| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 16, Number 3, June 2023, pages 165-170
Trends of Upper Gastrointestinal Bleeding Mortality in the United States Before and During the COVID-19 Era: Estimates From the Centers for Disease Control WONDER Database
Nooraldin Merzaa, e , Ahmed Taher Masoudb, Zohaib Ahmeda, Dushyant Singh Dahiyac, Ali Nawrasd, Abdallah Kobeissyd
aDepartment of Internal Medicine, University of Toledo, Toledo, OH, USA
bDepartment of Internal Medicine, Fayoum University, Fayoum, Egypt
cDepartment of Internal Medicine, Central Michigan University College of Medicine, Saginaw, MI, USA
dDivision of Gastroenterology and Hepatology, University of Toledo, Toledo, OH, USA
eCorresponding Author: Nooraldin Merza, Department of Internal Medicine, University of Toledo, Toledo, OH, USA
Manuscript submitted April 13, 2023, accepted May 13, 2023, published online June 11, 2023
Short title: Trends of UGIB Mortality and COVID-19
doi: https://doi.org/10.14740/gr1626
| Abstract | ▴Top |
Background: There have been reports of increased upper gastrointestinal bleeding (UGIB) in patients with coronavirus disease 2019 (COVID-19). Still, only a few studies have examined the mortality rate associated with UGIB in the United States before and during COVID-19. Hereby, we explored the trends of UGIB mortality in the United States before and during COVID-19. The study’s objective was to investigate whether the COVID-19 pandemic significantly impacted UGIB mortality rates in the USA.
Methods: The decedents with UGIB were included. Age-standardized mortality rates were estimated with the indirect method using the 2000 US Census as the standard population. We utilized the deidentified data from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database. Linear regression analysis was performed to determine 2021 projected mortality rates based on trends between 2012 and 2019 to quantify the association of the pandemic with UGIB-related deaths.
Results: The mortality rate increased from 3.3 per 100,000 to 4.3 per 100,000 among the population between 2012 and 2021. There was a significant increase in the overall mortality rate between each year and the following year from 2012 to 2019, ranging from 0.1 to 0.2 per 100,000, while the rise in the overall mortality rate between each year and 2021 ranges from 0.4 to 0.9 per 100,000.
Conclusions: Our results showed that the mortality rate increased among the population between 2012and 2021, suggesting a possible influence of COVID-19 infection on the incidence and mortality of UGIB.
Keywords: Upper gastrointestinal bleeding; COVID-19; Trending mortality rate; CDC WONDER database
| Introduction | ▴Top |
Upper gastrointestinal bleeding (UGIB) is a potentially life-threatening medical condition affecting millions globally [1]. It is caused by various factors, including peptic ulcers, esophageal varices, and gastric cancer. UGIB is responsible for approximately 75% of all cases of acute gastrointestinal bleeding [2]. In the United States, UGIB is a significant cause of morbidity and mortality, with a mortality rate of approximately 10% [3-5].
Coronavirus disease 2019 (COVID-19) is a recent infectious viral disease that occurs due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 is usually an asymptomatic disease or presents with variable degrees of flu-like manifestations [6, 7]. It may progress to a severe and critical degree of respiratory distress which may be explained by the associated cytokine storm and cytotoxic effect of COVID-19 on the airway epithelium [8, 9].
The COVID-19 pandemic has raised concerns about increased mortality rates from UGIB for reasons that are not yet fully understood [10, 11]. SARS-CoV-2 was found to alter the patient’s coagulation profile and increase the risk of thrombosis and coagulopathy. Mainly because the natural anticoagulation mechanisms are downregulated due to the inflammatory processes initiated by the viral infection in addition to the endothelial damage, which releases the von Willebrand factor and activates complement [12-14]. Prolonged COVID-19-related hospital stays and using antithrombotic medications also played a role in altered coagulation profiles that may increase the risk of gastrointestinal bleeding. Moreover, corticosteroids and mechanical ventilation utilization, which may be required in severe COVID-19 infections, are significantly well-established risk factors for gastrointestinal bleeding [15, 16]. Additionally, during the pandemic, there were significant disruptions in healthcare delivery systems and delayed medical interventions [17-19].
