meta-analysis. Gastrointest Endosc. 2021;94(4):698-712.e696.
doi pubmed - Liang JX, Bi XJ, Li XM, Gao ZL, Suo F, Cui EG, Li HF, et al. Evaluation of multislice spiral computed tomography perfusion imaging for the efficacy of preoperative concurrent chemoradiotherapy in middle-aged and elderly patients with locally advanced gastric cancer. Med Sci Monit. 2018;24:235-245.
doi pubmed pmc - Virostko J. Quantitative magnetic resonance imaging of the pancreas of individuals with diabetes. Front Endocrinol (Lausanne). 2020;11:592349.
doi pubmed pmc - Tsuji Y, Takahashi N, Isoda H, Koizumi K, Koyasu S, Sekimoto M, Imanaka Y, et al. Early diagnosis of pancreatic necrosis based on perfusion CT to predict the severity of acute pancreatitis. J Gastroenterol. 2017;52(10):1130-1139.
doi pubmed - Simon R. Complications after pancreaticoduodenectomy. Surg Clin North Am. 2021;101(5):865-874.
doi pubmed - Tsuji Y, Yamamoto H, Yazumi S, Watanabe Y, Matsueda K, Yamamoto H, Chiba T. Perfusion computerized tomography can predict pancreatic necrosis in early stages of severe acute pancreatitis. Clin Gastroenterol Hepatol. 2007;5(12):1484-1492.
doi pubmed - Saneesh PS, Garga UC, Gupta AK, Yelamanchi R. Role of multi-detector computed tomography in severity assessment of cases of acute pancreatitis. Wien Klin Wochenschr. 2021;133(13-14):654-660.
doi pubmed - Li H, Wu Y, Xu C, An H, Guo C, Cui H. Early ultrasound-guided percutaneous catheter drainage in the treatment of severe acute pancreatitis with acute fluid accumulation. Exp Ther Med. 2018;16(3):1753-1757.
doi pubmed pmc - Lu X, Gao J, Huang YG, Gu ML. CT-guided puncture and drainage for the treatment of severe acute pancreatitis: A case report. Asian J Surg. 2023;46(9):3978-3979.
doi pubmed - Lu WW, Chen X, Ni JL, Zhu SL, Fei AH, Wang XS. The role of gut microbiota in the pathogenesis and treatment of acute pancreatitis: a narrative review. Ann Palliat Med. 2021;10(3):3445-3451.
doi pubmed - Guayara-Quinn CG, Pare N, Scott RL, Sepulveda CA, Katz MJ, Lipton RB, Schaefer LA, et al. Development and psychometric evaluation of the Test of Practical Judgment alternate form (Form B). Appl Neuropsychol Adult. 2023;30(2):176-185.
doi pubmed pmc - Tatsugami F, Higaki T, Nakamura Y, Honda Y, Awai K. Dual-energy CT: minimal essentials for radiologists. Jpn J Radiol. 2022;40(6):547-559.
doi pubmed pmc - O'Shea A, Harisinghani M. PI-RADS: multiparametric MRI in prostate cancer. MAGMA. 2022;35(4):523-532.
doi pubmed - Mekheal N, Roman S, Alkomos MF, Mekheal E, Farokhian A, Millet C, Shah H, et al. Hemosuccus pancreaticus: challenging diagnosis and treatment. Eur J Case Rep Intern Med. 2022;9(5):003337.
doi pubmed pmc - Amblee A, Mohananey D, Morkos M, Basu S, Abegunde AT, Ganesh M, Bhalerao N, et al. Acute pancreatitis in patients with severe hypertriglyceridemia in a multi-ethnic minority population. Endocr Pract. 2018;24(5):429-436.
doi pubmed - Zhang Q, Zeng R, Tang X. Application value and safety of NIPPV combined with routine clearance in the treatment of stroke-associated pneumonia in elderly patients. Am J Transl Res. 2022;14(11):7860-7869.
pubmed pmc - Li ZY, Zhang L, Jin T, Huang ZX, Song B, Wu B, Zhang WW, et al. Correlation analysis of computed tomography imaging scoring to the presence of acute kidney injury in severe acute pancreatitis. Sichuan Da Xue Xue Bao Yi Xue Ban. 2011;42(5):695-698.
pubmed - Li Q, Cui D, Feng Y, He Y, Shi Z, Yang R. Correlation between microvessel density (MVD) and multi-spiral CT (MSCT) perfusion parameters of esophageal cancer lesions and the diagnostic value of combined CtBP2 and P16(INK4A). J Gastrointest Oncol. 2021;12(3):981-990.
doi pubmed pmc - Guo D, Dai W, Shen J, Zhang M, Shi Y, Jiang K, Guo L. Assessment of prophylactic carbapenem antibiotics administration for severe acute pancreatitis: an updated systematic review and meta-analysis. Digestion. 2022;103(3):183-191.
doi pubmed - Tun WM, Poologasundarampillai G, Bischof H, Nye G, King ONF, Basham M, Tokudome Y, et al. A massively multi-scale approach to characterizing tissue architecture by synchrotron micro-CT applied to the human placenta. J R Soc Interface. 2021;18(179):20210140.
doi pubmed pmc - Garbino N, Brancato V, Salvatore M, Cavaliere C. A systematic review on the role of the perfusion computed tomography in abdominal cancer. Dose Response. 2021;19(4):15593258211056199.
doi pubmed pmc - Yasuda H, Horibe M, Sanui M, Sasaki M, Suzuki N, Sawano H, Goto T, et al. Etiology and mortality in severe acute pancreatitis: A multicenter study in Japan. Pancreatology. 2020;20(3):307-317.
doi pubmed - Walsh BT, Xu T, Wang Y, Attia E, Kaplan AS. Time course of relapse following acute treatment for anorexia nervosa. Am J Psychiatry. 2021;178(9):848-853.
doi pubmed pmc - Rudisill SS, Kucharik MP, Varady NH, Martin SD. Evidence-based management and factors associated with return to play after acute hamstring injury in athletes: a systematic review. Orthop J Sports Med. 2021;9(11):23259671211053833.
doi pubmed pmc - Behar-Cohen F, Gelize E, Jonet L, Lassiaz P. [Anatomy of the retina]. Med Sci (Paris). 2020;36(6-7):594-599.
doi pubmed - de Laat-Kremers R, Di Castelnuovo A, van der Vorm L, Costanzo S, Ninivaggi M, Cerletti C, Huskens D, et al. Increased BMI and blood lipids are associated with a hypercoagulable state in the Moli-sani Cohort. Front Cardiovasc Med. 2022;9:897733.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


