| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website http://www.gastrores.org |
Case Report
Volume 10, Number 2, April 2017, pages 126-127
Collagenous Gastritis in a Young Female With IgA Deficiency
Muhammad S. Anwara, c, Ali Aamara, Ali Marhabab, Jagmohan S. Sidhub
aYale-Waterbury Internal Medicine, Waterbury, CT, USA
bUHS Wilson Medical Center, Binghamton, NY, USA
cCorresponding Author: Muhammad S. Anwar, Yale-Waterbury Internal Medicine, 64 Robbins Street, Waterbury, CT 06708, USA
Manuscript accepted for publication January 26, 2017
Short title: Collagenous Gastritis
doi: https://doi.org/10.14740/gr748w
| Abstract | ▴Top |
Collagenous gastritis, without colonic involvement, is exceptionally rare. It is not known to be associated with IgA deficiency and scleroderma. This is the first report of this type of association. We present a 26-year-old white female with a past medical history of gastroesophageal reflux disease and scleroderma. She was evaluated for complaints of abdominal pain and diarrhea. Esophagogastroduodenoscopy showed gastritis and duodenitis. Colonoscopy was normal. The histopathological report showed collagenous gastritis and focal lymphocytic duodenitis. A definitive treatment has not been established for this condition. Reporting such cases furthers understanding of the disease and will help to establish diagnostic criteria and to develop therapeutic strategies.
Keywords: Collagenous gastritis; Duodenitis; Diarrhea
| Introduction | ▴Top |
Collagenous gastritis was first described in 1989 when it was reported in a 15-year-old female. Thus far, less than 60 cases of collagenous gastritis are reported in the literature. It is not known to be associated with IgA deficiency and scleroderma. This is the first report of this type of association. Histologically, it is characterized by thick collagen bands under the mucosal epithelium and infiltration of lamina propria with inflammatory cells, similar to collagenous colitis [1]. The etiology is still unclear. Due to association with autoimmune diseases, it is assumed that collagenous gastritis has an immune etiology. It is equally common among males and females. Most commonly, it presents with chronic watery diarrhea along with weight loss due to associated collagenous colitis [2].
| Case Report | ▴Top |
A 26-year-old Caucasian female with past medical history of gastroesophageal reflux disease presented with abdominal pain and irregular bowel habits with a tendency for diarrhea for 6 months. She had intermittent abdominal pain. She had two loose bowel movements daily without any blood or mucus. She lost 20 pounds of weight during this time. She had been on a gluten free diet for 3 months with partial improvement. She was on omeprazole 20 mg for heartburn for 6 months. On examination, she had mild epigastric tenderness. CBC was normal except for a mild increase in the lymphocyte count. Antigliadin antibody IgG was elevated. Anti-tissue transglutaminase IgA was normal but total IgA level was low. Due to the abnormal serology for celiac disease and irregular bowel habits, esophagogastroduodenoscopy and colonoscopy was done. EGD suggested gastritis and duodenitis. Colonoscopy was normal. The gastric biopsy showed significant thickening of sub-epithelial collagen (Fig. 1) and chronic inflammation consistent with collagenous gastritis. The duodenal biopsy showed preservation of villous architecture with mildly increased intraepithelial lymphocytic inflammation consistent with focal mild lymphocytic duodenitis (Fig. 2). As she was already on omeprazole with a gluten free diet, a follow-up visit in 3 months was planned. She reported partial improvement in her symptoms after 3 months. Her abdominal pain resolved but she still reported three loose bowel movements per day.