To date, no sufficient studies have evaluated the UGIB mortality rate in the USA before and during the COVID-19 pandemic. Therefore, this study aimed to analyze death records and data from the Wide-Ranging Online Data for Epidemiologic Research (WONDER) database to assess the association between the COVID-19 pandemic and the change in the mortality rate among patients with UGIB.
| Materials and Methods | ▴Top |
This cross-sectional study used deidentified publicly available data, so informed consent and institutional review board approval were not required in accordance with the Common Rule. The study followed the STROBE reporting guideline [20]. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. We obtained deidentified data from the National Vital Statistics System (NVSS) through the Centers for Disease Control and Prevention (CDC) WONDER database [21]. The NVSS database registers more than 99% of deaths in the USA, and this study used data updated to January 22, 2022 [22]. Deaths from UGIB causes were identified by International Classification of Diseases, Tenth Revision (ICD-10) code (K92.0-K92.1-K92.2-I85.0-K22.1.K25.0-K25.2-K25.4-K25.6-K26.0-K26.2-K26.4-K26.6-K27.0-K27.2-K27.4-K27.6-K28.0-K28.2-K28.4-K28.6-K29.0-K63.8-K31.8-K29.7-K22.6-K22.8-K27.1), gender, and age. Individuals younger than age 25 years were excluded from the study.
We included decedents with UGIB, defined by ICD-10 diagnosis codes, as one cause of death (multiple causes were possible). Age-standardized mortality rates were estimated with the indirect method using the 2000 US Census as the standard population [23]. We performed linear regression analysis to determine 2021 projected mortality rates based on trends between 2012 and 2019. We quantified the association of the pandemic with UGIB-related deaths by calculating percentage differences between the projected and observed mortality rates. To enrich robustness, we also performed a sensitivity analysis by setting UGIB as the underlying (primary) cause of death. Statistical analyses were performed using the CDC WONDER database (age standardization), R version 4.0.2 (data cleaning and management), and PyCharm version 3.9.0 (modeling analysis).
| Results | ▴Top |
Table 1 and Figure 1 demonstrate the overall mortality rate from UGIB and the correlation between the mortality rate, age, and sex. The mortality rate increased from 3.3 per 100,000 to 4.3 per 100,000 among the population between 2012 and 2021. The youngest age group (25 - 44 years) showed the lowest mortality rate (0.28 per 100,000 in 2012 vs. 0.48 per 100,000 in 2021), while the oldest age group (65 - 84 years) showed the highest mortality rate (11.0 per 100,000 in 2012 vs. 13.13 per 100,000 in 2021) across all age groups. Regarding the sex of the population, the female group showed an elevation of the mortality rate from 3.3 per 100,000 in 2012 to 4.1 per 100,000 in 2021. The male group showed an elevation of the mortality rate from 3.3 per 100,000 in 2012 to 4.5 per 100,000 in 2021. The mortality rate in males (3.8 per 100,000 in 2016 and 4.5 per 100,000 in 2021) was higher than females between 2016 and 2021 (3.5 per 100,000 in 2016 and 4.1 per 100,00 in 2020). Regarding the yearly geographical trend, in 2021, the highest states with mortality rates were: Montana, Wyoming, West Virginia, and Mississippi (Fig. 2). The increase in the overall mortality rate between each year and the next year from 2012 to 2019 ranges from 0.1 to 0.2 per 100,000, while the increase in the overall mortality rate between each year and 2021 ranges from 0.4 to 0.9 per 100,000.
