| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 16, Number 1, February 2023, pages 17-24
A Comparative Analysis of Bleeding Peptic Ulcers in Hospitalizations With and Without End-Stage Renal Disease
Dushyant Singh Dahiyaa, l, m , Sohaib Mandoorahb, l, Manesh Kumar Gangwanic, Hassam Alid, Nooraldin Merzac, Muhammad Azize, Amandeep Singhf, Abhilash Perisettig, Rajat Gargf, Chin-I Chengh, Priyata Duttai, Sumant Inamdarj, Madhusudhan R. Sanakaf, Mohammad Al-Haddadk
aDepartment of Internal Medicine, Central Michigan University College of Medicine, Saginaw, MI, USA
bDivision of Pulmonary and Critical Care Medicine, Central Michigan University College of Medicine, Saginaw, MI, USA
cDepartment of Internal Medicine, The University of Toledo Medical Center, Toledo, OH, USA
dDepartment of Internal Medicine, East Carolina University, Greenville, NC, USA
eDepartment of Gastroenterology and Hepatology, The University of Toledo Medical Center, Toledo, OH, USA
fDepartment of Gastroenterology, Hepatology and Nutrition, Cleveland Clinic Foundation, Cleveland, OH, USA
gDivision of Gastroenterology and Hepatology, Kansas City Veterans Affairs Medical Center, Kansas City, MO, USA
hDepartment of Statistics, Actuarial and Data Science, Central Michigan University, Mt Pleasant, MI, USA
iDepartment of Internal Medicine, Trinity Health, Ann Arbor, MI, USA
jDepartment of Gastroenterology and Hepatology, University of Arkansas for Medical Sciences, Little Rock, AR, USA
kDivision of Gastroenterology and Hepatology, Indiana University School of Medicine Indianapolis, IN, USA
lThese authors contributed equally to this article.
mCorresponding Author: Dushyant Singh Dahiya, Department of Internal Medicine, Central Michigan University College of Medicine, Saginaw, MI 48601, USA
Manuscript submitted February 11, 2023, accepted February 13, 2023, published online February 28, 2023
Short title: Peptic Ulcer Bleeding in ESRD
doi: https://doi.org/10.14740/gr1605
| Abstract | ▴Top |
Background: End-stage renal disease (ESRD) patients are highly susceptible to peptic ulcer bleeding (PUB). We aimed to assess the influence of ESRD status on PUB hospitalizations in the United States (USA).
Methods: We analyzed the National Inpatient Sample to identify all adult PUB hospitalizations in the USA from 2007 to 2014, which were divided into two subgroups based on the presence or absence of ESRD. Hospitalization characteristics and clinical outcomes were compared. Furthermore, predictors of inpatient mortality for PUB hospitalizations with ESRD were identified.
Results: Between 2007 and 2014, there were 351,965 PUB hospitalizations with ESRD compared to 2,037,037 non-ESRD PUB hospitalizations. PUB ESRD hospitalizations had a higher mean age (71.6 vs. 63.6 years, P < 0.001), and proportion of ethnic minorities i.e., Blacks, Hispanics, and Asians compared to the non-ESRD cohort. We also noted higher all-cause inpatient mortality (5.4% vs. 2.6%, P < 0.001), rates of esophagogastroduodenoscopy (EGD) (20.7% vs. 19.1%, P < 0.001), and mean length of stay (LOS) (8.2 vs. 6 days, P < 0.001) for PUB ESRD hospitalizations compared to the non-ESRD cohort. After multivariate logistic regression analysis, Whites with ESRD had higher odds of mortality from PUB compared to Blacks. Furthermore, the odds of inpatient mortality from PUB decreased by 0.6% for every 1-year increase in age for hospitalizations with ESRD. Compared to the 2011 - 2014 study period, the 2007 - 2010 period had 43.7% higher odds (odds ratio (OR): 0.696, 95% confidence interval (CI): 0.645 - 0.751) of inpatient mortality for PUB hospitalizations with ESRD.
Conclusions: PUB hospitalizations with ESRD had higher inpatient mortality, EGD utilization, and mean LOS compared to non-ESRD PUB hospitalizations.