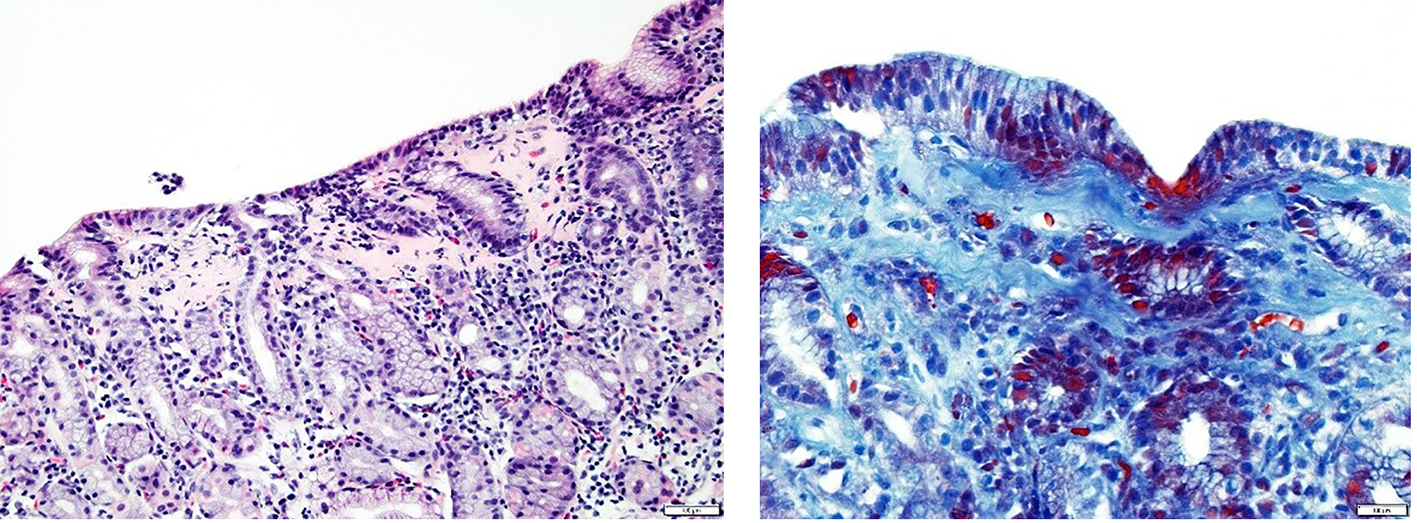 Click for large image | Figure 1. Gastric biopsy showing significant thickening of sub-epithelial collagen. |
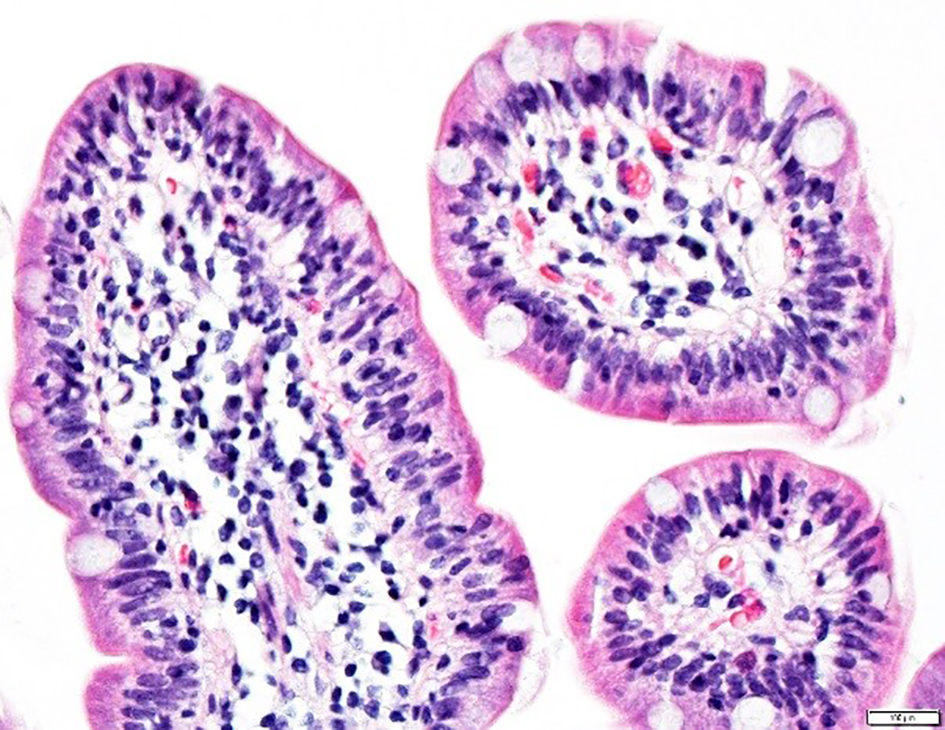 Click for large image | Figure 2. Duodenal villi with increased intraepithelial lymphocytes. |
| Discussion | ▴Top |
Collagenous gastritis without colonic involvement is very rare. The clinical symptoms may include abdominal pain, diarrhea, nausea, vomiting, weight loss, abdominal distension, gastrointestinal bleeding and fatigue. The clinical picture is different in pediatric and adult age groups depending on the site of gastrointestinal tract involvement. In the pediatric age group, it presents mostly with anemia and abdominal pain related to involvement of stomach [3]. In adults, it presents with chronic watery diarrhea due to coexisting collagenous colitis and more diffuse involvement of gastrointestinal tract involvement.
Adult collagenous gastritis is also associated with autoimmune diseases, such as systemic lupus erythematosus, ulcerative colitis, lymphocytic gastritis, and lymphocytic colitis. Due to this association, immune etiology has been postulated. Immune factors stimulate the production of extracellular matrix via production of growth factors and cytokines leading to collagen deposition. On EGD, gastric mucosa looks nodular with depressed mucosa in between nodules particularly in the body of stomach. The nodular mucosa is irregular in size and distribution with no significant inflammation. The depressed mucosa consists of inflammatory cells with atrophic glands, collagen bands and abnormal capillary vessels [4].