 Click to view | Table 1. Mortality Rate per 100,000 for Patients With UGIB From 2012 Through 2021 |
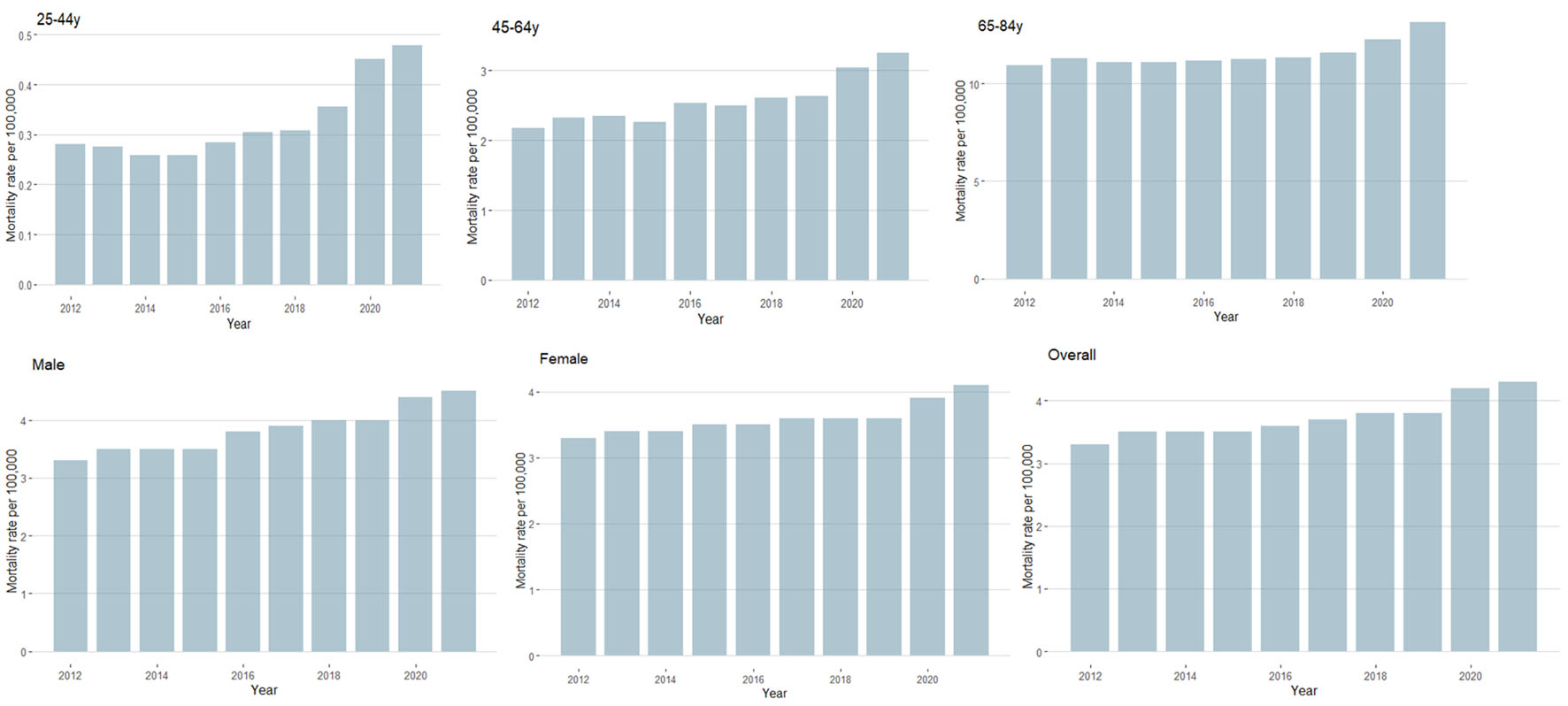 Click for large image | Figure 1. Trends in UGIB-related mortality before and during the COVID-19 pandemic, 2012 to 2021. Mortality rates are presented for decedent groups stratified by sex and age. UGIB: upper gastrointestinal bleeding; COVID-19: coronavirus disease 2019. |
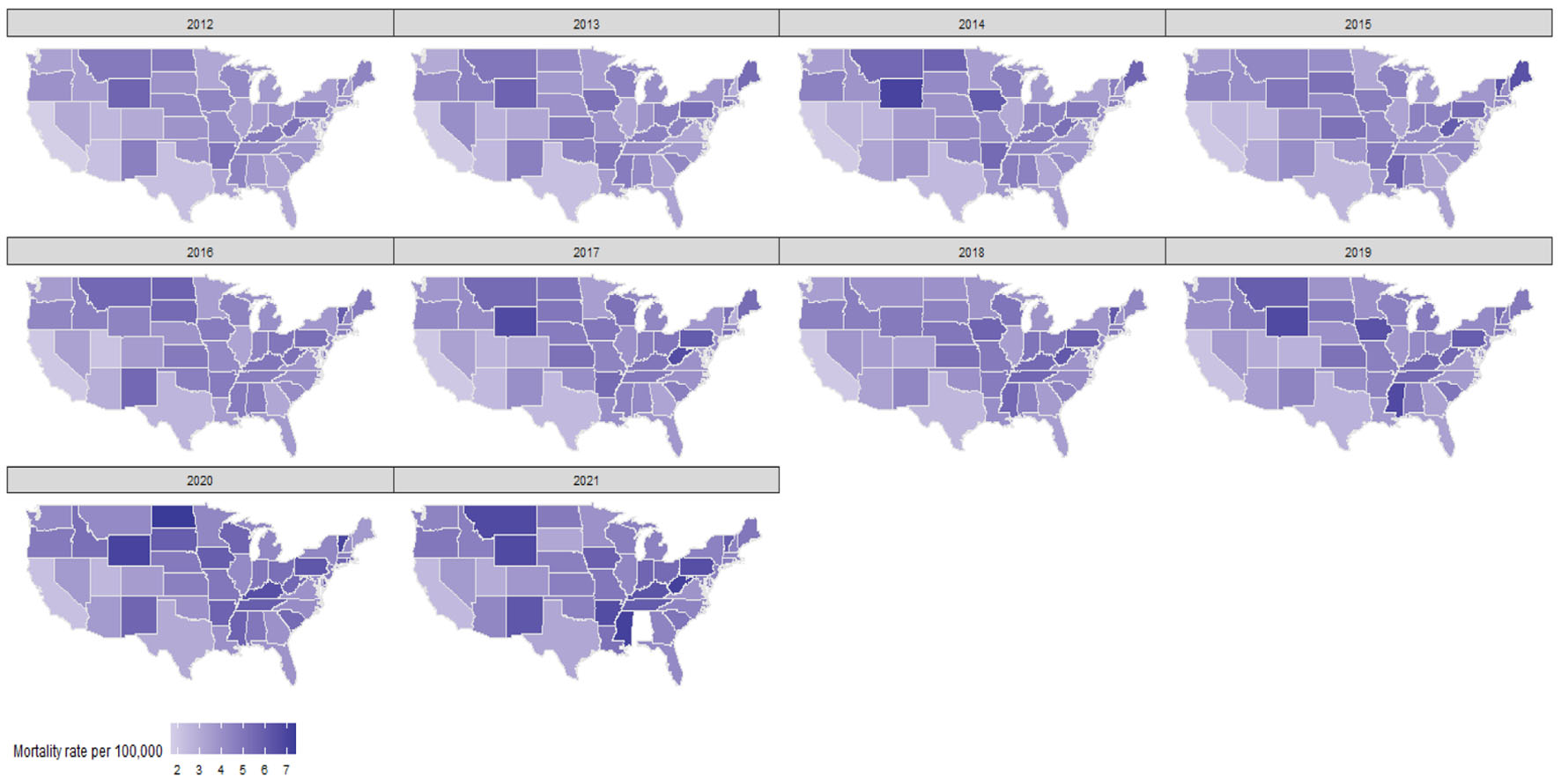 Click for large image | Figure 2. Geographical trending of the UGIB-related mortality before and during the COVID-19 pandemic, 2012 to 2021. UGIB: upper gastrointestinal bleeding; COVID-19: coronavirus disease 2019. |
| Discussion | ▴Top |
The influence of COVID-19 infection on the mortality rates of UGIB has been a topic of significant interest and research. This study provides valuable insights into the impact of COVID-19 infection on UGIB incidence and mortality rates. We found that the mortality rate increased from 3.3 per 100,000 to 4.3 per 100,000 among the population between 2012 and 2021. We also noticed that the mortality rate increased with aging and the male gender.
