| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 17, Number 2, April 2024, pages 90-99
Mucosa-Associated Lymphoid Tissue Surgeries as a Possible Risk for Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis
Rutvi Amina, q , Aditya Mansabdarb, q
, Hyundam Guc, Bhavani Ganginenid, Neev Mehtae, Harini Patelf, Neel Patelg, Srishti Lallerh, Suprada Vinayaki, Mohammed Ali Abdulqaderj, Hardik Jaink, Amitjeet Singh Rekhrajl, Harshini Adimoulamem, Gurinder Singhn, Jose Moonjely Daviso, Urvish Patelg, Harmeet Gillp
aDepartment of Medicine, Surat Municipal Institute of Medical Education and Research, Surat, Gujarat 395010, India
bDepartment of Medicine, First Faculty of Medicine, Charles University, Prague 12108, Czechia
cDepartment of Internal Medicine, Yeouido St. Mary’s Hospital, The Catholic University of Korea College of Medicine, Seoul 07345, Korea
dDepartment of Internal Medicine, Guntur Medical College, Guntur, Andhra Pradesh 522004, India
eDepartment of Medicine, Lahey Hospital and Medical Center, Burlington, MA 01805, USA
fDepartment of Medicine, Gujarat Medical Educational and Research Society (GMERS), Himmatnagar, Gujarat 383001, India
gDepartment of Public Health, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA
hDepartment of Internal Medicine, Sutter Roseville Medical Center, Roseville, CA 95661, USA
iDepartment of Internal Medicine, Wellmont Health Systems/Ballad Health, VA 24273, USA
jDepartment of Internal Medicine-Pediatrics, Geisinger Med Center, Danville, PA 17822, USA
kGovernment Medical College, Gujarat, India
lDepartment of Medicine, Lyell McEwin Hospital, Elizabeth Vale, SA 5112, Australia
mJawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry 605006, India
nDepartment of Clinical and Medical Sciences, Universidad Especializada de las Americas, Panama 0849-0141, Panama
oAlbert Einstein College of Medicine, New York, NY 10461, USA
pDepartment of Medicine, HopeHealth, Florence, SC 29501, USA
qCorresponding Author: Rutvi Amin, Department of Medicine, Surat Municipal Institute of Medical Education and Research, Surat, Gujarat 395010, India; Aditya Mansabdar, Department of Medicine, First Faculty of Medicine, Charles University, Prague 12108, Czechia
Manuscript submitted September 4, 2023, accepted March 27, 2024, published online April 30, 2024
Short title: MALTectomy and Its Association With IBD
doi: https://doi.org/10.14740/gr1672
| Abstract | ▴Top |
Background: Inflammatory bowel disease (IBD) is a group of chronic inflammatory gastrointestinal disorders that are caused by genetic susceptibility and environmental factors and affects a significant portion of the global population. The gut-associated lymphoid tissue (GALT) is known to play a crucial role in immune modulation and maintaining gut microbiota balance. Dysbiosis in the latter has a known link to IBD. Therefore, the increasing prevalence of adenoidectomy in children should be explored for its potential association with IBD. The objective of this paper was to assess the association between adenoid tissue removal and the risk of developing Crohn’s disease (CD) and ulcerative colitis (UC).
Methods: We conducted a pooled meta-analysis to evaluate the extended clinical outcomes in patients who underwent appendicectomy and tonsillectomy compared to those who did not. Our approach involved systematically searching the PubMed database for relevant observational studies written in English. We followed the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines to collect data from various time periods, and to address the diversity in study results; we employed a random-effects analysis that considered heterogeneity. For outcomes, odds ratios (ORs) were pooled using a random-effects model.
Results: Seven studies, out of a total of 114,537, met our inclusion criteria. Our meta-analysis revealed a significant association between appendicectomy and CD (OR: 1.57; 95% confidence interval (CI): 1.01 - 2.43; heterogeneity I2 = 93%). Similarly, we found a significant association between tonsillectomy and CD (OR: 1.93; 95% CI: 0.96 - 3.89; I2 = 62%). However, no significant association was observed between appendicectomy and UC (OR: 0.60; 95% CI: 0.24 - 1.47; I2 = 96%), while a modest association was found between tonsillectomy and UC (OR: 1.24; 95% CI: 1.18 - 1.30; I2 = 0%).
