| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 17, Number 3, June 2024, pages 101-108
Needle-Knife Fistulotomy Versus Needle-Knife Papillotomy in Difficult Biliary Cannulation: A Systematic Review and Meta-Analysis
Saqr Alsakarneha, g, Tim Brothertonb, Fouad Jabera, Mahmoud Y. Madib, Laith Numanb, Mohamed Ahmedc, Yazan Sallama, Mohammad Adama, Dushyant Singh Dahiyad, Pearl Aggarwale, Fazel Dinaryf
aDepartment of Medicine, University of Missouri-Kansas City, Kansas City, MO, USA
bDepartment of Gastroenterology and Hepatology, Saint Louis University, St. Louis, MO, USA
cDepartment of Gastroenterology and Hepatology, University of Missouri-Kansas City, Kansas City, MO, USA
dDivision of Gastroenterology, Hepatology & Motility, The University of Kansas School of Medicine, Kansas City, Kansas, USA
eDepartment of Medicine, University Hospitals, Cleveland, OH, USA
fDepartment of Gastroenterology and Hepatology, University Hospitals, Cleveland, OH, USA
gCorresponding Author: Saqr Alsakarneh, Department of Medicine, University of Missouri-Kansas City, Kansas City, MO 64108, USA
Manuscript submitted April 5, 2024, accepted April 25, 2024, published online June 29, 2024
Short title: NKF vs. NKP for Difficult Biliary Cannulation
doi: https://doi.org/10.14740/gr1726
| Abstract | ▴Top |
Background: Endoscopic retrograde cholangiopancreatography (ERCP) is an essential endoscopic therapeutic modality for biliary and pancreatic diseases. Needle-knife fistulotomy (NKF) and papillotomy (NKP) are the two most commonly used rescue techniques for patients with difficult biliary cannulation. However, there remains a need for comparative studies on these approaches to inform clinical decision-making. This meta-analysis aimed to evaluate the efficacy and safety of NKF compared to NKP as a rescue technique in difficult biliary cannulation after failed conventional ERCP.
Methods: We searched PubMed, Scopus, Embase, and Web of Science databases through November 2023 to include all studies that directly compared the outcomes of NKF with NKP in difficult biliary cannulation. Single-arm studies were excluded. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) for dichotomous data related to clinical events were calculated using the Mantel-Haenszel method within a random-effect model. The primary outcome was the biliary cannulation success rate.
Results: Four studies with 823 patients (n = 376 NKF vs. n = 447 NKP) were included in our analysis. There was no significant difference between the two groups in biliary cannulation success rate (91.7% vs. 86.9%, respectively; OR = 1.54, 95% CI: 0.21 - 2.49, P = 0.14; I2 = 0%). However, the overall rate of adverse events was significantly lower in the NKF group than in the NKP group (OR = 0.46, 95% CI: 0.25 - 0.84, P = 0.01). Pancreatitis (OR = 0.23, 95% CI: 0.05 - 1.11, P = 0.07) and bleeding (OR = 1.43, 95% CI: 0.59 - 3.46, P = 0.42) were similar between the two groups. No significant differences in cholangitis, cholecystitis, perforation, or mortality were observed.
Conclusions: Our meta-analysis indicates comparable success rates in comparing NKF and NKP techniques for difficult biliary cannulation after failed conventional ERCP cannulation. Notably, the NKF technique significantly reduces overall adverse events compared to NKP, suggesting that NKF may be preferable due to its favorable safety profile. Additional randomized controlled trials (RCTs) are warranted to evaluate the interval benefit of an NKF technique.
Keywords: ERCP; Needle-knife; Fistulotomy; Papillotomy
| Introduction | ▴Top |
Endoscopic retrograde cholangiopancreatography (ERCP) is an essential endoscopic therapeutic modality for a multitude of biliary and pancreatic diseases. Biliary cannulation is one of the most technically challenging portions of the procedure with failed biliary cannulation being associated with a higher rate of adverse events [1].