The collagenous gastritis is considered a chronic, intermittent to persistent histological disease with chronic, intermittent clinical course in the majority of adult patients. There are no reports of any association between collagenous gastritis and any malignancy, lymphoma or any other gastric disorders [4]. The course and prognosis of the disease is still unclear. The thickness of collagen bands has been associated with disease duration, but not with disease severity. However, in the majority of cases, the collagen deposits remain unchanged or become thicker due to continued inflammation. Due to the small number of cases reported and unclear etiology, no standard therapy has been established. Proton-pump inhibitors, oral corticosteroids and a gluten-free diet have been tried with limited success [5].
Funding Sources
None.
Competing Interests
None.
Author Contributions
All authors have directly participated in the execution in a manner substantial enough to take responsibility for it.
| References | ▴Top |
- Rosell-Camps A, Riera-Llodra JM, Colom-Segui M, Zibetti S, Amengual-Antich I. Collagenous gastritis in the pediatric age. Rev Esp Enferm Dig. 2015;107(5):313-315.
pubmed - Rustagi T, Rai M, Scholes JV. Collagenous gastroduodenitis. J Clin Gastroenterol. 2011;45(9):794-799.
doi pubmed - Ma C, Park JY, Montgomery EA, Arnold CA, McDonald OG, Liu TC, Salaria SN, et al. A Comparative Clinicopathologic Study of Collagenous Gastritis in Children and Adults: The Same Disorder With Associated Immune-mediated Diseases. Am J Surg Pathol. 2015;39(6):802-812.
doi pubmed - Kamimura K, Kobayashi M, Sato Y, Aoyagi Y, Terai S. Collagenous gastritis: Review. World J Gastrointest Endosc. 2015;7(3):265-273.
doi pubmed - Soeda A, Mamiya T, Hiroshima Y, Sugiyama H, Shidara S, Dai Y, Nakahara A, et al. Collagenous gastroduodenitis coexisting repeated Dieulafoy ulcer: A case report and review of collagenous gastritis and gastroduodenitis without colonic involvement. Clin J Gastroenterol. 2014;7(5):402-409.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