Conclusions: In summary, we found that the trend of appendicectomy is linked to higher odds of CD, and tonsillectomy is more likely associated with increased odds for both CD and UC, with a risk of bias present.
Keywords: Mucosa-associated lymphoid tissue surgeries; MALTectomy; Appendectomy; Tonsillectomy; Inflammatory bowel disease; Ulcerative colitis; Crohn’s disease
| Introduction | ▴Top |
Inflammatory bowel disease (IBD) encompasses a group of chronic gastrointestinal disorders characterized by remitting and relapsing inflammation in the digestive tract. The burden of IBD is increasing worldwide, with an estimated prevalence of more than 0.3% of the population in Western countries, especially in North America, Oceania, and Europe [1], along with increasing trend in Asia and South America. It presents with a wide variety of symptoms, including anemia, weight loss, abdominal pain, diarrhea, and rectal bleeding [2]. Crohn’s disease (CD) and ulcerative colitis (UC) are subtypes of IBD, and these conditions significantly impact the quality of life of affected individuals. Extensive research has been conducted over the years to understand the etiology of IBD, which is now recognized as multifactorial, involving a combination of genetic susceptibility and environmental factors [2].
The mucosa-associated lymphoid tissue (MALT) is the largest lymphoid compartment in the human body [3]. Depending on its anatomical position, it can be classified into various subgroups; bronchus-associated, conjunctiva-associated, gut-associated, larynx-associated, and nose-associated lymphoid tissues [4]. Gut-associated lymphoid tissue (GALT) consists of multi follicular structures like tonsils, Peyer’s patches, appendix, colonic and cecal patches, and numerous smaller, single follicular structures called isolated lymphoid follicles (ILF) [5]. It plays a crucial role in immune modulation and preserving the balance of the gut microbiota [6]. The gut microbiota provides various benefits to humans, including pathogen protection, nutrition, and support for the immune system. To maintain good human health, the gut microbiota and the human host engage in various symbiotic interactions. However, dysbiosis, a condition characterized by alterations in the function and composition of the gut microbiota, can disrupt this delicate balance. Although many studies have reported disrupted microbiota in patients with IBD, a direct relationship has not yet been firmly established [7-11]. The prevalence of adenoidectomy in children is also increasing, from 370/100,000 in 1996 to 687/100,000 in 2006 [12]. Thus, establishing an association between such surgical procedures and IBD becomes even more important.
In this article, our objectives were twofold: 1) to review and synthesize the currently available data on the association between mucosa-associated lymphoid tissue removal (MALTectomy) and IBD; 2) to highlight potential biases in the existing data and discuss existing knowledge gaps. By accomplishing these objectives, we aimed to provide a comprehensive overview of the current understanding of the relationship between MALTectomy and IBD and identify areas in research that require further exploration.
| Materials and Methods | ▴Top |
Endpoints
We planned a meta-analysis of previously published prospective and retrospective human studies. We aimed to determine a connection between MALTectomy and IBD. We defined MALTectomy as appendectomy or tonsillectomy and IBD as UC or CD. For our study, we selected patients with IBD as our patient population, and the intervention we looked for was appendectomy or tonsillectomy, while the control group consisted of patients without IBD.
Search strategy
In adherence to the Preferred Reporting Items for Systematic Reviews and Meta Analysis (PRISMA) guidelines and Meta-analysis of Observational Studies in Epidemiology (MOOSE) protocols, a systematic review and meta-analysis was conducted on existing literature. The study focused on comparing the outcomes of UC and CD following tonsillectomy or appendectomy. Relevant articles were identified through a comprehensive search using PubMed and targeted keywords ((“Inflammatory Bowel Disease” (Title/Abstract) OR “IBD” (Title/Abstract) OR “Crohn’s disease” (Title/Abstract) OR “Ulcerative colitis” (Title/Abstract)) AND (“adenoidectomy” (Title/Abstract) OR “MALT-ectomy” (Title/Abstract) OR “appendicectomy” (Title/Abstract) OR “tonsillectomy” (Title/Abstract) OR “lymphoid tissue” (Title/Abstract) OR “GALT-ectomy” (Title/Abstract).