Multiple attempts at cannulation increase risk of post-ERCP pancreatitis (PEP) and time under anesthesia [2]. In rare cases, PEP is severe enough to lead to fatality. Success rate of biliary cannulation depends on the experience of the endoscopist. Even among experienced endoscopists, the failure rate can reach 10-20% [2-4].
Factors contributing to difficult biliary cannulation include size and location of the duodenal papilla, presence of duodenal diverticulum, surgically altered anatomy (e.g., Roux-en-Y), and any other factor that leads to malposition of the papilla (e.g., infiltrating tumor) [1]. When standard biliary cannulation techniques fail, a precut technique can be utilized to increase successful cannulation rate. Needle-knife fistulotomy (NKF) and papillotomy (NKP) are the two most commonly used precut techniques [5].
However, there remains a need for comparative studies on these approaches to inform clinical decision-making. This meta-analysis aimed to evaluate the efficacy and safety of NKF compared to NKP as a rescue technique in difficult biliary cannulation after failed conventional ERCP.
| Materials and Methods | ▴Top |
Search strategy and study eligibility
Two independent reviewers (SA and FJ) conducted a systematic search of studies published before November 30, 2023, reporting on outcomes of rescue techniques after failed standard ERCP biliary cannulation. We systematically searched the online MEDLINE, Embase, Web of Sciences, and Scopus databases using key words in different combination: “precut”, “rescue precut”, “needle knife fistulotomy”, “needle knife papillotomy”, “ERCP”, and “endoscopic retrograde cholangiopancreatography”. In addition, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), we screened the reference lists of the articles and corresponded with study investigators [6]. No language restrictions were applied, as long as study outcomes were reported in the text. A third reviewer (MM) resolved any disagreement.
Study inclusion and exclusion
We used the following criteria in this analysis: prospective or retrospective studies which evaluated patients with failed ERCP (patient population) who underwent rescue precut, either NKF or NKP (intervention), where clinical safety and efficacy were reported (outcomes). Only studies that compare NKF with NKP were included.
The study was excluded if the precut procedure (NKF or NKP) was used as the primary technique or the study was a case report, case series with less than 10 sample sizes, animal study, editorial, meta-analysis, or review article. Studies without relevant clinical data on clinical success or adverse events were excluded.
Data extraction and quality assessment
All relevant data were extracted according to predefined table independently by SA and FJ. The following parameters were extracted: first author, year of publication, country, study design, patient demographics, technical success, functional success, and outcomes of interest. Using the Newcastle-Ottawa Scale, the methodological quality of the included cohort studies was assessed independently by two investigators (SA and LN). In a case of discrepancy, a third independent individual (MM) was consulted.
Definitions of outcomes
In the NKF technique, the incision begins approximately 3 - 5 mm above the papilla, following the alignment of the biliary axis back to the orifice [7]. In contrast, NKP involves cutting the major papilla from the orifice towards the 11:00 o’clock position [8]. All outcomes were assessed for the NKF and NKP groups. The primary outcomes were the pooled rates and odds ratios (ORs) for successful biliary cannulation with NKF versus NKP and pooled ORs of PEP with NKF versus NKP after failed ERCP. Secondary outcomes were to compare the overall adverse events and bleeding, perforation, asymptomatic hyperamylasemia, and cholangitis, individually, with NKF versus NKP. The American Society for Gastrointestinal Endoscopy lexicon for grading of severity of procedural adverse events with endoscopy were used to define adverse events.
Data synthesis and statistical analysis
We used R, version 3.2.3 (R Project for Statistical Computing), with Meta and Metaprop packages for all analyses. Using the Freeman-Turkey double arcsine transformation (FTT) method, the pooled, weight-adjusted event rate estimate for the clinical outcomes in each group were calculated using Metaprop package. Between-study heterogeneity was assessed using the Cochrane Q-statistic (I2), which represents the percentage of total between-study variation that cannot be attributed solely to chance. Between-study heterogeneity was rated as low if 25% < I2 ≤ 50%, moderate if 50% < I2 ≤ 75%, and high if I2 > 75%. A leave-1-out meta-analysis was performed to assess the influence of the outcome by excluding each study and identifying influential studies that may contribute to heterogeneity. Statistical tests were two-sided and used a significance threshold of P < 0.05. The assessment of publication bias was investigated by evaluation of funnel plot asymmetry and sensitivity analysis. In addition to the ethical standards of the competent institution for human subjects, this meta-analysis was conducted in compliance with the Helsinki Declaration [9].
