| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Case Report
Volume 16, Number 3, June 2023, pages 195-200
Takotsubo Cardiomyopathy Associated With Acute Pancreatitis
Samyak Dhruva, e, Shravya Ginnaramb, Arhum Shahc, Don C. Rockeyd
aMedStar St. Mary’s Hospital, Leonardtown, MD, USA
bAbington Hospital, Jefferson Health, Abington, PA, USA
cDepartment of Physiology, Georgetown University, Washington DC, USA
dDigestive Disease Research Center, Medical University of South Carolina, Charleston, SC, USA
eCorresponding Author: Samyak Dhruv, MedStar St. Mary’s Hospital, Leonardtown, MD, USA
Manuscript submitted May 2, 2023, accepted May 23, 2023, published online June 11, 2023
Short title: TCM Associated With Acute Pancreatitis
doi: https://doi.org/10.14740/gr1633
| Abstract | ▴Top |
Takotsubo cardiomyopathy is classically associated with emotional stress in middle-aged women. In clinical practice, physical stressors are a more common cause of Takotsubo cardiomyopathy. Here, we present two patients who had acute pancreatitis as a physical stressor that caused Takotsubo cardiomyopathy, and an additional 13 cases identified in the literature. An important clinical feature of these cases is that because metabolic derangements are often encountered, close attention to electrolyte repletion with cardiac monitoring is indicated.
Keywords: Troponin; Gallstones; Echocardiography; Abdominal pain; Shortness of breath
| Introduction | ▴Top |
Takotsubo cardiomyopathy (TCM) or stress-induced cardiomyopathy was first described in Japan in 1990 and is characterized by acute transient reversible left ventricular systolic dysfunction with apical distension [1]. It often mimics acute coronary syndrome in the absence of obstructive coronary artery disease. Typically, physical or emotional stress acts as a trigger of TCM. Among the documented triggers of TCM, acute pancreatitis has been previously reported, though uncommonly [2]. Here, we present two additional patients with severe acute pancreatitis that led to TCM.
| Case Reports | ▴Top |
Case 1
A 41-year-old man was admitted to the hospital with epigastric abdominal pain radiating to the back, nausea and vomiting for 1 day. His past medical history was notable for alcohol use of five to seven drinks of vodka daily for several years. Vital signs in the emergency room were as follows: heart rate (HR) 110 beats/min, blood pressure (BP) 123/80 mm Hg, respiratory rate (RR) 16/min and temperature 37 °C. Mucous membranes were dry. Abdominal examination demonstrated bowel sounds in all quadrants, and epigastric tenderness without guarding or rigidity. Initial laboratory data were as follows: lipase 200 IU/L, aspartate aminotransferase (AST) 235 IU/L, alanine aminotransferase (ALT) 154 IU/L, alkaline phosphatase 72 IU/L, total bilirubin 0.8 mg/dL, direct bilirubin 0.3 mg/dL, blood urea nitrogen (BUN) 15 mg/dL, creatinine 1.33 mg/dL, magnesium 1.0 mg/dL, potassium 3.0 mg/dL, hemoglobin 13.9 g/dL, white blood cell (WBC) 4.8 × 103/µL and platelet count of 117 × 103/µL. Computed tomography (CT) of the abdomen and pelvis with contrast showed a normal acinar pattern of the pancreas with a borderline dilated common bile duct (CBD) of 9 mm in diameter and fatty infiltration of the liver. No gallstones were identified. Ultrasound abdomen was performed which showed CBD diameter of 7 mm without any gallstones or CBD stones. A clinical diagnosis of acute pancreatitis likely secondary to alcohol use was made per Atlanta criteria. Intravenous (IV) Ringer’s lactate solution (LR), thiamine, folate, and multivitamin were started with the banana bag. The Clinical Institute Withdrawal Assessment of Alcohol Scale (CIWA) protocol was started for alcohol withdrawal. Despite aggressive electrolyte repletion, the patient remained agitated the next day with ongoing evidence of intravascular volume depletion, and new T wave inversions were identified on telemetry monitor confirmed with 12-lead electrocardiography (ECG) (Fig. 1). Troponin levels showed a marked increase to 300 ng/L (14 ng/L on admission). He underwent an emergent cardiac catheterization which showed no significant epicardial coronary artery disease. (Fig. 2). Transthoracic echocardiogram showed a severely reduced left ventricular function with an ejection fraction (EF) of 25-30%, apical ballooning and akinesia of the mid-apical myocardium consistent with TCM (Fig. 3) Lisinopril and carvedilol were begun and the patient slowly improved. Extensive counseling regarding alcohol cessation was given and resources were provided to help with his alcohol use disorder. He was discharged home with instructions to follow up with cardiology outpatient but failed to present for further medical care.
