| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website http://www.gastrores.org |
Case Report
Volume 12, Number 1, February 2019, pages 37-39
Peri-Ampullary Metastasis From Endometrial Adenocarcinoma: A Rare Etiology of Obstructive Jaundice
Eimad Ahmmada, d, Ahmad S. Abdulkarimb, Ahmed Dirweeshc
aDivision of Internal Medicine, Mayo Clinic, Rochester, MN, USA
bHealthPartners Specialty Center, Digestive Care, Saint Paul, MN, USA
cDivision of Gastroenterology, University of Minnesota, Minneapolis, MN, USA
dCorresponding Author: Eimad Ahmmad, 200 1st St SW, Rochester, MN 55905, USA
Manuscript submitted December 12, 2018, accepted January 10, 2019
Short title: Uterine Cancer and Obstructive Jaundice
doi: https://doi.org/10.14740/gr1129
| Abstract | ▴Top |
Endometrial cancer is the commonest gynecologic malignancy, of which adenocarcinoma is the most common histologic type. While most women who relapse present with local symptoms within 3 years of the initial diagnosis, metastatic disease usually involves the abdominal cavity and liver. Herein we present a rare case of a patient with a remote history of endometrial adenocarcinoma status-post curative surgical resection and adjuvant therapy who presented with obstructive jaundice proved to be secondary to peri-ampullary metastasis of uterine adenocarcinoma.
Keywords: Endometrial; Peri-ampullary; Jaundice
| Introduction | ▴Top |
Obstructive jaundice is a known common clinical problem with detrimental consequences including liver, renal, and cardiovascular dysfunction, bleeding disorders, nutritional and immune derangement with susceptibility to infections and increased morbidity and mortality. The most common cause is biliary stones. Other causes include trauma, infections, inflammation, biliary stricture, enlarged lymph nodes and tumors. Pancreatic cancer is the most common neoplastic cause of obstructive jaundice; however ampullary or peri-ampullary metastases are extremely rare.
Uterine endometrial adenocarcinoma has a favorable prognosis since the majority of patients present with early-stage disease. Metastasis occurs in late-stage disease and it includes local metastasis (pelvic or para-aortic lymph nodes, vagina, or adnexa) and/or distant metastasis (inguinal lymph nodes, intraperitoneal cavity, lung, liver or bone). Metastasis to the pancreas or peri-ampullary region resulting in obstructive jaundice or pancreatitis is extremely rare and only few cases were reported [1-4]
| Case Report | ▴Top |
A 58-year-old morbidly obese female with a history of endometrial adenocarcinoma status post total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAHBSO) followed by chemoradiotherapy 5 years ago, who was in her usual state of health until 1 month prior to this admission when she noticed intermittent melena and most recently she had multiple bouts of diarrhea with drops of frank blood in the toilet bowl. She also reported increasing shortness of breath and yellowish discoloration of her eyes and skin. She denied abdominal pain, nausea, emesis, fever, chills, use of non-steroidal anti-inflammatory drugs, anticoagulants, alcohol or smoking use. She had an uneventful cholecystectomy for gallstone disease 2 years ago.
Her examination was significant for BMI of 46, pallor, icterus and mild epigastric tenderness. The rest of the systemic and abdominal examination was grossly normal. Laboratory workup was significant for hemoglobin of 8.0 g/dL, aspartate aminotransferase (AST) 171 U/L, alanine aminotransferase (ALT) 199 U/L, alkaline phosphatase (ALP) 1,059 U/L, total bilirubin 15.3 mg/dL, direct bilirubin 11.9 mg/dL, international normalized ratio (INR) 1.7. An upper endoscopy performed revealed a mass in the periampullary region (Fig. 1). Multiple duodenal biopsies were taken. Results were positive for a well differentiated adenocarcinoma with expression of PAX-8 and strong estrogen receptor staining consistent with metastatic endometrial cancer.
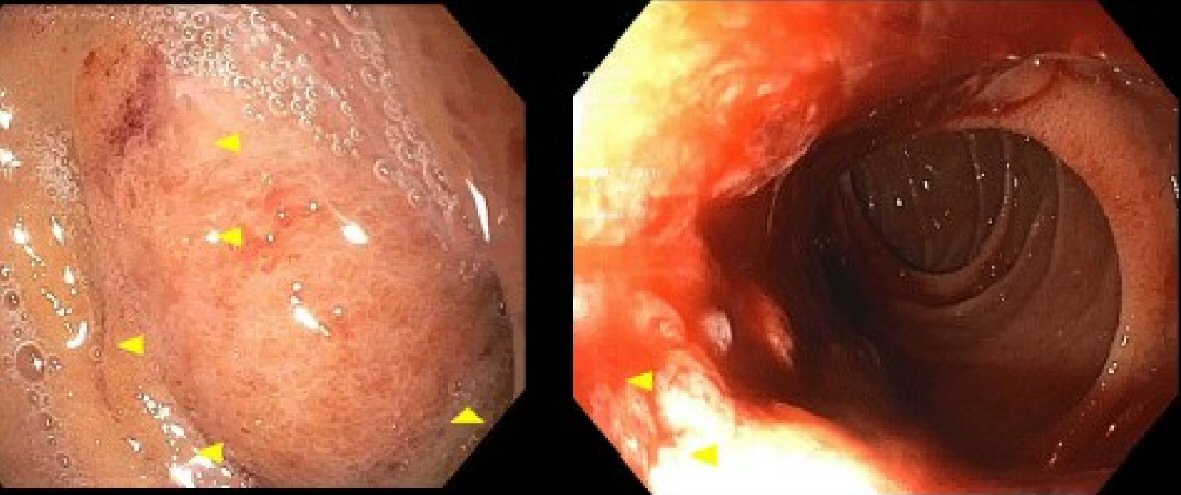 Click for large image | Figure 1. Endoscopic view of the duodenal mass before (left), and after biopsy (right). |
A computed tomography (CT) scan of the abdomen and pelvis was remarkable for mild diffuse biliary dilation. She underwent an endoscopic retrograde cholangiopancreatography (ERCP) with failed biliary access due to inadequate positioning and poor fluoroscopy penetration to facilitate the procedure. Biliary drainge was successfully achieved via percutaneous transhepatic cholangiogram and external biliary drain placement (Fig. 2).