Keywords: Peptic ulcer bleeding; Upper gastrointestinal bleeding; End-stage renal disease; Racial disparities; Mortality
| Introduction | ▴Top |
Peptic ulcer disease (PUD) has been recognized as a significant contributor to mortality in the United States (USA) [1]. However, in recent years, the incidence and prevalence of PUD have decreased due to improved hygiene and sanitary conditions. PUD is characterized by a defect in the duodenal or gastric mucosa extending beyond the muscularis mucosa into deeper layers of the gastrointestinal (GI) tract. It is also associated with several complications, the most cited of which is peptic ulcer bleeding (PUB), seen in up to 15-20% of the patients [2]. It has been identified as the most common cause of non-variceal upper GI bleeding (UGIB) worldwide [3-5]. Similarly, in the USA, there are about 350,000 hospitalizations annually for UGIB, of which PUB has consistently been a leading cause. Despite significant advancements in medical and endoscopic therapy, severe PUB continues to be life-threatening condition associated with considerable mortality, decreased overall quality of life, and higher healthcare costs [3-5].
Studies report that patients with end-stage renal disease (ESRD), through a cluster of complex pathophysiological mechanisms, are at a higher risk of bleeding peptic ulcers than the general population [6, 7]. A higher rate of hemodialysis utilization, which is independently associated with a higher occurrence of PUB, has also been reported in the US population and may amplify the rate of PUB [7]. However, there continues to be a significant knowledge gap on the exact influence of ESRD status on PUB. Hence, this study was designed to assess and compare hospitalization characteristics, clinical outcomes, and the healthcare burden of PUB in patients with and without ESRD. Furthermore, we also identified the rates of utilization of esophagogastroduodenoscopy (EGD) in these hospitalizations and the predictors of all-cause inpatient mortality for PUB hospitalizations with ESRD.
| Materials and Methods | ▴Top |
Design and data source
This retrospective study utilized the National Inpatient Sample (NIS) database to derive the study population. The NIS is one of the largest, publicly available, multi-ethnic databases in the USA. It is maintained by Agency for Healthcare Research and Quality (AHRQ) as a part of the Healthcare Cost and Utilization Project (HCUP). It is derived from billing data submitted by hospitals across the USA to state-wide data organizations. It covers > 95% of the US population and approximates a 20% stratified sample of discharges from US community hospitals [8]. The dataset is weighted to obtain national estimates [9]. During the 2007 - 2014 study period, the NIS database was coded using the International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System (ICD-9-CM/PCS). The database can be accessed from HCUP [10].
Study population and outcome measures
We utilized the NIS to identify all adult (≥ 18 years) hospitalizations with a primary diagnosis of PUB in the USA from 2007 to 2014. The study population was divided into two distinct groups based on the presence or absence of ESRD. A comparative analysis was performed for hospitalization characteristics, clinical outcomes, rates of utilization of EGD, and the burden of the disease on the US healthcare system. Moreover, predictors of all-cause inpatient mortality were also identified for PUB hospitalizations with ESRD.
Statistical analysis
Statistical analysis was conducted using SAS 9.4 (SAS Institute Inc, Cary, NC) to account for the stratified survey design weights. The weights were considered in the statistical estimating process by incorporating the variables for the strata, cluster, and weight. Descriptive statistics included meaning for continuous variables and count (percentage) for categorical variables. The Cochran-Armitage trend test was implemented to test the trend for proportions of binary variables in years. The Rao-Scott design-adjusted Chi-square test, which took the stratified survey design into account, examined the association between two categorical variables. A multivariable logistic regression model was adopted to identify associations between in-hospital mortality and demographic variables. All analytical results were considered significant when P values were ≤ 0.05.
Ethical considerations
As the NIS database lacks specific patient and hospital identifiers, our study was exempt from Institutional Review Board (IRB) approval per guidelines put forth by our institutional IRB for analysis of inpatient databases. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
Comparative analysis of hospitalization characteristics
Between 2007 and 2014, there were 351,965 PUB hospitalizations with ESRD compared to 2,037,037 non-ESRD PUB hospitalizations in the USA (Table 1). PUB hospitalizations with ESRD had a higher mean age (71.6 vs. 63.6 years, P < 0.001) and proportion of males (55.5% vs. 44.2%, P < 0.001) compared to non-ESRD PUB hospitalizations. Racial differences were also evident in our study. PUB hospitalizations with ESRD had a higher proportion of ethnic minorities, i.e., Blacks (20.2% vs. 12.4%, P < 0.001), Hispanics (9.2% vs. 8.5%, P < 0.001), and Asians (4.5% vs. 3.3%, P < 0.001) compared to the non-ESRD PUB cohort. However, non-ESRD PUB hospitalizations had a higher proportion of Whites (72.2% vs. 63.2%, P < 0.001) than the PUB ESRD subgroup. Interestingly, we noted a lower proportion of patients with Helicobacter pylori (H. pylori) (3.8% vs. 5.7%, P < 0.001) in the PUB ESRD cohort compared to non-ESRD PUB hospitalizations.