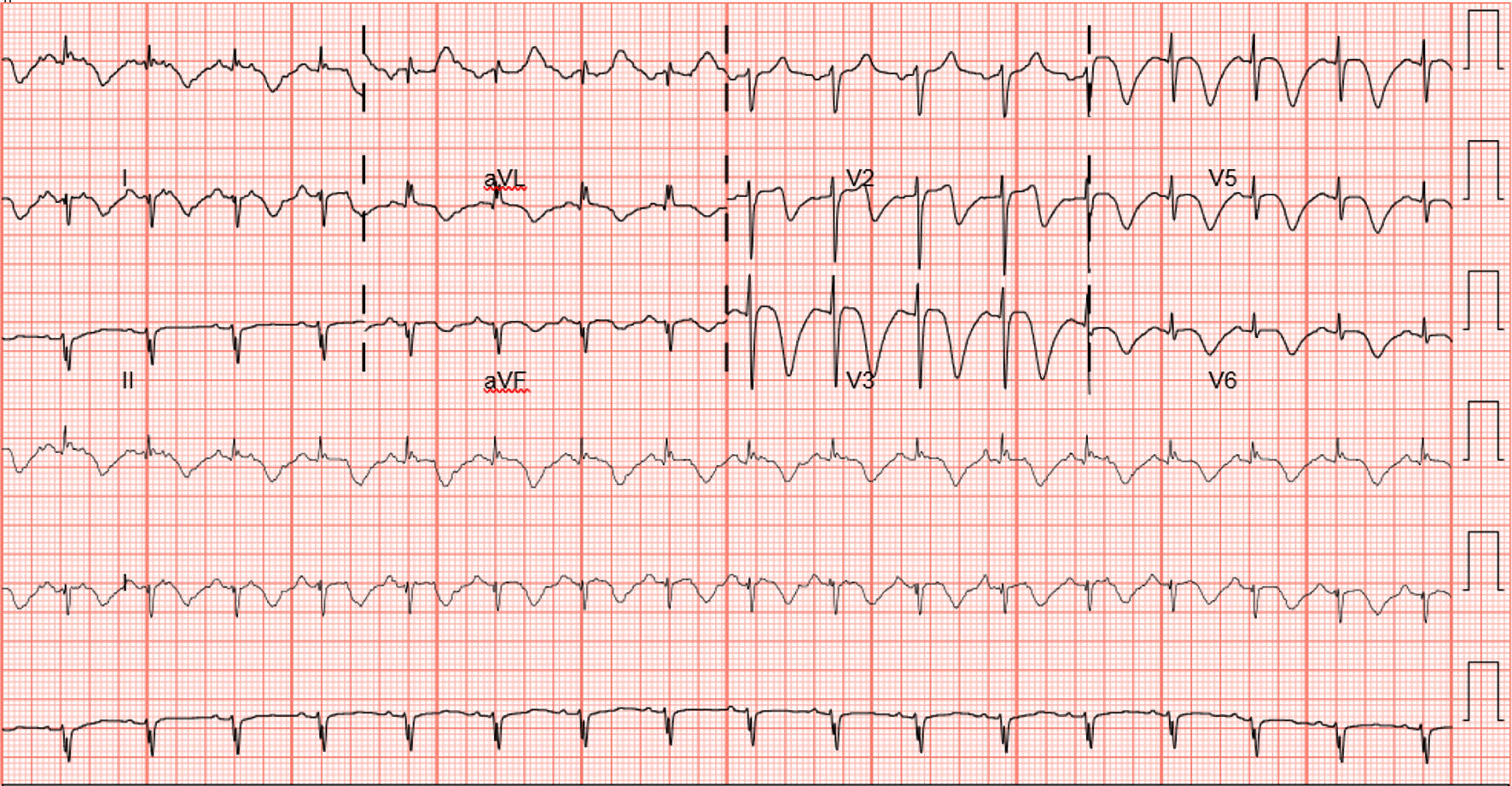 Click for large image | Figure 1. ECG showing diffuse deep T wave inversions suggestive of ischemia (case 1). ECG: electrocardiography. |
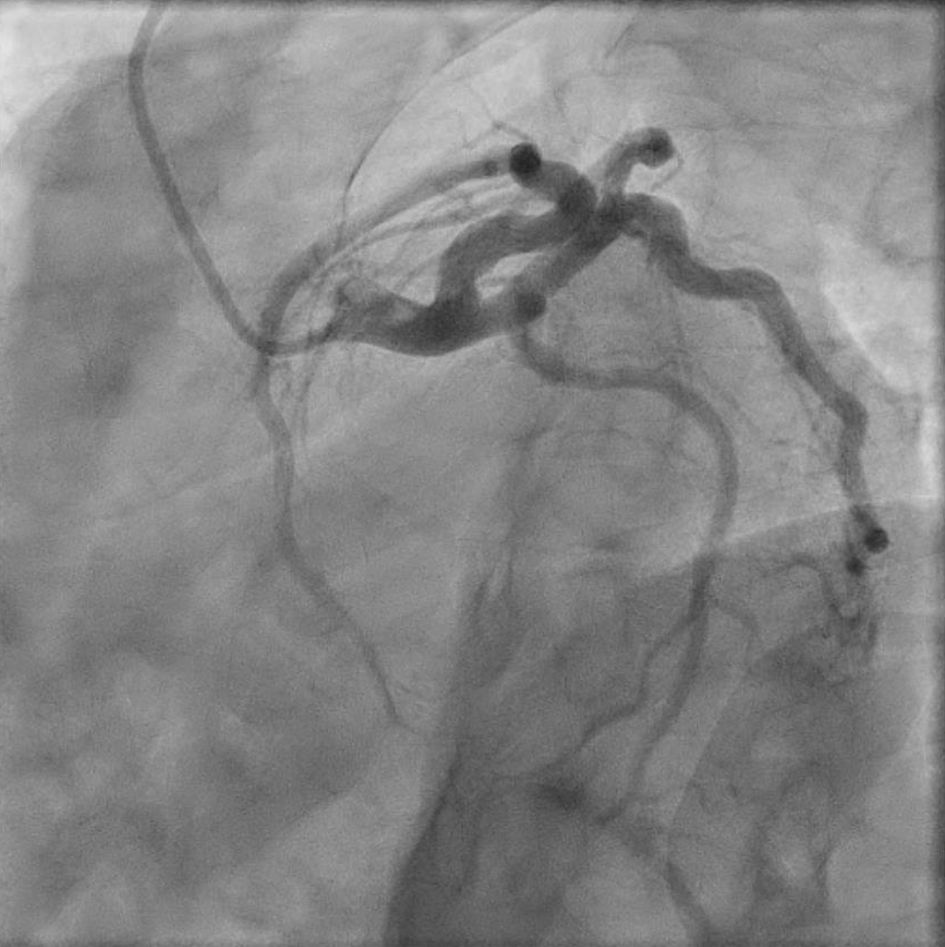 Click for large image | Figure 2. Normal coronary angiogram of the patient consistent with Takotsubo cardiomyopathy (case 1). |
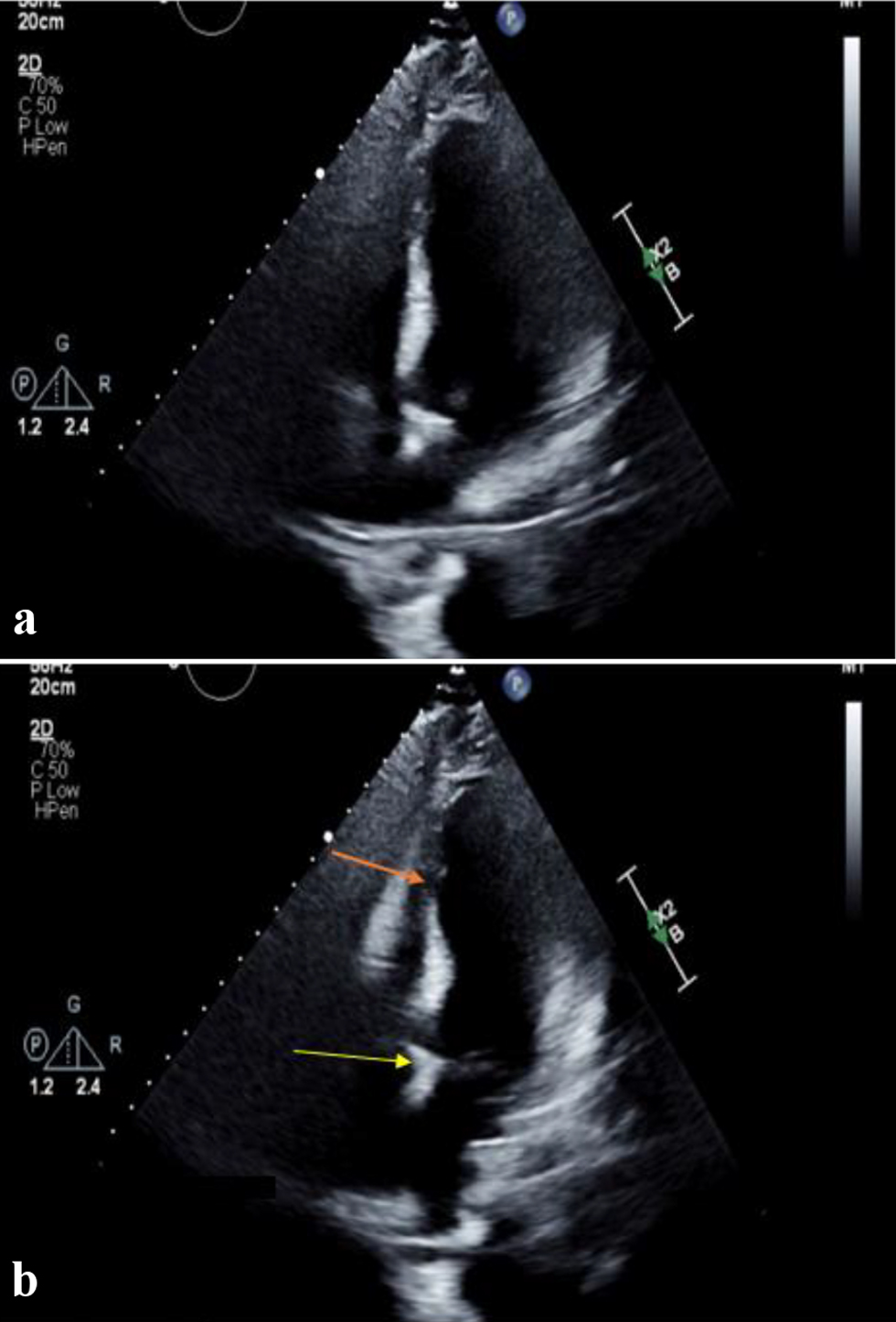 Click for large image | Figure 3. Four-chamber view of left ventricle in (a) diastole and (b) systole, showing hypercontractile basal segment (yellow arrow) with apical ballooning (orange arrow) consistent with Takotsubo cardiomyopathy (case 1). |
Case 2
A 41-year-old woman with the past medical history of hypertension treated with nifedipine presented with acute onset of right upper quadrant and epigastric pain radiating to the back. On presentation, she had a HR of 140/min, BP 142/90 mm Hg, RR of 16/min and temperature of 36.8 °C. Abdominal examination was notable for right upper quadrant and epigastric tenderness. Initial laboratory results in the emergency room were as follows: AST 21 IU/L, ALT 13 IU/L, alkaline phosphatase 92 IU/L, total bilirubin 0.5 mg/dL, direct bilirubin 0.2 mg/dL, BUN < 5 mg/dL, creatinine 0.55 mg/dL, magnesium 1.5 mg/dL, potassium 2.7 mg/dL, complete blood count was remarkable for a WBC of 13 × 103/µL and hemoglobin of 9.2 g/dL, lipase was 67 U/L and lactic acid was 3.3 mmol/L. Ultrasound of the abdomen showed gallstones without evidence of cholecystitis. Magnetic resonance cholangiopancreatography (MRCP) revealed a CBD of 5 mm in diameter without evidence of obstruction, and edema but was consistent with acute pancreatitis. The patient was started on IV normal saline and made nil per os (NPO). Lactic acid normalized with IV hydration and her HR decreased to 80/min. On the day after admission, the patient complained of having shortness of breath and developed hypotension with BP of 92/60 mm Hg. Chest X-ray showed pulmonary edema. ECG showed new diffuse T wave inversions (Fig. 4) and the patient’s troponin levels were > 800 ng/L (normal on admission). The patient was started on diuretic therapy. Transthoracic echocardiography (ECHO) showed a severely reduced left ventricular function with an EF of 35% with global hypokinesis that was most pronounced at the cardiac apex (Fig. 5). Emergency cardiac catheterization was performed which showed normal coronary arteries and the patient was diagnosed with TCM. An angiotensin-converting enzyme inhibitor and carvedilol were begun, with improvement in her shortness of breath (SOB); she was discharged with outpatient follow-up with cardiology team. One month later, the patient presented with midepigastric abdominal pain, at which time transthoracic echocardiogram was normal.