Inclusion criteria
Our study focused on observational studies that involved patients with IBD who had undergone an appendectomy or tonsillectomy. We included studies covering all age groups in our research. We included all the articles present in PubMed without using a timeline filter.
Exclusion criteria
Studies other than observational studies, non-human, non-English, and non-full text studies were excluded from quantitative analysis.
Study selection
We utilized certain eligibility criteria and relevant keywords to screen and evaluate abstracts that would be included in our systematic review and Meta-analysis. The abstracts were independently screened by RA, AM, and HG. Furthermore, any disagreements were resolved by UP. Full length articles that met the screening criteria from the abstracts were obtained, and each of them were evaluated.
Data extraction
Data on study name, year of study, study design, population of interest (i.e., IBD and non-IBD patients), study sample (number of patients with UC, CD and no IBD), surgical procedures (i.e., patients with either UC or CD who had undergone appendectomy or tonsillectomy), outcomes and conclusion were collected by BG and HP using standard template, and any disagreement was resolved by HG and UP. The data extraction process involved using an Excel sheet to collect information from the included studies for article assessment. The form was carefully designed in collaboration with the biostatistician and methodologist on the team NM and NP. Table 1 [13-19] shows the data we collected for this article.
 Click to view | Table 1. Summaries of Study Findings Association Between Surgical Procedures and IBD |
Quality assessment
The Newcastle-Ottawa scale (NOS) criteria were selected to assess the quality of the included studies. The highest score on the NOS scale is 9 points. Articles with high quality scores receive 7 points or more; articles with medium quality scores receive 4 to 6 points; articles with low-quality scores receive less than 3 points. Each section of NOS is assessed according to these criteria: 1) Selection: representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, demonstration that outcome of interest was not present at the start of the study; 2) Comparability: comparability of cohorts based on the design or analysis; 3) Outcome: assessment of outcome, follow-up longevity, adequacy of follow-up of cohorts.
Statistical analysis
Excel sheet was used to collect the data and Review Manager version 5.3 software was used to analyze the data. We performed inverse variance technique and random effects models to estimate the pooled effect size (pooled odds ratio (OR)) and 95% confidence interval (95% CI). Forest plots and funnel plots were obtained. P < 0.05 was considered statistically significant. All statistical analyses were carried out using Review Manager 5.4.
Ethical approval
Institutional Review Board (IRB) approval was not needed for this study. Though this article does not contain any studies with direct involvement of human participants or animals performed by any of the authors, all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
| Results | ▴Top |
We identified 114,537 articles on IBD and MALT surgeries on PubMed. Out of these, 270 studies had detailed post procedure history of IBD. After excluding studies, we found 23 observational studies fitting in the eligibility for the qualitative and quantitative assessment. After a detailed assessment, a total of six studies were selected to evaluate the quantitative outcomes. The detailed selection process was shown in Figure 1. Table 2 [13, 15-19] describes the risk of bias assessment by NOS.