Ethical approval
The data utilized in this study is available publicly. Hence, an analysis did not require Institutional Review Board (IRB) approval as per guideline put forth by our institutional IRB.
| Results | ▴Top |
Literature search and study characteristics
A total of 97 unique records were identified according to the above search strategy. After title and abstract screening, four studies with a total of 823 patients were included in the study. PRISMA flowchart illustrates our selection process as shown in Figure 1. All studies compared patients undergoing NKF (376 patients) and NKP (447 patients). Further details on patient characteristics, etiology, and study outcomes are presented in Tables 1 and 2 [7, 10-12]. Two studies were randomized controlled trials (RCTs), and two studies were retrospective cohort studies. All patients in the NKF and NKP groups underwent at least one attempt of ERCP biliary cannulation before performing NKF or NKP. Table 1 [7, 10-12] shows the baseline characteristics of the included studies and their quality analysis. Three studies were from Greece and one study was from China. Two studies were considered high quality and two studies moderate quality based on the Newcastle-Ottawa scale for study quality assessment (Table 1) [7, 10-12].
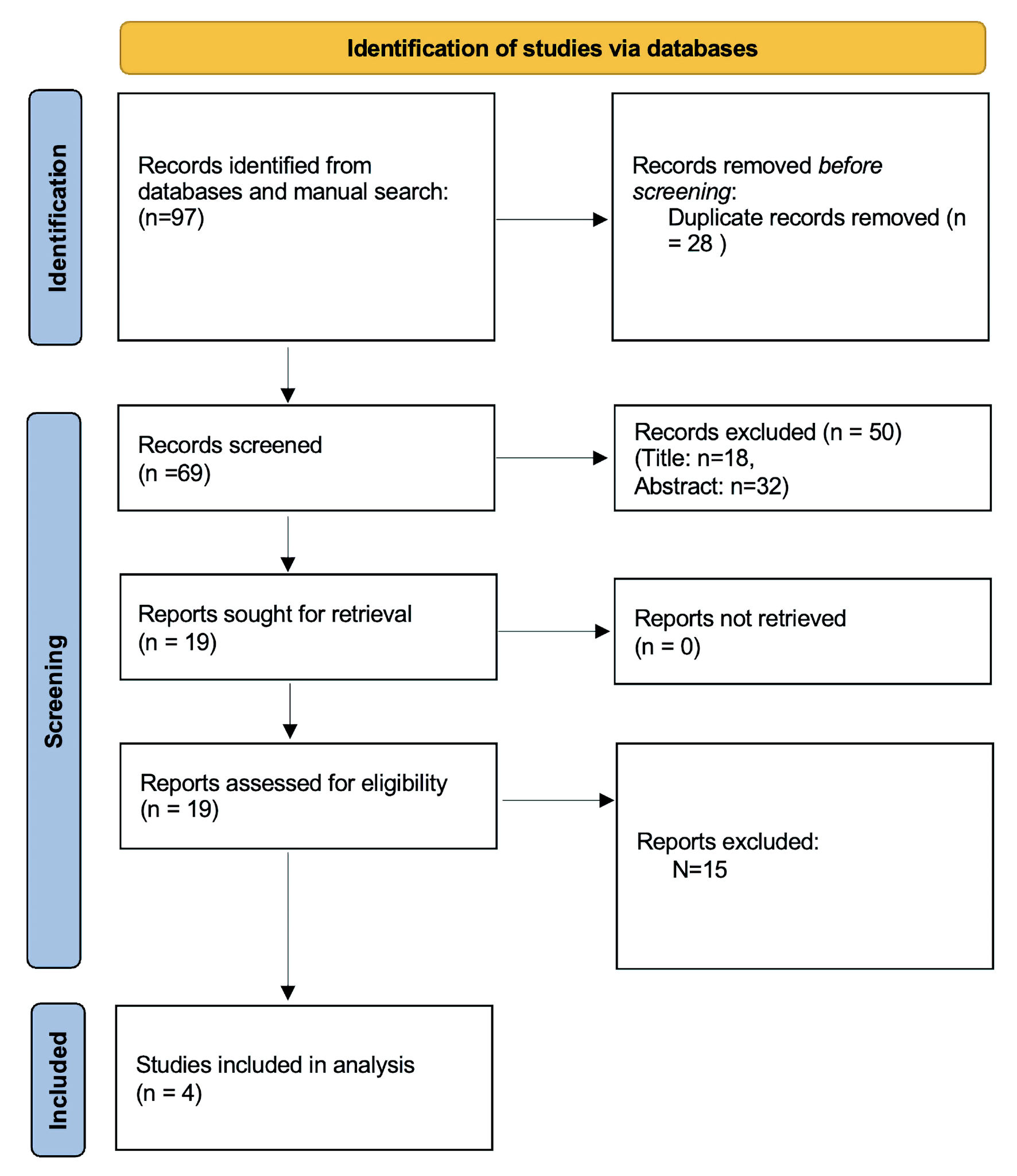 Click for large image | Figure 1. PRISMA flow chart of study inclusion. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses. |
 Click to view | Table 1. Characteristics of Included Studies |
 Click to view | Table 2. Individual Complications and Biliary Cannulation Success Rate |
Biliary cannulation success rate
The primary outcome was a comparison of biliary cannulation success rate between NKF and NKP technique after failed biliary cannulation. There was no significant difference between the two groups in the initial biliary cannulation success rate (91.7% vs. 86.9%, respectively; OR =1.54, 95% CI: 0.21 - 2.49, P = 0.14). Forest plot is shown in Figure 2.
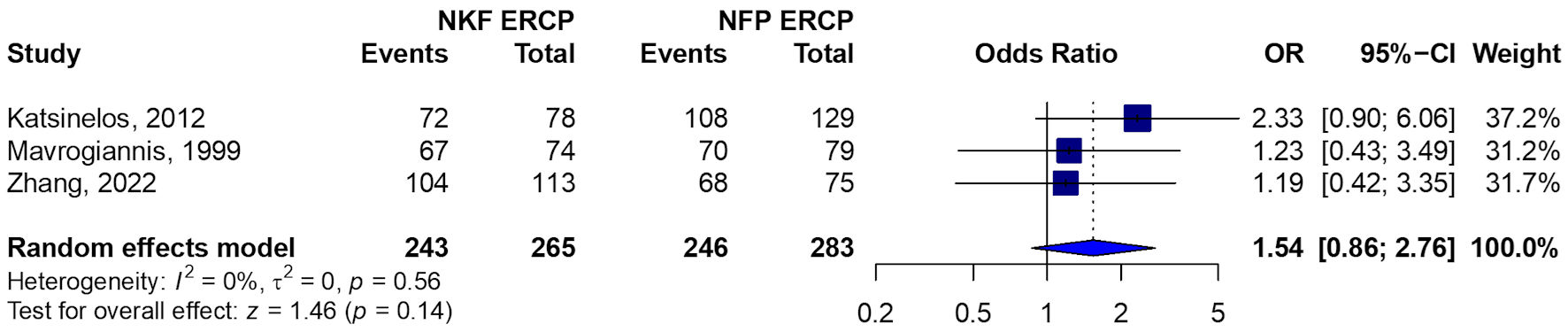 Click for large image | Figure 2. Forest plot of biliary cannulation success rate. NKF: needle-knife fistulotomy; NFP: needle-knife papillotomy; ERCP: endoscopic retrograde cholangiopancreatography; OR: odds ratio; CI: confidence interval. |
Adverse events
The pooled overall rate of adverse events was significantly lower in the NKF group than NFP group (OR = 0.46, 95% CI: 0.25 - 0.84, P = 0.01). Pooled studies were homogenous in the overall adverse events rate among included studies (I2 = 40%, P = 0.17). Forest plot is shown in Figure 3a.