 Click to view | Table 1. Hospitalization Characteristics and Clinical Outcomes for Peptic Ulcer Bleeding (PUB) Hospitalizations With and Without End-Stage Renal Disease (ESRD) in the United States From 2007 to 2014 |
Comparative analysis of clinical outcomes and healthcare burden
PUB hospitalizations with ESRD had a longer mean length of stay (LOS) (8.2 vs. 6 days, P < 0.001) and higher rates of all-cause inpatient mortality (5.4% vs. 2.6%, P < 0.001) compared to the non-ESRD-PUB cohort. Moreover, the rates of utilization of EGD were higher for PUB hospitalizations with ESRD (20.9% vs. 19.1%, P < 0.001) compared to the non-ESRD PUB cohort. Compared to non-ESRD PUB hospitalizations, we noted a higher proportion of PUB hospitalizations with ESRD at large (62.7% vs. 60.7%, P < 0.001), urban teaching (47.9% vs. 45.6%, P < 0.001) hospitals. Most PUB hospitalizations with ESRD were reported in the South (37.3%), followed by the Midwest (24.7%), West (21%), and Northeast (17.1%) hospital regions.
Predictors of all-cause inpatient mortality
A multivariate regression analysis was performed to investigate the predictors of all-cause inpatient mortality for PUB hospitalizations with ESRD. We noted a decrease in the odds of inpatient mortality by 0.6% (odds ratio (OR): 0.994, 95% confidence interval (CI): 0.991 - 0.997) for every 1-year increase in age; however, no effect of gender was noted. White PUB hospitalizations with ESRD had 32.1% higher odds (OR: 0.757, 95% CI: 0.683 - 0.840) of inpatient mortality compared to Blacks (Table 2). Furthermore, the study period was divided into two distinct 4-year periods to compare the differences in all-cause inpatient mortality with time. After multivariate regression analysis, we noted 43.7% higher odds (OR: 0.696, 95% CI: 0.645 - 0.751) of inpatient mortality for PUB hospitalizations with ESRD for the 2007 - 2010 study period compared to the 2011 - 2014 period (Table 2).
 Click to view | Table 2. Independent Predictors of All-Cause Inpatient Mortality for Peptic Ulcer Bleeding (PUB) Hospitalizations With End-Stage Renal Disease (ESRD) in the United States From 2007 to 2014 |
| Discussion | ▴Top |
We compared 351,965 PUB hospitalizations with ESRD to 2,037,037 non-ESRD PUB hospitalizations between 2007 and 2014 in the USA. Ethnic minorities, i.e., Blacks, Hispanics, and Asians were disproportionately affected as we noted higher rates of PUB hospitalizations with ESRD compared to the non-ESRD PUB cohort. We also noted higher healthcare utilization rates for PUB hospitalizations with ESRD as these patients had a longer LOS and EGD utilization compared to the non-ESRD PUB cohort. Furthermore, the all-cause inpatient mortality was more than double (5.4% vs. 2.6%, P < 0.001) for PUB hospitalizations with ESRD compared to the non-ESRD PUB cohort. After multivariate logistic regression analysis, White race, lower age, and 2007 - 2010 study period were associated with higher inpatient mortality rates. These findings are of utmost importance as they provide gastroenterologists with real-world data on PUB hospitalizations with ESRD at the highest risk of adverse clinical outcomes and those who may benefit the most from prompt and aggressive therapeutic measures.
PUD affects 4 million people worldwide annually with an incidence rate of 1.5-3% and a complication rate of 10-20% [11-15]. PUB, seen in about 15-20% of the patients with PUD, has been cited as the most common complication [2]. Compared to the general population, patients with ESRD have a higher incidence of PUD complicated by UGIB, leading to higher mortality, healthcare costs, and reduced quality of life [4, 5, 16, 17, 19]. Although H. pylori infection continues to one of the most common causes of PUD, the epidemiology of PUD and its complications have evolved over the years [19, 20]. A longer life expectancy, widespread use of non-steroidal anti-inflammatory drugs (NSAIDs), higher comorbidities, and ESRD requiring dialysis are responsible for higher rates of PUB [19, 21-25]. In our study, there were 351,965 PUB hospitalizations with ESRD with a mean age of 71.6 years and 55.5% males. However, the mean age for non-ESRD PUB hospitalizations was 63.5 years, with a slight female predominance (51% vs. 49%, P < 0.001). These findings may be related to the older age of patients with ESRD, who are at higher-than-average risk of PUB, and the fact that there is a male predominance in the prevalence of ESRD and the utilization of hemodialysis [26].