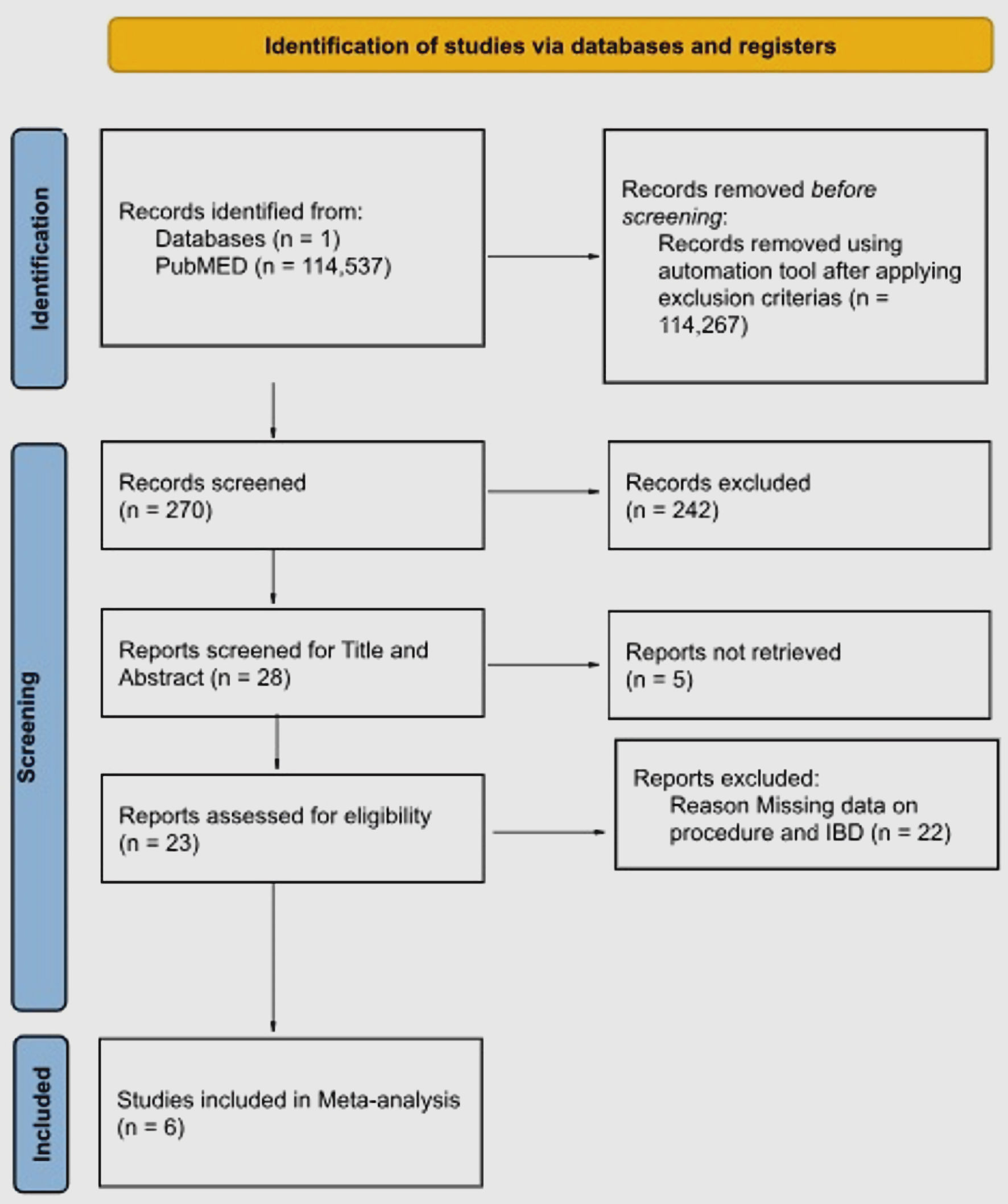 Click for large image | Figure 1. PRISMA flow diagram showing study selection. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta Analysis. |
 Click to view | Table 2. Newcastle-Ottawa Scale |
Outcomes
CD and appendicectomy
We found six observational studies that evaluated the effect of appendicectomy on possible risk of CD. Our meta-analysis (Fig. 2a) shows that patients with appendicectomy had a 53% higher chance of CD as compared to without appendicectomy (pooled OR: 1.57, 95% CI: 1.01 - 2.43; P < 0.00001). Heterogeneity was substantial at 93% (P < 0.00001).
 Click for large image | Figure 2. The association between MALTectomy (appendicectomy/tonsillectomy) and Crohn’s disease. (a) Forest plot of the association between MALTectomy (appendicectomy/tonsillectomy) and Crohn’s disease. (b) Funnel plot of the association between MALTectomy (appendicectomy/tonsillectomy) and Crohn’s disease. SE: standard error; CI: confidence interval; MALTectomy: mucosa-associated lymphoid tissue removal; OR: odds ratio. |
CD and tonsillectomy
We analyzed two observational studies that examined the relationship between the history of tonsillectomy and its link to developing CD. Figure 2a demonstrates our findings, indicating a 24% higher CD association in those with tonsillectomy (pooled OR: 1.93, 95% CI: 0.96 - 3.89; P < 0.00001), with no significant heterogeneity (62%; P < 0.00001).