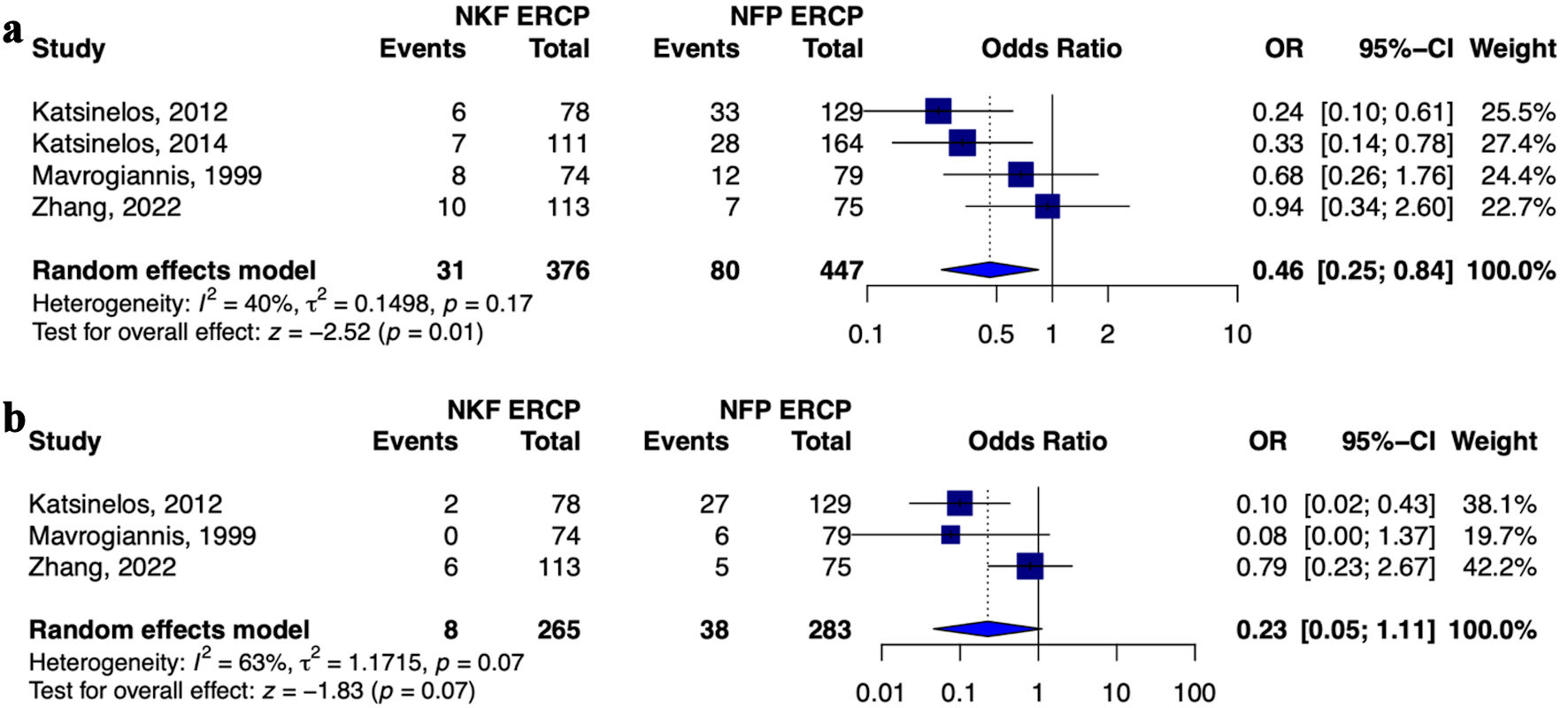 Click for large image | Figure 3. Forest plot of (a) overall rate of adverse events and (b) post-ERCP pancreatitis. NKF: needle-knife fistulotomy; NFP: needle-knife papillotomy; ERCP: endoscopic retrograde cholangiopancreatography; OR: odds ratio; CI: confidence interval. |
The pooled incidence of pancreatitis was comparable between the two groups (OR = 0.23, 95% CI: 0.05 - 1.11, P = 0.07). Pooled studies were homogenous (I2 = 0%, P = 0.95). Forest plot is shown in Figure 3b. No significant differences were observed in terms of bleeding (OR = 1.43, 95% CI: 0.59 - 3.46, P = 0.42), cholangitis, cholecystitis, perforation, or mortality (Table 2) [7, 10-12].