Racial differences were also prevalent in our study. PUB hospitalizations with ESRD had a higher proportion of ethnic minorities such as Blacks, Hispanics, and Asians; however, non-ESRD PUB hospitalizations had a higher proportion of Whites (Table 1). These findings align with current literature citing PUB as the most common complication of PUD in Whites, whereas Blacks have lower rates of PUB but higher rates of complications of PUD [27, 28]. Interestingly, H. pylori infection was more frequent in non-ESRD PUB hospitalizations compared to PUB hospitalizations with ESRD. The exact reason for this finding is unknown and needs further investigation with larger prospective studies.
Despite significant advancements in the management strategies for PUB, the mortality rate remains high, ranging from 5% to 10% worldwide [29]. Numerous studies have focused on the short-term mortality after PUB; however, only some estimate the long-term complications. In literature, the overall 30-day mortality of PUB has been reported as 10.8% with a higher prevalence of mortality in patients ≥ 80 years, followed by patients aged 65 - 79 years and then individuals < 65 years of age [30]. In our study, we report a higher mortality rate for PUB hospitalizations with ESRD (5.4% vs. 2.6%, P < 0.001) compared to patients admitted for PUB do not have ESRD. Furthermore, for PUB hospitalizations with ESRD, an analysis of individual years from 2007 to 2014 revealed a downtrend in the PUB mortality rate from 6.6% in 2007 to 4.8% in 2014 (Fig. 1). However, the mortality rates for PUB in patients without ESRD decreases slightly from 2.7% in 2007 to 2.5% in 2014 (Fig. 2). From a procedural perspective, we noted a higher number of EGDs for PUB hospitalizations with ESRD (20.9% vs. 19.1%, P < 0.001) compared to the non-ESRD cohort. This may be secondary to a higher number of re-bleeds or a low threshold for endoscopic intervention in these typically ill ESRD patients. It is worth noting that the overall rates of EGD for both sub-groups were low. The exact reason for this finding is currently unknown and needs further investigation with large, prospective, multi-center studies to identify patient characteristics that required inpatient EGDs compared to those that did not.
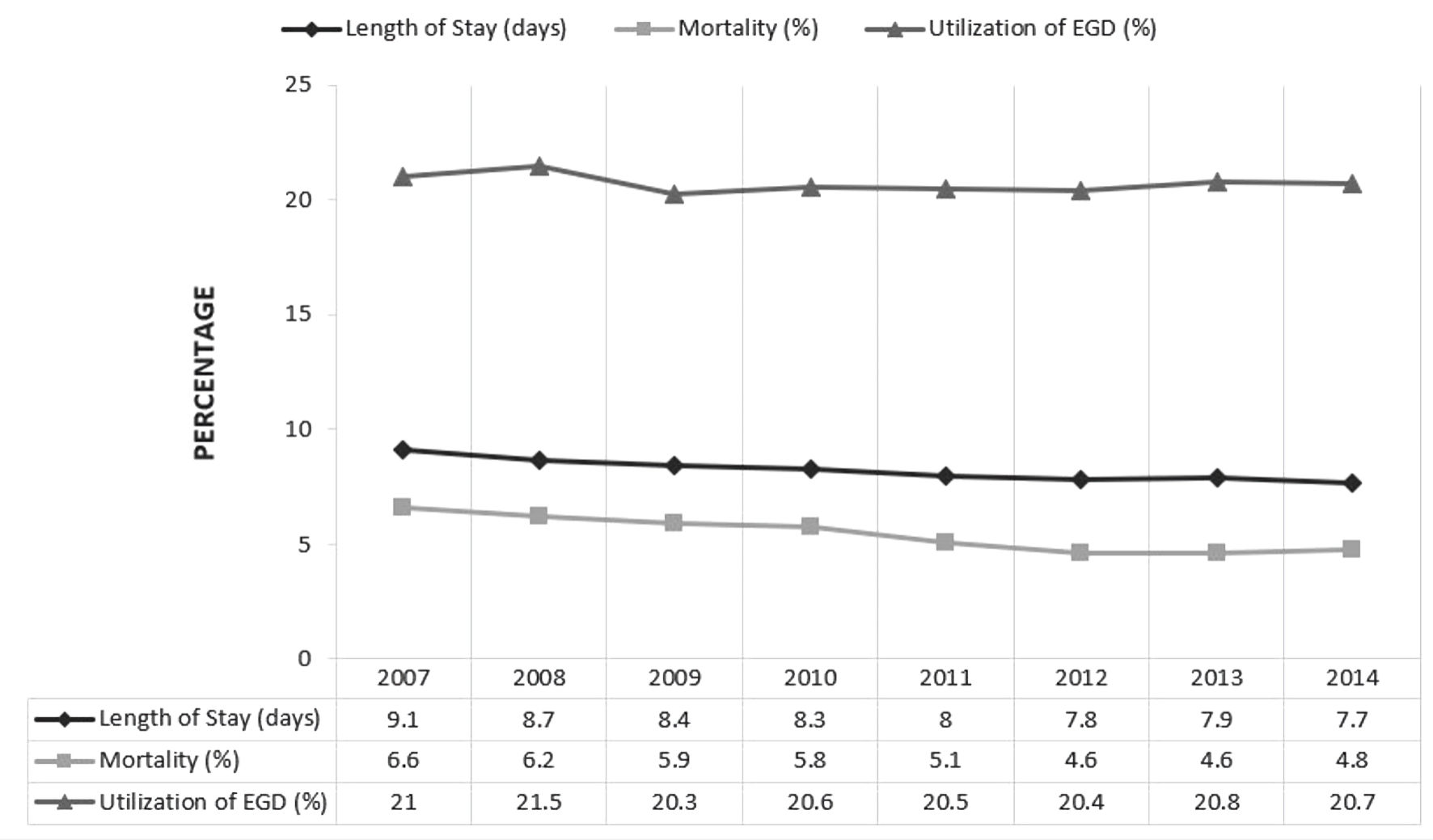 Click for large image | Figure 1. Trends of length of stay, esophagogastroduodenoscopy (EGD) utilization and all-cause inpatient mortality for peptic ulcer bleeding (PUB) hospitalizations with end-stage renal disease (ESRD) in the United States. |