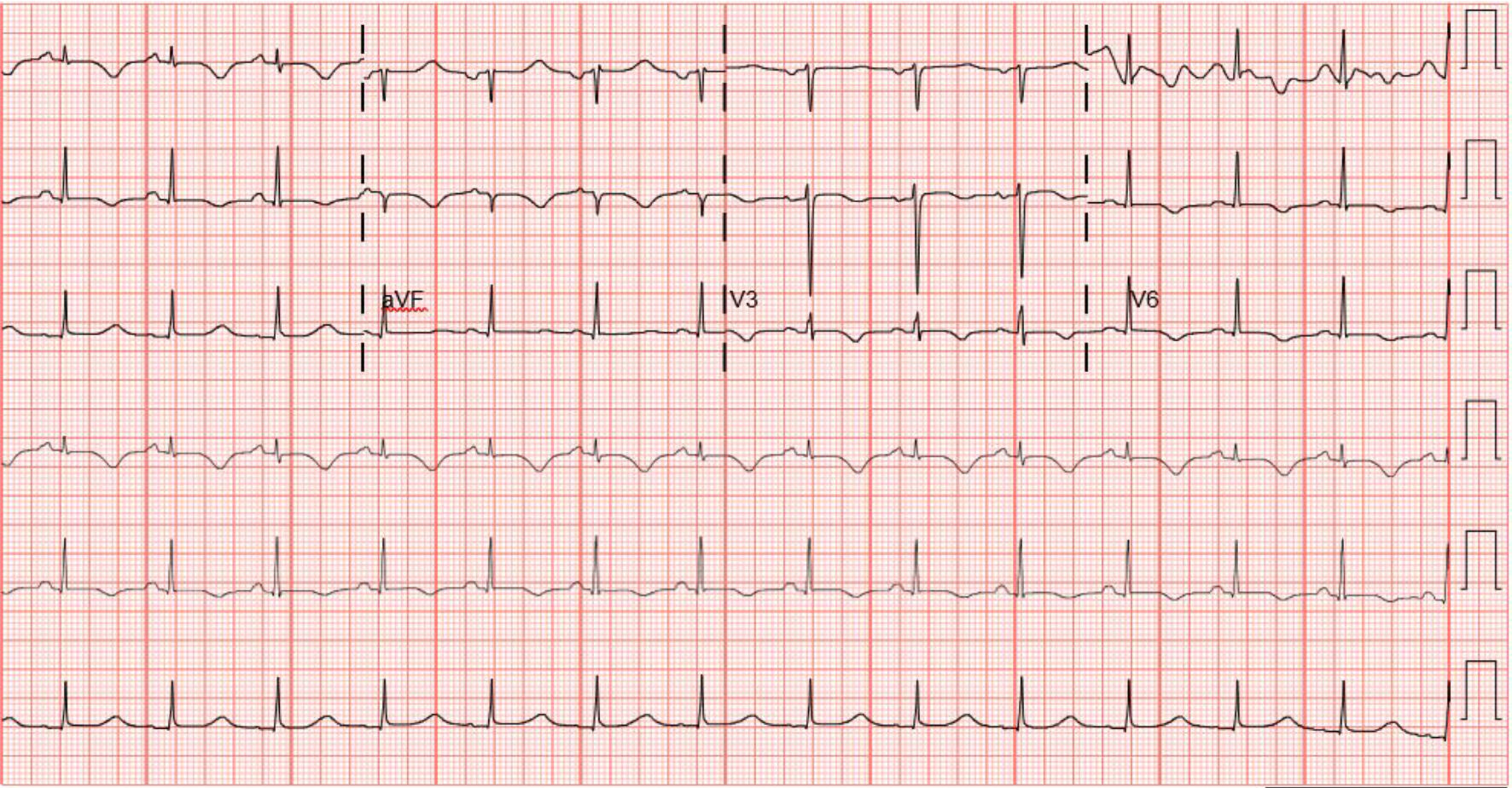 Click for large image | Figure 4. ECG showing diffuse T wave inversion suggestive of ischemia (case 2). ECG: electrocardiography. |
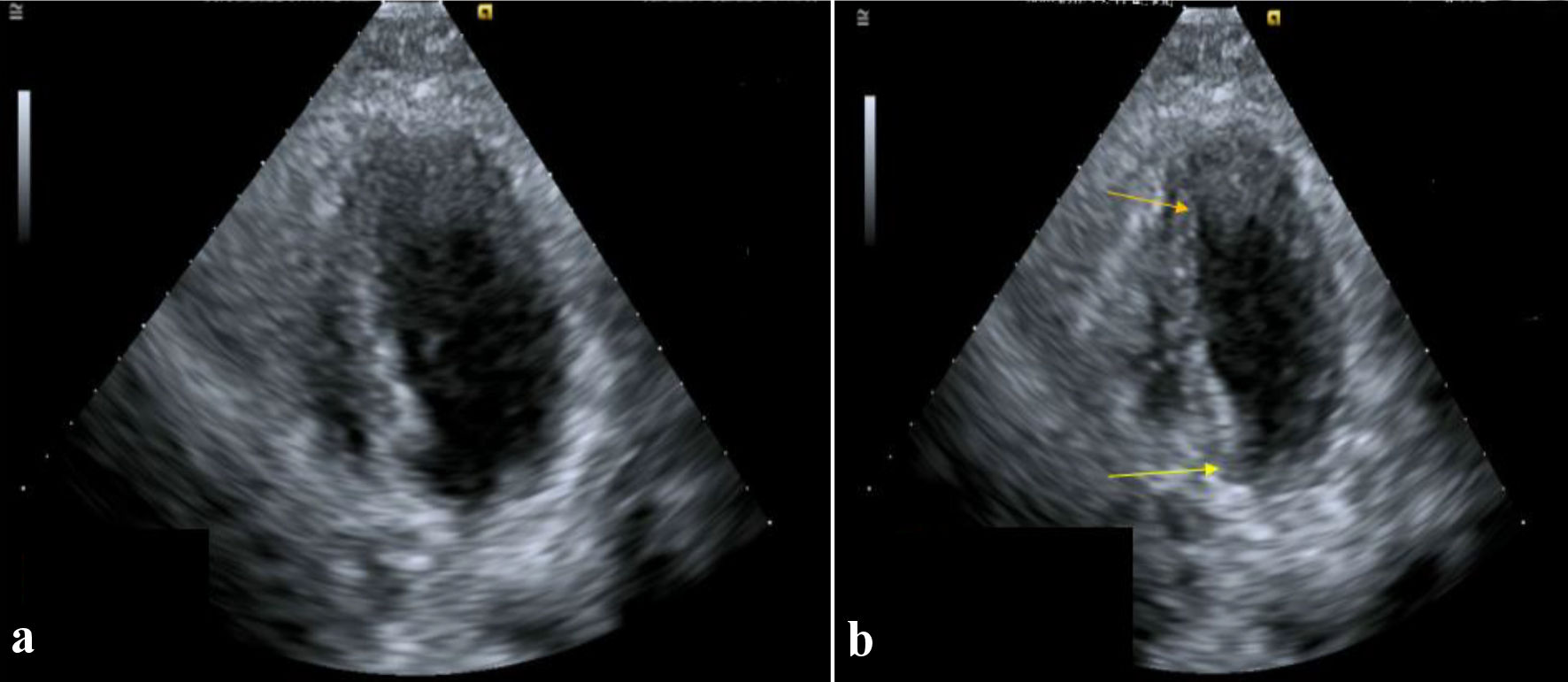 Click for large image | Figure 5. Four-chamber view of left ventricle in (a) diastole and (b) systole, showing hypercontractile basal segment (yellow arrow) with apical ballooning (orange arrow) consistent with Takotsubo cardiomyopathy (case 2). |
| Discussion | ▴Top |
TCM is a clinical syndrome characterized by transient left ventricular dysfunction causing apical akinesis/ballooning resembling an octopus fishing trap (Takotsubo) on ECHO. It is thought to be triggered by a sudden unexpected physical/emotional stressor or trauma [3]. The cause of regional differences in contractility is unknown though regional differences in catecholamine-induced vasoconstriction, innervation and difference in adrenergic sensitivity have been proposed as potential mechanisms [3]. Additionally, distributive shock, which is typical of acute pancreatitis can cause transient cardiac microvascular hypoperfusion and likely contribute to TCM in our patients. Experimental studies in rats with pancreatitis have demonstrated edema in the cardiac interstitium, cardiomyocyte hypoxia, over-contracted myofibrils, intracellular edema, cardiomyocyte hypertrophy and deposition of extracellular matrix in the stroma [4].
Acute pancreatitis as a physical stressor causing TCM has only been reported in 13 cases in the literature. In the current report, we have identified two additional cases of TCM that occurred during an acute episode of pancreatitis (Table 1) [2, 5-16]. We speculate that relative intravascular volume depletion typical of pancreatitis led to adrenergic stress and transient cardiac microvascular hypoperfusion, which in turn caused cardiac dysfunction. In both patients, TCM resolved.