Assessment of publication bias and sensitivity analysis
Publication bias was not assessed with funnel plots as the number of studies included in the analysis was < 10. The influence of a single study on the overall meta-analysis estimate was investigated by omitting one study at a time. The omission of any study resulted in no significant difference, indicating that our results were statistically reliable.
| Discussion | ▴Top |
ERCP plays a prominent role in the management of pancreatic and biliary diseases. Endoscopic biliary cannulation was first described in 1968 as a means to visualize the ampulla of Vater [13]. The first endoscopic sphincterotomy was performed in 1974 by Kawai and Claussen and remains a primary tool for successful cannulation [14]. ERCP was initially only used diagnostically, however, most ERCPs are now performed with a therapeutic intent [15, 16].
PEP is the most common complication of ERCP, occurring in an estimated 1-7% of patients [17-21]. Difficult biliary cannulation is a recognized risk factor for PEP [19]. Precut biliary access is a time-saving technique that also has potential to reduce the rate of PEP in patients with difficult biliary cannulation [22, 23]. Before deciding to use a precut technique, several factors must be considered such as how critical the indication of the ERCP is, patient’s general clinical condition, level of expertise of the endoscopist, and what other techniques are available.
In the comparison of NKF and NKP for difficult biliary cannulation, our meta-analysis indicates comparable success rates. Both RCTs included in this analysis showed similar cannulation success rates for NKF and NKP [7, 10]. For Zhang et al, NKP was selected for patients with small and flat papilla, and NKF was selected for patients with normal and swollen papilla [10]. This was decided on a modification of a prior classification of the morphology of the major duodenal papilla [24]. In the study by Mavrogiannis et al, patients were randomized to NKF or NKP by the sealed-envelope method [7].
Some endoscopists speculate that NKF is safer as it avoids thermal injury to the papilla thereby preserving outflow of pancreatic secretions and mitigating risk of PEP [11, 25]. However, the rate of PEP was similar between the two groups. Interestingly, Mavrogiannis et al [7] found a significant increase in PEP in the NKP group, whereas there was no difference between the groups in the study by Zhang et al [10]. While the NKF approach may indeed lead to fewer injuries to the pancreatic duct orifice, it is important to note that the boundaries between NKF and NKP are not always clearly delineated, particularly in cases involving small papillae [26]. This implies benefit in the individualized approach on the basis of major duodenal papilla morphology. While an individualized approach may be optimal, this might not be commonplace in clinical practice due to endoscopist comfort with one technique over the other and due to a lack of consensus on the matter.
Katsinelos et al identified both NFK and NKP as risk factors for PEP [12]. Sub-analysis showed that risk is higher with NKP as compared to NKF [12]. This was attributed to the fact that thermal injury and papilla edema were avoided and so maintaining the flow of pancreatic enzymes, a mechanism which is thought to be contributory to PEP. Another analysis showed that risk of pancreatitis is actually due to the fact that NKP technique is typically undertaken after repeated cannulation attempts with possible pancreatic duct cannulations or inadvertent pancreatic injections rather than to the injury induced by NKP itself [10]. In a prospective controlled trial, Swan et al compared early NKP to continued standard cannulation (CSC) in difficult biliary access cases [27]. The incidence of PEP was associated with both increased time until successful cannulation and a greater number of cannulation attempts. PEP rates were not significantly different in the CSC and NKP techniques arms.
The NKF approach shows a marked decrease in overall adverse events in comparison to NKP. However, when examining individual occurrences such as pancreatitis, cholangitis, cholecystitis, and perforation, the rates were similar between the two groups. This parity might be attributed to the limited sample size of the studies. The cumulative total of these incidents resulted in a significant overall adverse event rate.
