| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website http://www.gastrores.org |
Case Report
Volume 3, Number 2, April 2010, pages 91-92
Nicorandil Induced Colonic Ulcer: A Late Complication?
Ravindra S Datea, b, Olatunde S. Owaa, Muntzer M Mughala
aDepartment of Gastrointestinal Surgery, Lancashire Teaching Hospitals NHS, Foundation Trust, Preston Road, Chorley, Lancashire, PR7 1PP, UK
bCorresponding author, Email:
Manuscript accepted for publication April 21, 2010
Short title: Nicorandil Induced Colonic Ulcer
doi: https://doi.org/10.4021/gr2010.04.191w
This article has been retracted
| Abstract | ▴Top |
Nicorandil is a third line treatment for ischemic heart disease. Oral and anal ulceration are recognized side effects of Nicorandil occurring within few months of commencing the treatment. Colonic ulcers are rare. We present a case of an 82-year-old woman who developed colonic ulcers 8 years after commencing on Nicorandil. The ulcers healed within 6 months of discontinuing the treatment. The case may suggest colonic ulceration as long term effect of the drug.
Keywords: Nicorandil; Colon; Ulcer
| Introduction | ▴Top |
Nicorandil is used for the treatment of ischemic heart disease. Oral and anal ulcerations are rare but recognized side effects of the drug occurring within few months of commencement of the treatment [1, 2]. Colonic ulcers are even rarer [3, 4]. Exact pathogenesis of these ulcers is not known but it appears to be related to the dose of Nicarandil [5]. Relationship of ulcer with duration of treatment is not known.
We present a case of 82 years old lady who developed colonic ulcers 8 years after commencing on nicorandil for ischemic heart disease.
| Case report | ▴Top |
An 82-year-old lady was presented with abdominal pain and constipation. She had colonoscopy which revealed a 2 x 2 cm polyp at 22 cm. This was excised. Histology showed a tubulovillous adenoma with mild dysplasia. She had 2 further “follow-up” colonoscopies at 2 yearly intervals. These were normal. A further colonoscopy 3 years later showed circumferential ulcer at the junction of the proximal and middle third of transverse colon (Fig. 1). Histology showed non-specific inflammatory changes; there was no evidence of granulomata, dysplasia or neoplasia. Persistent ulceration was noted on 2 further colonoscopies at one year interval (Fig. 2). Biopsies were benign on both the occasions. The ulceration was thought to be secondary to mucosal prolapse.
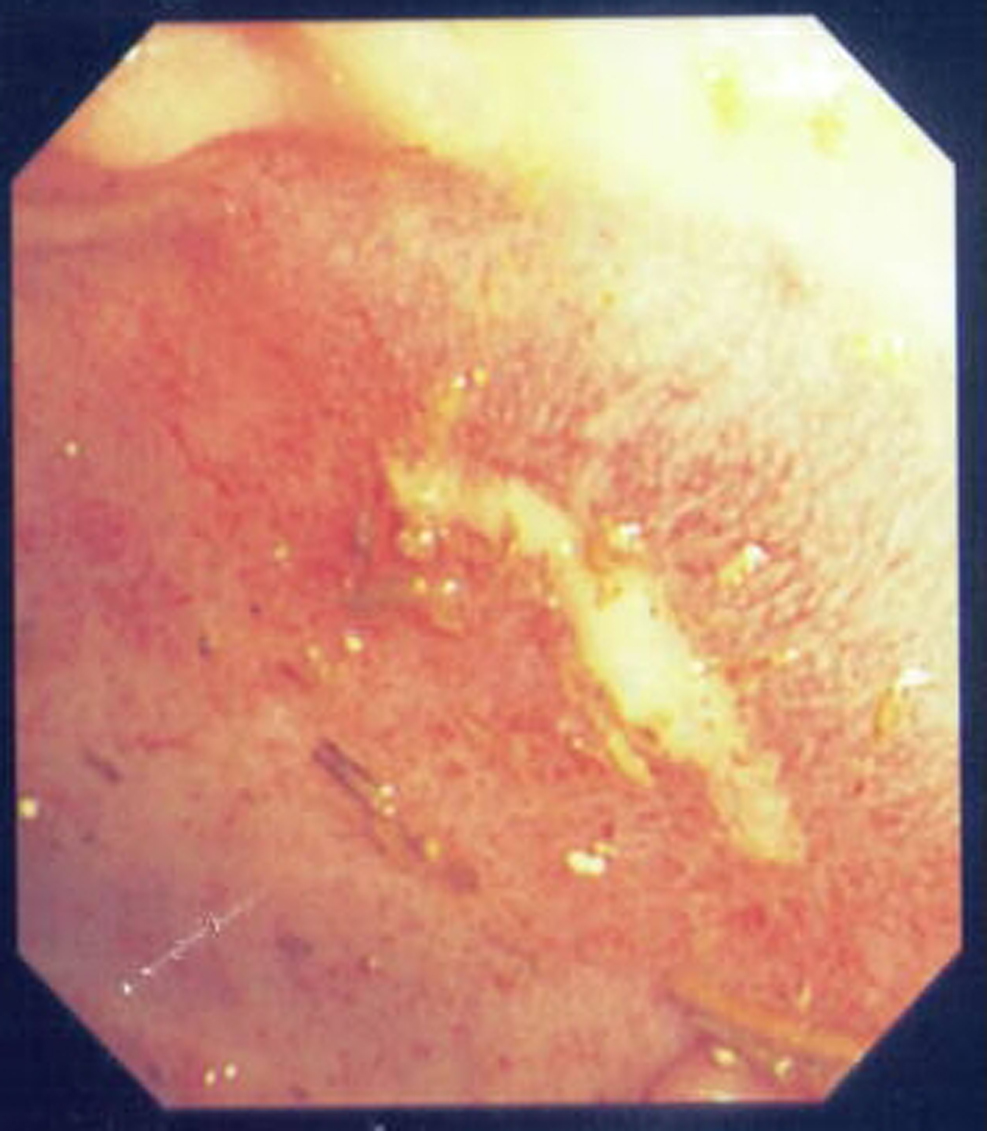 Click for large image | Figure 1. Ulceration in transverse colon noted 8 years after commencing Nicorandil. |
| Discussion | ▴Top |
Nicorandil, a potassium activator is a third line drug in the treatment of severe ischaemic heart disease [4]. It acts by relaxing the smooth muscle of the blood vessels, causing both arterial and venous vasodilatation. Its use has been associated with oral and anal ulcerations [6, 7], but ulcers at other sites in gastrointestinal tract have also been described [8, 9].