UC and appendicectomy
We examined five observational studies on appendicectomy’s impact on UC risk. Figure 3a suggests a 40% lower UC likelihood after appendicectomy (pooled OR: 0.60, 95% CI: 0.24 - 1.47; P < 0.00001), despite high study variation (heterogeneity: 96%, P < 0.00001).
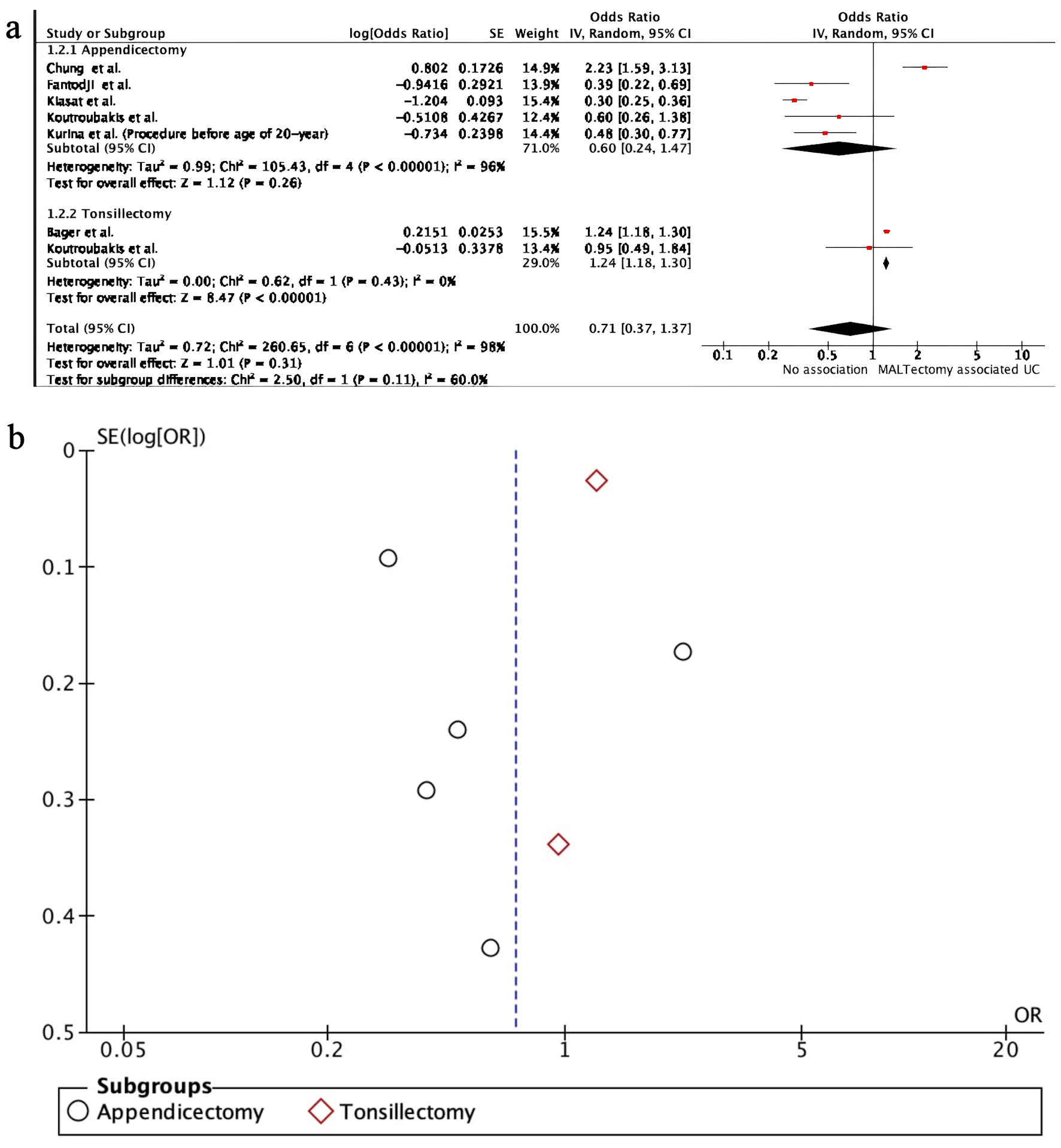 Click for large image | Figure 3. The association between MALTectomy (appendicectomy/tonsillectomy) and ulcerative colitis. (a) Forest plot of the association between MALTectomy (appendicectomy/tonsillectomy) and ulcerative colitis. (b) Funnel plot of the association between MALTectomy (appendicectomy/tonsillectomy) and ulcerative colitis. SE: standard error; CI: confidence interval; MALTectomy: mucosa-associated lymphoid tissue removal; OR: odds ratio. |
UC and tonsillectomy
We reviewed two observational studies investigating tonsillectomy’s link to UC. As shown in Figure 3a, results reveal a 24% increased likelihood of UC development post tonsillectomy compared to those without (pooled OR: 1.24, 95% CI: 1.18 - 1.30; P < 0.00001). Heterogeneity was absent (0%, P < 0.00001).
| Discussion | ▴Top |
In this study, our objective was to investigate the potential association between MALTectomy (MALT removal) and the occurrence of IBD. We categorized MALTectomy into two specific types: appendectomy and tonsillectomy. IBD encompasses CD and UC. Our primary finding indicates a positive association between the development of CD in patients with a prior MALTectomy. Similarly, there was a positive association between the development of UC in patients with a prior tonsillectomy. However, no significant association was observed between UC and prior appendicectomy.
The positive findings of our study of tonsillectomy and its association with CD are supported by various studies. For instance, Koutroubaki et al demonstrated a 229-fold increased likelihood of CD development in patients with a history of tonsillectomy, compared to those without the procedure [13]. Similarly, Sun et al reported a 37-fold elevated chance, and Bager et al found a 1.52-fold higher risk of CD in individuals with a history of tonsillectomy [15, 20].