The strengths of this meta-analysis include a comprehensive search of multiple databases by two independent reviewers. Limitations of this meta-analysis include the low number of included studies, variability in study type (two retrospective studies and two RCTs), and variability in time spent attempting standard biliary cannulation before pursuing a precut technique. Also, three of the included studies were from Greece, and only one study was from China. One of the included studies was from 1999, when canulation techniques were much more difficult. There is also variability in endoscopist experience and skill among the different studies. Confounding variables such as patient history of PEP or other independent risk factors for pancreatitis were not available for analysis and could not be assessed. Ideally, the same criteria would be applied regarding the decision to proceed with NKP or NKF, and this would occur at the same time interval following attempted standard biliary cannulation as repeat attempts at standard cannulation lead to trauma and edema of the papilla.
The international consensus recommendations for difficult biliary access emphasize the importance of considering alternative techniques when facing challenges in accessing the biliary system [29]. They caution against persisting with the same approach, as this increases the risk of additional injury to the papilla. Specifically, they advocate for the judicious use of precut techniques when deemed appropriate. Our study contributes additional insights into the utilization of these techniques, demonstrating their efficacy and safety in clinical practice.
In conclusion, this systemic review and meta-analysis suggests an NKF technique is the safer option for difficult biliary cannulation. Our results align with the European Society of Gastrointestinal Endoscopy, who recommends NKF as the preferred technique in difficult biliary cannulation [29]. Patients may benefit from an individualized approach on the basis of the anatomy of the major duodenal papilla. Additional RCTs are warranted to evaluate the interval benefit of an NKF technique.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
Authors have no conflict of interest.
Informed Consent
Informed consent was deemed inappropriate for this research.
Author Contributions
Conception and design: Saqr Alsakarneh, Mahmoud Y. Madi, Dushyant Singh Dahiya, Fazel Dinary. Administrative support: Saqr Alsakarneh, Mahmoud Y. Madi, Dushyant Singh Dahiya, and Laith Numan. Provision, collection, and assembly of data: Saqr Alsakarneh, Mahmoud Y. Madi, Dushyant Singh Dahiya, Fouad Jaber, Mohammad Ahmed, Yazan Sallam, Mohamed Adam, and Pearl Aggrawal. Statistical analysis: Saqr Alsakarneh. Review of literature, drafting the manuscript, and revision of key components of manuscript: all authors. Final approval of manuscript and agreement to be accountable for all aspects of the work: all authors.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Berry R, Han JY, Tabibian JH. Difficult biliary cannulation: Historical perspective, practical updates, and guide for the endoscopist. World J Gastrointest Endosc. 2019;11(1):5-21.
doi pubmed pmc - Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, et al. Are we meeting the standards set for endoscopy? Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007;56(6):821-829.
doi pubmed pmc - Varadarajulu S, Kilgore ML, Wilcox CM, Eloubeidi MA. Relationship among hospital ERCP volume, length of stay, and technical outcomes. Gastrointest Endosc. 2006;64(3):338-347.
doi pubmed - Tse F, Yuan Y, Moayyedi P, Leontiadis GI. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2012;12(12):CD009662.
doi pubmed pmc - Chen J, Wan JH, Wu DY, Shu WQ, Xia L, Lu NH. Assessing quality of precut sphincterotomy in patients with difficult biliary access: an updated meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2018;52(7):573-578.
doi pubmed - Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
doi pubmed pmc - Mavrogiannis C, Liatsos C, Romanos A, Petoumenos C, Nakos A, Karvountzis G. Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones. Gastrointest Endosc. 1999;50(3):334-339.
doi pubmed - Rollhauser C, Johnson M, Al-Kawas FH. Needle-knife papillotomy: a helpful and safe adjunct to endoscopic retrograde cholangiopancreatography in a selected population. Endoscopy. 1998;30(8):691-696.
doi pubmed - World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194.
doi pubmed - Zhang QS, Xu JH, Dong ZQ, Gao P, Shen YC. Success and safety of needle knife papillotomy and fistulotomy based on papillary anatomy: a prospective controlled trial. Dig Dis Sci. 2022;67(5):1901-1909.
doi pubmed - Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, Terzoudis S, et al. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27(1):65-72.