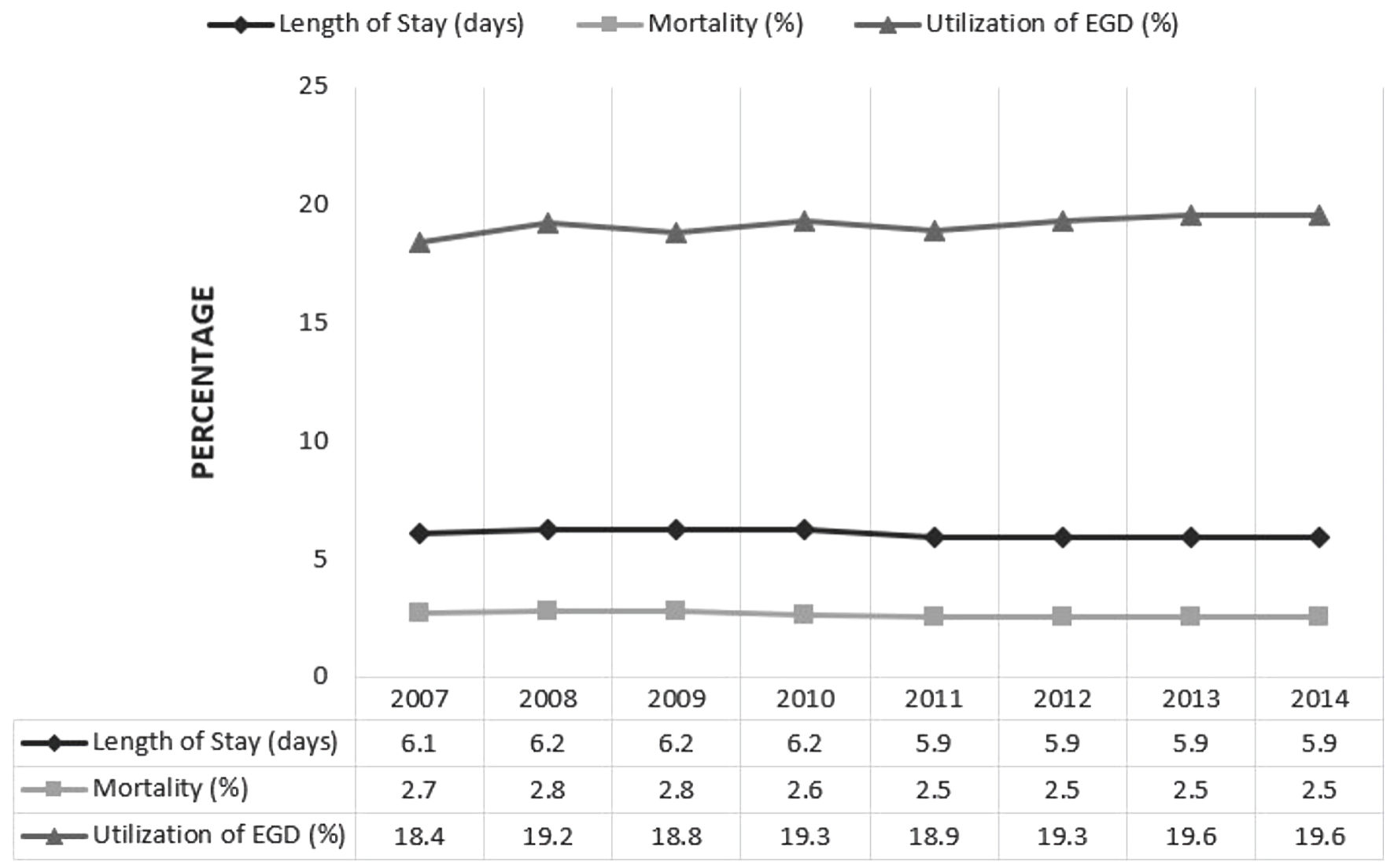 Click for large image | Figure 2. Trends of length of stay, esophagogastroduodenoscopy (EGD) utilization and all-cause inpatient mortality for peptic ulcer bleeding (PUB) hospitalizations without end-stage renal disease (ESRD) in the United States. |
A multivariate regression analysis was performed to identify independent predictors of all-cause inpatient mortality for PUB hospitalizations with ESRD (Table 2). We noted a decrease in the odds of inpatient mortality by 0.6% for every 1-year increase in age. This may, in part, be because more patients died of non-ulcer bleeding causes, which tends to increase with age, rather than PUB. Similar findings were observed in a study by Sung et al, where 79.7% of the confirmed 9,375 cases of PUB died secondary to non-ulcer bleeding causes such as multiorgan failure, pulmonary conditions, and terminal malignancy [29]. Furthermore, gender was not an independent predictor for all-cause inpatient mortality for PUB hospitalizations with ESRD. This may have been due to a downtrend in the mortality rates for both genders proportionately. Additionally, we noted that White PUB hospitalizations with ESRD had higher odds of inpatient mortality compared to Blacks. This may be because the reference population of Black patients with PUD have the lowest rates of PUB among all races, but the highest rate of bowel perforations as a complication of PUD [27]. Our analysis also revealed that the odds of inpatient mortality for the 2007 - 2010 study period was 43.7% higher (OR: 0.696, 95% CI: 0.645 - 0.751) than that for the 2011 - 2014 period. This suggests a significant improvement in the overall management of PUB in the later years, as reported in current literature [31].
PUB places a significant burden on the US healthcare system in terms of attributable costs and utilization of resources for management. The cost of management of non-variceal UGIB, of which PUB is the leading cause, has been estimated to be around $3,402 per person per hospital stay without complications and $5,632 per person per hospital stay with complications [32]. This cost is expected to be higher in patients with ESRD as they are at higher-than-average risk of additional complications, risk of rebleeding, longer hospital stays, and other acute care needs. In our study, we noted a longer mean length of hospital stay (8.2 vs. 6 days, P < 0.001) for PUB hospitalizations with ESRD compared to the non-ESRD cohort. Additionally, larger hospitals were noted to have close to two-thirds