With appendicectomy, our study identified a positive link with CD development, which is supported by various studies. Kurina et al. reported a 1.92-fold heightened risk of CD in patients with a history of appendicectomy [16]. Chen et al found a 1.878-fold higher likelihood, while Chung et al. reported a 3.48-fold increased risk [17, 18]. Fantodji et al also observed a 2.02-fold elevated risk of CD development in patients with a history of appendicectomy [19].
In summation, the pooled odds ratio (OR) for CD in our meta-analysis was 1.63 (95% CI: 1.23 - 2.16; I2: 0%), indicating a positive association between MALTectomy and CD (Fig. 2a, b).
A similar positive association between tonsillectomy and the risk of UC development was also evident, as indicated by the study of Bager et al, who reported a 1.24-fold elevated risk of UC in individuals with a prior tonsillectomy [15]. However, the pooled OR for UC, was 0.71 (95% CI: 0.37 - 1.37; I2: 60%), indicating no such association between MALTectomy and UC (Fig. 3a, b).
Strengths and limitations
Our meta-analysis encompassed a diverse set of seven studies from various geographic regions, including Denmark, China, England, and Sweden. This diversity underscores the broad applicability of our findings to different populations. Our inclusion criteria were precise, encompassing patients who had undergone either tonsillectomy or appendicectomy and subsequently developed IBD (CD or UC), ensuring the study’s specificity. We also performed comprehensive literature searches across multiple databases to guarantee inclusivity.
However, despite the strengths of our analysis, there were certain limitations. Data-specific limitations include the lack of complete data in some studies, potentially limiting the scope and comprehensiveness of our analysis. Language and regional biases could lead to the omission of studies published in languages different from the one in which the meta-analysis was conducted. There was also significant degree of heterogeneity between researches and moderate degree of risk of bias.
Project-specific limitations encompassed the exclusion of other mucosal tissues (e.g., bronchial, gastric, nasal) from analysis, the absence of consideration for the time duration between the procedure and IBD development, and the omission of disease severity as a factor in comparison with IBD development in patients without MALTectomy.