Pathogenesis of these ulcers is not known, but they appear to be related to the dose of Nicorandil and resolve upon withdrawal of the drug with median healing time of 12 weeks. Other proposed mechanisms are vascular steal phenomenon and direct local effect of either Nicorandil itself or its metabolite [5].
Most of the oral ulcers develop within few months of commencing the Nicorandil [10]. Our patient though on a high dose of Nicorandil developed ulcers in the colon 8 years after commencingtreatment, suggesting that this may be a long term effect of the drug. Her 3 colonoscopies during these 8 years did not show any evidence of ulceration. Healing of ulcer on discontinuing the medication confirmed the etiological role of Nicorndil.
Nicorandil should be considered in the differential diagnosis of idiopathic gastrointestinal ulceration to avoid unnecessary surgical intervention. Physicians prescribing the drug should be aware of this side effect. This drug is used for ischemic heart disease and patients using this are also more likely to be on anticoagulants which increase the risk of bleeding from ulcers. Surgeons treating the patients with per rectal bleeding should consider discontinuing Nicorandil along with anticoagulation in appropriate circumstances.
Most of the ulcers develop within few months of commencing the Nicorandil [10]. Our patient developed ulcer in colon 8 years after commencing the treatment suggesting that this may be a long term effect of the drug.
Competing Interests
None to declare.
| References | ▴Top |
- Abdelrazeq AS, Owen C, Smith L, McAdam JG, Pearson HJ, Leveson SH. Nicorandil-associated para-stomal ulceration: Case series. Eur J Gastroenterol Hepatol. 2006;18(12):1293-1295.
pubmed doi - Egred M. Nicorandil-associated ulcerations. Eur J Gastroenterol Hepatol. 2007;19(5):395-398.
pubmed doi - Brown R, Lee A, Welfare M. Nicorandil-induced colonic ulceration. Heart. 2008;94(5):678.
pubmed doi - Titi MA, Seow C, Molloy RG. Nicorandil-Induced Colonic Ulceration: A New Cause of Colonic Ulceration. Report of Four Cases. Dis Colon Rectum 2008.
pubmed - Toquero L, Briggs CD, Bassuini MM, Rochester JR. Anal ulceration associated with Nicorandil: case series and review of the literature. Colorectal Dis. 2006;8(8):717-720.
pubmed doi - Watson A, Suttie S, Fraser A, O'Kelly T, Loudon M. Nicorandil associated anal ulceration. Colorectal Dis. 2004;6(5):330-331.
pubmed doi - Webster K, Godbold P. Nicorandil induced oral ulceration. Br Dent J. 2005;198(10):619-621.
pubmed doi - Egred M, Andron M, Morrison WL. Nicorandil may be associated with gastrointestinal ulceration. Bmj. 2006;332(7546):889.
pubmed doi - King PM, Suttie SA, Jansen JO, Watson AJ. Perforation of the terminal ileum: a possible complication of nicorandil therapy. Surgeon. 2004;2(1):56-57.
pubmed doi - Gupta A, Morris G. Major aphthous ulcers induced by nicorandil. Age Ageing. 2000;29(4):372-373.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