of the total PUB hospitalizations with ESRD followed by medium-sized hospitals and then smaller hospitals. Teaching hospitals located in urban areas made up 47.9% of these inpatient admissions, followed closely by urban non-teaching (42.9%) and then by rural hospitals (9.2%). This inequitable distribution may be because large hospitals located in dense urban areas are usually tertiary referral care centers, with better access to resources and multi-disciplinary expertise to manage the disease entity and its complications.
This NIS-based study has several strengths and some limitations. The biggest strength of the study is the study population, which is derived from the largest, publicly available, all-payer healthcare database designed to provide US regional and national estimates of inpatient utilization, access, charges, quality, and outcomes. Additionally, by using only ICD-9 codes (2007 - 2014 study period) for the analysis, we were able to maintain uniformity in the study population and prevent bias from unknown confounders. Furthermore, due to the unique study design, we were able to thoroughly examine multiple outcome-oriented facets and hospitalization data for this large study population. Our study also provides gastroenterologists with an in-depth perspective of the magnitude of disease and its burden on the US healthcare system. However, we acknowledge all the limitations associated with this study. The NIS lacks data on the ethology of ESRD, time to diagnosis, the severity of the condition, the hospitalization course, medications (i.e., anticoagulants, antiplatelets, NSAIDs, etc.), and pharmacological aspects of management for the disease. Due to the limitations associated with the NIS database in an effort to protect patient privacy, we are unable to see individual patient characteristics that would have led to an inpatient EGD and rates of H. pylori in both subgroups. Additionally, the data available from NIS are subject to all the biases present in retrospective studies. Lastly, the NIS is an administrative database that uses the ICD-9 coding system to gather relevant information on hospitalizations and outcomes; hence, it is prone to coding errors. However, despite these limitations, the large sample size, analysis techniques to limit bias, and the answers to proposed scientific questions provide a better understanding of the topic in question. Through this study, we strive to stimulate discussion and encourage future large, multi-center prospective clinical studies on PUB in patients with ESRD.