 Click to view | Table 1. Patients Reported in the Literature with Takotsubo Cardiomyopathy |
Ten out of the 13 previously reported TCM cases with pancreatitis have been in middle-aged or elderly women, most of whom were predisposed to gallstone pancreatitis. This is consistent with the current body of literature that suggests that a large proportion of TCM cases occur among postmenopausal women, perhaps due to the cardio-protective role of estrogen in younger women and downregulation of beta receptors in cardiac myocytes which is lost with estrogen loss [17, 18]. Younger males have also been diagnosed with TCM, as in our first patient. This was the fourth reported case described among males where TCM was associated with the pancreatitis. Presumably, the absence of estrogen and a higher degree of sympathetic activation leads to a stress-induced catecholamine surge that is required to initiate TCM. Consequently, there is a high risk of acute phase events including heart failure, in-hospital complications, and mortality among males with TCM [19, 20]. The median age for pancreatitis TCM is 57 years with almost 70% of cases being more than 50 years of age.
Electrolyte disturbances, especially hypomagnesemia and hypokalemia are common in patients with chronic alcoholism-related pancreatitis; such electrolyte abnormalities are particularly important because they may predispose patients to cardiac complications. The association between electrolyte abnormalities and TCM however has not been examined extensively in the literature. It is likely that the catecholamine surge in response to stress evokes an efflux of magnesium, leading to a depletion in magnesium stores, an increase in intracellular calcium, subsequent cell death, altered contractility and fatal arrhythmias. As potassium influx is essential for cardiac repolarization, hypokalemia lengthens the action potential and QT interval increasing the risk for fatal ventricular arrhythmia [21].
Interestingly, the diagnosis of TCM in our first patient was made incidentally when the rhythm changes were identified on the telemetry monitoring. Therefore, it could be argued that patients with pancreatitis and electrolyte abnormalities or those with clinical evidence of unexpected stress, be monitored on the telemetry so that cardiac rhythm changes can be identified early, and appropriate management can be pursued in a timely manner. Our case is the first in literature where a patient was diagnosed with TCM with pancreatitis even before any cardiac symptoms developed, showing the importance of telemetry monitoring in these pancreatitis’ cases. There are cases in the literature where young patients with pancreatitis and TCM have been inappropriately treated with thrombolysis because of a strong suspicion of acute coronary event [2]. This would appear to be unfortunate since this could readily predispose the patient to potential bleeding complications. We speculate that there may be a role for early cardiac ECHO, CT angiography or perhaps an early cardiac magnetic resonance imaging (MRI) in patients with suspected TCM to help clarify the diagnosis.
In review of the previous cases of TCM, almost all cases of TCM developed within 1 week of acute pancreatitis, typically with the acute onset shortness of breath and chest pain. Presentations were typical, with documented reductions in the left ventricular EF < 35% with apical hypokinesis and hypercontractile basal segments. None of them had any evidence of coronary artery disease in the angiography. The outcome of TCM secondary to pancreatitis has been favorable and only one patient had a cardiac arrest which was followed by cardiogenic shock, eventually requiring a left ventricular-assisted device [5].
Learning points
In summary, we present two patients who had acute pancreatitis that caused TCM and review an additional 13 cases identified in the literature. In both of our patients, acute electrolyte abnormalities were prominent, and may have contributed to the pathogenesis of TCM. We suggest that patients with pancreatitis and electrolyte abnormalities be monitored with cardiac telemetry, at least until electrolyte disturbances are corrected.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed patient consent was obtained to publish the article.
Author Contributions
Samyak Dhruv is the main and corresponding author. He came up with the idea to publish these rare cases. He prepared the manuscript, edited it and finalized the draft. Shravya Ginnaram helped with image editing and help with finalizing the table Arhum Shah helped with editing the images. Don C. Rockey is the attending gastroenterologist on the case. He helped with editing and finalizing the draft.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Sato H, Tateishi H, Uchida T, et al. Tako-tsubo-like left ventricular dysfunction due to multivessel coronary spasm. In: Kodama K, Haze K, Hori M, editors. Clinical aspect of myocardial injury: from ischemia to heart failure (in Japanese). Tokyo: Kagakuhyoronsha Publishing Co, 1990; p. 56-64.