Future research is essential to elucidate specific underlying mechanisms, contributing to early diagnosis and targeted treatment strategies. Furthermore, exploring associations between the removal of other adenoid tissues and the risk of IBD development would enhance our understanding of the relationship between surgical procedures and IBD outcomes, offering a more comprehensive perspective.
Conclusions
In conclusion, our meta-analysis suggests a potential positive relationship between the following procedures and IBD (CD and UC): tonsillectomy and appendicectomy with CD.
Acknowledgments
None to declare.
Financial Disclosure
The study had no internal or external funding source.
Conflict of Interest
Authors declare no conflict of interest.
Informed Consent
The data used in this study are de-identified from PubMed, so informed consent was not needed for this study.
Author Contributions
Conceptualization: Rutvi Amin and Neev Mehta. Methodology: Aditya Mansabdar, Neev Mehta, and Neel Patel. Acquisition of data: Bhavani Gangineni, Harini Patel, and Amitjeet Singh Rekhraj. Software: Rutvi Amin, Aditya Mansabdar, Bhavani Gangineni, Urvish Patel, and Gurinder Singh. Formal analysis and investigation: Rutvi Amin, Aditya Mansabdar, Hyundam Gu, Neel Patel, and Mohammed Ali Abdulqader. Resources: Srishti Laller, Suprada Vinayak, Harshini Adimoulame, Gurinder Singh, and Urvish Patel. Validation: Neev Mehta, Suprada Vinayak, Hyundam Gu, and Srishti Laller. Data curation: Aditya Mansabdar, Bhavani Gangineni, Suprada Vinayak, Hardik Jain, Amitjeet, Singh Rekhraj, and Urvish Patel. Writing - original draft preparation: Rutvi Amin, Aditya Mansabdar, Hyundam Gu, and Harini Patel. Writing - review, critical feedback, and editing: Rutvi Amin, Aditya Mansabdar, Srishti Laller, Harshini Adimoulame, Jose Moonjely Davis, and Harmeet Gill. Visualization: Jose Moonjely Davis. Project administration: Jose Moonjely Davis and Harmeet Gill. Supervision: Harmeet Gill.
Data Availability
The data are collected from the studies published online, publicly available, and specific details related to the data and/or analysis will be available upon request.
Abbreviations
IBD: inflammatory bowel disease; GALT: gut-associated lymphoid tissue; MOOSE: Meta-analysis of Observational Studies in Epidemiology; OR: odds ratio; CI: confidence interval; CD: Crohn’s disease; UC: ulcerative colitis; MALT: mucosa-associated lymphoid tissue; MALTectomy: mucosa-associated lymphoid tissue removal; ILF: isolated lymphoid follicles; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta Analysis; RA: Rutvi Amin; AM: Aditya Mansabdar; HG: Hyundam Gu; UP: Urvish Patel; BG: Bhavani Gangineni; HP: Harini Patel; NM: Neev Mehta; NP: Neil Patel; RR: relative risk; AHR: adjusted hazard ratio; HR: hazard ratio; H/o: history of; NOS: Newcastle-Ottawa Scale
| References | ▴Top |
- Carriere J, Darfeuille-Michaud A, Nguyen HT. Infectious etiopathogenesis of Crohn's disease. World J Gastroenterol. 2014;20(34):12102-12117.
doi pubmed pmc - McDowell C, Farooq U, Haseeb M. Inflammatory bowel disease. In: StatPearls. Treasure Island (FL) with ineligible companies. 2024.
pubmed - Muzes G, Bohusne Barta B, Sipos F. Colitis and colorectal carcinogenesis: the focus on isolated lymphoid follicles. Biomedicines. 2022;10(2):226.
doi pubmed pmc - Heel KA, McCauley RD, Papadimitriou JM, Hall JC. Review: Peyer's patches. J Gastroenterol Hepatol. 1997;12(2):122-136.