Conclusions
In conclusion, our study explored, in-depth, the relationship between PUB and ESRD. PUD hospitalizations with ESRD had a higher proportion of ethnic minorities (Blacks, Hispanics, and Asians) compared to the non-ESRD cohort. We also report higher mortality rates, longer LOS, and higher utilization of EGD for PUB hospitalizations with ESRD compared to the non-ESRD cohort. However, for the study period, the all-cause inpatient mortality for PUD hospitalizations with ESRD was on a steady decline, reflecting a significant improvement in management strategies.
Acknowledgments
None to declare.
Financial Disclosure
No funding sources to declare.
Conflict of Interest
All other authors report no conflict of interest.
Informed Consent
As the NIS database lacks patient and hospital identifiers, informed consent was not required for this study.
Author Contributions
Conceptualization: Dushyant Singh Dahiya, Madhusudhan R. Sanaka, and Mohammad Al-Haddad. Data curation: Dushyant Singh Dahiya and Chin-I Cheng. Formal analysis: Chin-I Cheng. Project administration: Dushyant Singh Dahiya and Mohammad Al-Haddad. Resources: Dushyant Singh Dahiya and Chin-I Cheng. Software: Chin-I Cheng. Supervision: Dushyant Singh Dahiya, Madhusudhan R. Sanaka, and Mohammad Al-Haddad. Visualization: Dushyant Singh Dahiya and Mohammad Al-Haddad. Investigation, methodology, validation, writing-original draft, writing-review and editing: all authors.
Data Availability
The National Inpatient Sample (NIS) is a large, publicly available, all-payer inpatient care database in the United States containing data on millions of hospital stays per year. The large sample size derived from the NIS database provides sufficient data for the analysis of uncommon disorders and procedures. The NIS is publicly available at: https://www.hcup-us.ahrq.gov/.
Abbreviations
AHRQ: Agency for Healthcare Research and Quality; CCI: Charlson Comorbidity Index; CI: confidence interval; EGD: esophagogastroduodenoscopy; ESRD: end-stage renal disease; GI: gastrointestinal; ICD-9-CM/PCS: International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System; IRB: Institutional Review Board; LOS: length of stay; NIS: National Inpatient Sample; OR: odds ratio; PUD: peptic ulcer disease; PUB: peptic ulcer bleeding; UGIB: upper gastrointestinal bleeding
| References | ▴Top |
- Duggan JM, Duggan AE. The possible causes of the pandemic of peptic ulcer in the late 19th and early 20th century. Med J Aust. 2006;185(11-12):667-669.
doi pubmed - Narayanan M, Reddy KM, Marsicano E. Peptic ulcer disease and helicobacter pylori infection. Mo Med. 2018;115(3):219-224.
- Kamboj AK, Hoversten P, Leggett CL. Upper gastrointestinal bleeding: etiologies and management. Mayo Clin Proc. 2019;94(4):697-703.
doi pubmed - Quan S, Frolkis A, Milne K, Molodecky N, Yang H, Dixon E, Ball CG, et al. Upper-gastrointestinal bleeding secondary to peptic ulcer disease: incidence and outcomes. World J Gastroenterol. 2014;20(46):17568-17577.
doi pubmed - Barkun A, Leontiadis G. Systematic review of the symptom burden, quality of life impairment and costs associated with peptic ulcer disease. Am J Med. 2010;123(4):358-366.e352.
doi pubmed - Lin XH, Lin CC, Wang YJ, Luo JC, Young SH, Chen PH, Hou MC, et al. Risk factors of the peptic ulcer bleeding in aging uremia patients under regular hemodialysis. J Chin Med Assoc. 2018;81(12):1027-1032.
doi pubmed - Laeeq SM, Tasneem AA, Hanif FM, Luck NH, Mandhwani R, Wadhva R. Upper gastrointestinal bleeding in patients with end stage renal disease: causes, characteristics and factors associated with need for endoscopic therapeutic intervention. J Transl Int Med. 2017;5(2):106-111.
doi pubmed - Healthcare Cost and Utilization Project. Introduction to the HCUP National Inpatient Sample (NIS). The National (nationwide) Inpatient Sample database documentation. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2016.jsp and https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2017.jsp. Accessed December 12, 2022.