- Yeh J, Carroll J. Takotsubo cardiomyopathy complicating acute pancreatitis: a case report. BMC Gastroenterol. 2021;21(1):134.
doi pubmed pmc - Assad J, Femia G, Pender P, Badie T, Rajaratnam R. Takotsubo syndrome: a review of presentation, diagnosis and management. Clin Med Insights Cardiol. 2022;16:11795468211065782.
doi pubmed pmc - Luo Y, Li Z, Ge P, Guo H, Li L, Zhang G, Xu C, et al. Comprehensive mechanism, novel markers and multidisciplinary treatment of severe acute pancreatitis-associated cardiac injury - a narrative review. J Inflamm Res. 2021;14:3145-3169.
doi pubmed pmc - Koop AH, Bailey RE, Lowman PE. Acute pancreatitis-induced takotsubo cardiomyopathy and cardiogenic shock treated with a percutaneous left ventricular assist device. BMJ Case Rep. 2018;2018:bcr-2018-225877.
doi pubmed pmc - Sankri-Tarbichi AG, Mathew PK, Matos M, Hsi D. Stress-related cardiomyopathy. Heart Lung. 2007;36(1):43-46.
doi pubmed - Rajani R, Przedlacka A, Saha M, de Belder A. Pancreatitis and the broken heart. Eur J Emerg Med. 2010;17(1):27-29.
doi pubmed - Cheezum MK, Willis SL, Duffy SP, Moawad FJ, Horwhat JD, Huffer LL, Welch TS. Broken pancreas, broken heart. Am J Gastroenterol. 2010;105(1):237-238.
doi pubmed - Sudden Cardiac Death from Takotsubo Cardiomyopathy Triggered by Acute Pancreatitis. Abstract published at Hospital Medicine 2010, April 8-11, Washington, D.C.. Abstract 331 Journal of Hospital Medicine, Volume 5, Suppl 1. https://shmabstracts.org/abstract/sudden-cardiac-death-from-takotsubo-cardiomyopathy-triggered-by-acute-pancreatitis/. June 7th 2023.
- Leubner JK, Ortiz Z, Wolfrey J, Drake L. Can gallstones break the heart? Pancreatitis-induced Takotsubo cardiomyopathy mimicking acute myocardial infarction. J Am Geriatr Soc. 2014;62(9):1814-1815.
doi pubmed - Bruenjes JD, Vallabhajosyula S, Vacek CJ, Fixley JE. Acute pancreatitis-induced takotsubo cardiomyopathy in an African American male. ACG Case Rep J. 2015;3(1):53-56.
doi pubmed pmc - Boulos P. An inflamed pancreas and a broken heart: pancreatitis-induced Takotsubo cardiomyopathy. J Hosp Med. 2015;10:A349.
- Garbowska M, Kurek K, Sobkowicz B. Takotsubo cardiomyopathy resulting from exacerbation of chronic pancreatitis. Folia Cardiologica. 2016;11(5):473-476.
- Abe T, Simien M, Dolphurs H. Acute pancreatitis complicated by stress cardiomyopathy with persistent apical akinesis: a case report and literature review. J Investig Med High Impact Case Rep. 2019;7:2324709619893197.
doi pubmed pmc - Ashraf S, Lam K, Hu G. When your pancreas breaks your heart: a case of pancreatitis induced Takotsubo Cardiomyopathy. In: B52. critical care case reports: the liver, pancreas and intestines. American Thoracic Society. 2019. p. A3568-A3568.
- Khan Z. A case report of endoscopic retrograde cholangiopancreatography (ERCP) and acute pancreatitis induced takotsubo cardiomyopathy (TCM) in a patient with gallstones induced acute pancreatitis and cholangitis. Cureus. 2022;14(5):e24708.
doi pubmed pmc - Khalid N, Ahmad SA, Shlofmitz E, Chhabra L. Racial and gender disparities among patients with Takotsubo syndrome. Clin Cardiol. 2019;42(1):19.
doi pubmed pmc - Moolman JA. Unravelling the cardioprotective mechanism of action of estrogens. Cardiovasc Res. 2006;69(4):777-780.
doi pubmed - Khalid N, Ahmad SA, Umer A, Chhabra L. Factors impacting prognosis among patients with Tako-tsubo syndrome. Rev Esp Cardiol (Engl Ed). 2019;72(8):694.
doi pubmed - Arcari L, Nunez Gil IJ, Stiermaier T, El-Battrawy I, Guerra F, Novo G, Musumeci B, et al. Gender differences in takotsubo syndrome. J Am Coll Cardiol. 2022;79(21):2085-2093.
doi pubmed pmc - Andreozzi F, Cuminetti G, Karmali R, Kamgang P. Electrolyte disorders as triggers for takotsubo cardiomyopathy. Eur J Case Rep Intern Med. 2018;5(4):000760.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