 Click for large image | Figure 2. Percutaneous transhepatic cholangiogram and external biliary drain placement. |
| Discussion | ▴Top |
Extra-hepatic biliary obstruction can result from both benign and malignant lesions. Tumors resulting in biliary obstruction and jaundice usually arise from the pancreas, small intestine (periampullary tumors) or biliary ducts [5, 6].
The majority of tumors involving the pancreas are primary in origin, or have biliary or periampullary origins. Metastatic pancreatic tumors resulting in obstructive jaundice are rare, accounting for 2-5% of all pancreatic cancers [1, 2]. Primary tumors that commonly metastasize to the pancreas includes renal (the most common solid tumor that metastasizes to the pancreas), lung, colon and breast tumors [7]. Metastasis to the pancreas from uterine cancer is an extremely rare cause of obstructive jaundice, and only very few cases were reported in the literature [1-4]. It has been reported that the median interval between resection of the primary tumor and occurrence of the metastasis is usually around 9 years [8].
Diagnostic imaging for malignant distal biliary obstruction includes abdominal ultrasound, CT scan, magnetic resonance cholangiopancreatography (MRCP), ERCP, and endoscopic ultrasound [6, 9].
In our case, the abdominal ultrasound performed at admission was inconclusive. The abdominal CT performed was essential for further evaluation of the pancreatico-biliary system. Although surgical resection of peri-ampullary metastasis has been reported, it is not always feasible either because of local advancement of the tumor or the presence of other sites of distant metastasis. Palliative management usually focuses on biliary drainage and management of any associated complications such as bleeding and duodenal obstruction [9].
First-line therapy for patients who develop metastatic disease is typically a platinum-based chemotherapy regimen [10]. Our patient underwent a radiologically guided biliary drainage with improvement of cholestasis, thus creating a better overall clinical status for initiation of oncological therapy.
Financial Disclosures
None.
| References | ▴Top |
- Ogawa H, Tsujie M, Miyamoto A, Yasui M, Ikenaga M, Hirao M, Fujitani K, et al. Isolated pancreatic metastasis from uterine cervical cancer: a case report. Pancreas. 2011;40(5):797-798.
doi pubmed - Nishimura C, Naoe H, Hashigo S, Tsutsumi H, Ishii S, Konoe T, Watanabe T, et al. Pancreatic metastasis from mixed adenoneuroendocrine carcinoma of the uterine cervix: a case report. Case Rep Oncol. 2013;6(2):256-262.
doi pubmed - Manuel V, Rocha E, Fortini G, Pascoal Z, Netto R, Rengel L, Birolini C, et al. Uterine cancer presenting as obstructive jaundice. Int J Womens Health. 2016;8:261-263.
doi pubmed - Ogata S. Pancreatic metastasis of uterine cervix cancer mimicking a primary cancer. Dig Sys. 2018;2(1):1-2.
doi - Adsay NV, Andea A, Basturk O, Kilinc N, Nassar H, Cheng JD. Secondary tumors of the pancreas: an analysis of a surgical and autopsy database and review of the literature. Virchows Arch. 2004;444(6):527-535.
doi pubmed - Moon SG, Han JK, Kim TK, Kim AY, Kim TJ, Choi BI. Biliary obstruction in metastatic disease: thin-section helical CT findings. Abdom Imaging. 2003;28(1):45-52.
doi pubmed - Ballarin R, Spaggiari M, Cautero N, De Ruvo N, Montalti R, Longo C, Pecchi A, et al. Pancreatic metastases from renal cell carcinoma: the state of the art. World J Gastroenterol. 2011;17(43):4747-4756.
doi pubmed - Reddy S, Edil BH, Cameron JL, Pawlik TM, Herman JM, Gilson MM, Campbell KA, et al. Pancreatic resection of isolated metastases from nonpancreatic primary cancers. Ann Surg Oncol. 2008;15(11):3199-3206.
doi pubmed - Levey JM. Endoscopic biliary drainage for metastatic squamous cell carcinoma of the cervix. Gastrointest Endosc. 2000;51(1):97-99.
doi - Vale CL, Tierney J, Bull SJ, Symonds PR. Chemotherapy for advanced, recurrent or metastatic endometrial carcinoma. Cochrane Database Syst Rev. 2012;8:CD003915.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