doi pubmed - Brandtzaeg P, Kiyono H, Pabst R, Russell MW. Terminology: nomenclature of mucosa-associated lymphoid tissue. Mucosal Immunol. 2008;1(1):31-37.
doi pubmed - Donaldson DS, Else KJ, Mabbott NA. The gut-associated lymphoid tissues in the small intestine, not the large intestine, play a major role in oral prion disease pathogenesis. J Virol. 2015;89(18):9532-9547.
doi pubmed pmc - Andoh A, Sakata S, Koizumi Y, Mitsuyama K, Fujiyama Y, Benno Y. Terminal restriction fragment length polymorphism analysis of the diversity of fecal microbiota in patients with ulcerative colitis. Inflamm Bowel Dis. 2007;13(8):955-962.
doi pubmed - Fujimoto T, Imaeda H, Takahashi K, Kasumi E, Bamba S, Fujiyama Y, Andoh A. Decreased abundance of Faecalibacterium prausnitzii in the gut microbiota of Crohn's disease. J Gastroenterol Hepatol. 2013;28(4):613-619.
doi pubmed - Nishino K, Nishida A, Inoue R, Kawada Y, Ohno M, Sakai S, Inatomi O, et al. Analysis of endoscopic brush samples identified mucosa-associated dysbiosis in inflammatory bowel disease. J Gastroenterol. 2018;53(1):95-106.
doi pubmed - Sartor RB, Wu GD. Roles for intestinal bacteria, viruses, and fungi in pathogenesis of inflammatory bowel diseases and therapeutic approaches. Gastroenterology. 2017;152(2):327-339.e324.
doi pubmed pmc - Takahashi K, Nishida A, Fujimoto T, Fujii M, Shioya M, Imaeda H, Inatomi O, et al. Reduced abundance of butyrate-producing bacteria species in the fecal microbial community in Crohn's disease. Digestion. 2016;93(1):59-65.
doi pubmed - Bhattacharyya N, Lin HW. Changes and consistencies in the epidemiology of pediatric adenotonsillar surgery, 1996-2006. Otolaryngol Head Neck Surg. 2010;143(5):680-684.
doi pubmed - Koutroubakis IE, Vlachonikolis IG, Kapsoritakis A, Spanoudakis S, Roussomoustakaki M, Mouzas IA, Kouroumalis EA, et al. Appendectomy, tonsillectomy, and risk of inflammatory bowel disease: case-controlled study in Crete. Dis Colon Rectum. 1999;42(2):225-230.
doi pubmed - Kiasat A, Ekstrom LD, Marsk R, Lof-Granstrom A, Gustafsson UO. Childhood appendicitis and future risk of inflammatory bowel disease - A nationwide cohort study in Sweden 1973-2017. Colorectal Dis. 2022;24(8):975-983.
doi pubmed pmc - Bager P, Gortz S, Feenstra B, Nyboe Andersen N, Jess T, Frisch M, Melbye M. Increased risk of inflammatory bowel disease in families with tonsillectomy: a Danish national cohort study. Epidemiology. 2019;30(2):256-262.
doi pubmed - Kurina LM, Goldacre MJ, Yeates D, Seagroatt V. Appendicectomy, tonsillectomy, and inflammatory bowel disease: a case-control record linkage study. J Epidemiol Community Health. 2002;56(7):551-554.
doi pubmed pmc - Chen D, Ma J, Ben Q, Lu L, Wan X. Prior appendectomy and the onset and course of Crohn's disease in Chinese patients. Gastroenterol Res Pract. 2019;2019:8463926.
doi pubmed pmc - Chung WS, Chung S, Hsu CY, Lin CL. Risk of inflammatory bowel disease following appendectomy in adulthood. Front Med (Lausanne). 2021;8:661752.
doi pubmed pmc - Fantodji C, Jantchou P, Parent ME, Rousseau MC. Appendectomy and risk for inflammatory bowel disease: effect of age and time post appendectomy - a cohort study. BMJ Open Gastroenterol. 2022;9(1):e000925.
doi pubmed pmc - Sun W, Han X, Wu S, Yang C. Tonsillectomy and the risk of inflammatory bowel disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2016;31(6):1085-1094.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