- Houchens R, Ross D, Elixhauser A, et al. Nationwide Inpatient Sample (NIS) Redesign Final Report. 2014. HCUP Methods Series Report # 2014-04 ONLINE. April 4, 2014. U.S. Agency for Healthcare Research and Quality. Available: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed December 12, 2022.
- https://www.hcup-us.ahrq.gov
- Chung KT, Shelat VG. Perforated peptic ulcer - an update. World J Gastrointest Surg. 2017;9(1):1-12.
doi pubmed - Zelickson MS, Bronder CM, Johnson BL, Camunas JA, Smith DE, Rawlinson D, Von S, et al. Helicobacter pylori is not the predominant etiology for peptic ulcers requiring operation. Am Surg. 2011;77(8):1054-1060.
doi pubmed - Zittel TT, Jehle EC, Becker HD. Surgical management of peptic ulcer disease today—indication, technique and outcome. Langenbecks Arch Surg. 2000;385(2):84-96.
doi pubmed - Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010;27(3):161-169.
doi pubmed - Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC. Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion. 2011;84(2):102-113.
doi pubmed - Abbasi MA, Chertow GM, Hall YN. End-stage renal disease. BMJ Clin Evid. 2010;2010:2002.
- Kim M, Kim CS, Bae EH, Ma SK, Kim SW. Risk factors for peptic ulcer disease in patients with end-stage renal disease receiving dialysis. Kidney Res Clin Pract. 2019;38(1):81-89.
doi pubmed - Tseng GY, Lin HJ, Fang CT, Yang HB, Tseng GC, Wang PC, Hung TL, et al. Recurrence of peptic ulcer in uraemic and non-uraemic patients after Helicobacter pylori eradication: a 2-year study. Aliment Pharmacol Ther. 2007;26(6):925-933.
doi pubmed - Kyaw MH, Lau JYW. High rate of mortality more than 30 days after upper gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2017;15(12):1858-1859.
doi pubmed - Sung JJ, Kuipers EJ, El-Serag HB. Systematic review: the global incidence and prevalence of peptic ulcer disease. Aliment Pharmacol Ther. 2009;29(9):938-946.
doi pubmed - Musa SA, Brecker SJ, Rahman TM, Kang JY. Upper gastrointestinal haemorrhage in the acute cardiac care setting: antiplatelets and endoscopy. Scott Med J. 2012;57(2):88-91.
doi pubmed - Saran R, Robinson B, Abbott KC, Bragg-Gresham J, Chen X, Gipson D, Gu H, et al. US renal data system 2019 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2020;75(Suppl 1):1 A6-A7.
doi pubmed - McCullough KP, Morgenstern H, Saran R, Herman WH, Robinson BM. Projecting ESRD incidence and prevalence in the United States through 2030. J Am Soc Nephrol. 2019;30(1):127-135.
doi pubmed - Kaplan AA. Peritoneal dialysis or hemodialysis: present and future trends in the United States. Contrib Nephrol. 2017;189:61-64.
doi pubmed - Cheung J, Yu A, LaBossiere J, Zhu Q, Fedorak RN. Peptic ulcer bleeding outcomes adversely affected by end-stage renal disease. Gastrointest Endosc. 2010;71(1):44-49.
doi pubmed - Hecking M, Bieber BA, Ethier J, Kautzky-Willer A, Sunder-Plassmann G, Saemann MD, Ramirez SP, et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the Dialysis Outcomes and Practice Patterns Study (DOPPS). PLoS Med. 2014;11(10):e1001750.
doi pubmed - Havens JM, Castillo-Angeles M, Nitzschke SL, Salim A. Disparities in peptic ulcer disease: A nationwide study. Am J Surg. 2018;216(6):1127-1128.
doi pubmed - Wollenman CS, Chason R, Reisch JS, Rockey DC. Impact of ethnicity in upper gastrointestinal hemorrhage. J Clin Gastroenterol. 2014;48(4):343-350.
doi pubmed - Sung JJ, Tsoi KK, Ma TK, Yung MY, Lau JY, Chiu PW. Causes of mortality in patients with peptic ulcer bleeding: a prospective cohort study of 10,428 cases. Am J Gastroenterol. 2010;105(1):84-89.
doi pubmed - Christensen S, Riis A, Norgaard M, Sorensen HT, Thomsen RW. Short-term mortality after perforated or bleeding peptic ulcer among elderly patients: a population-based cohort study. BMC Geriatr. 2007;7:8.
doi pubmed - Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair P, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152(2):101-113.
doi pubmed - Adam V, Barkun AN. Estimates of costs of hospital stay for variceal and nonvariceal upper gastrointestinal bleeding in the United States. Value Health. 2008;11(1):1-3.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