pubmed pmc - Katsinelos P, Gkagkalis S, Chatzimavroudis G, Beltsis A, Terzoudis S, Zavos C, Gatopoulou A, et al. Comparison of three types of precut technique to achieve common bile duct cannulation: a retrospective analysis of 274 cases. Dig Dis Sci. 2012;57(12):3286-3292.
doi pubmed - McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-756.
doi pubmed pmc - Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20(4):148-151.
doi pubmed - Robison LS, Varadarajulu S, Wilcox CM. Safety and success of precut biliary sphincterotomy: Is it linked to experience or expertise? World J Gastroenterol. 2007;13(15):2183-2186.
doi pubmed pmc - Ahmed M, Kanotra R, Savani GT, Kotadiya F, Patel N, Tareen S, Fasullo MJ, et al. Utilization trends in inpatient endoscopic retrograde cholangiopancreatography (ERCP): A cross-sectional US experience. Endosc Int Open. 2017;5(4):E261-E271.
doi pubmed pmc - Alsakarneh S, Jaber F, Ahmed K, Ghanem F, Mohammad WT, Ahmed MK, Almujarkesh MK, et al. Incidence and cross-continents differences in endoscopic retrograde cholangiopancreatography outcomes among patients with cirrhosis: a systematic review and meta-analysis. Gastroenterology Res. 2023;16(2):105-117.
doi pubmed pmc - Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37(3):383-393.
doi pubmed - Mallery JS, Baron TH, Dominitz JA, Goldstein JL, Hirota WK, Jacobson BC, Leighton JA, et al. Complications of ERCP. Gastrointest Endosc. 2003;57(6):633-638.
doi pubmed - Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335(13):909-918.
doi pubmed - Alsakarneh S, Jaber F, Mohammed W, Jr., Almeqdadi M, Al-Ani A, Kilani Y, Abughazaleh S, et al. Applicability of child-turcotte-pugh score in anticipating post-ERCP adverse events in patients with cirrhosis: a systematic review and meta-analysis. J Clin Gastroenterol. 2024.
doi pubmed - Lopes L, Dinis-Ribeiro M, Rolanda C. Early precut fistulotomy for biliary access: time to change the paradigm of "the later, the better"? Gastrointest Endosc. 2014;80(4):634-641.
doi pubmed - Mariani A, Di Leo M, Giardullo N, Giussani A, Marini M, Buffoli F, Cipolletta L, et al. Early precut sphincterotomy for difficult biliary access to reduce post-ERCP pancreatitis: a randomized trial. Endoscopy. 2016;48(6):530-535.
doi pubmed - Canena J, Lopes L, Fernandes J, Costa P, Arvanitakis M, Koch AD, Poley JW, et al. Influence of a novel classification of the papilla of Vater on the outcome of needle-knife fistulotomy for biliary cannulation. BMC Gastroenterol. 2021;21(1):147.
doi pubmed pmc - Katsinelos P, Lazaraki G, Gkagkalis S, Chatzimavroudis G, Fasoulas K, Zavos C, Pilpilidis I, et al. Predictive factors for post-ERCP pancreatitis: a large-scale single expertized endoscopist study. Surg Laparosc Endosc Percutan Tech. 2014;24(6):512-516.
doi pubmed - Chan TT, Chew MCH, Tang RSY. Troubleshooting difficult bile duct access: advanced ERCP cannulation techniques, percutaneous biliary drainage, or EUS-guided rendezvous technique? Gastroenterology Insights. 2021;12(4):405-422.
- Swan MP, Alexander S, Moss A, Williams SJ, Ruppin D, Hope R, Bourke MJ. Needle knife sphincterotomy does not increase the risk of pancreatitis in patients with difficult biliary cannulation. Clin Gastroenterol Hepatol. 2013;11(4):430-436.e431.
doi pubmed - Liao WC, Angsuwatcharakon P, Isayama H, Dhir V, Devereaux B, Khor CJ, Ponnudurai R, et al. International consensus recommendations for difficult biliary access. Gastrointest Endosc. 2017;85(2):295-304.
doi pubmed - Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Deviere J, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(7):657-683.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