We reviewed the literature for similar trending studies of UGIB, where Vora et al evaluated the incidence of mortality and case fatality rates through a 30-year mortality trends analysis in Finland. They included 39,054 participants, and 494 (1.3%) suffered from UGIB. The age-standardized incidence of UGIB was 0.94 per 1,000 participants. Similar to our results, the incidence of UGIB and mortality was higher in males than in females. The reported UGIB-related mortality was (0.07 per 1,000 person-years) and the case fatality was 7 per 100 persons with (95% confidence interval: 4.7 - 10.1). Finally, they concluded that the case fatality was stable through the 30-year analysis. However, it was higher in males than females by about 5-10% [24].
Peiro Moreno et al studied the changes in the sales of nonsteroidal anti-inflammatory drugs (NSAIDs) and the trends of UGIB in Valencia from 2000 to 2005 [25, 26]. They found that an increase in NSAIDs use in this period was associated with an increase in the incidence of UGIB. However, it did not affect UGIB hospitalization rates [27, 28]. On the other hand, the findings of our study and other recently published population-based studies demonstrated an increase in hospitalization and mortality related to UGIB [29, 30]. Mohammed et al performed a trend analysis of UGIB in the last 15 years. They reported an increase in the UGIB hospitalization rates from 4.90% in 2006 to 7.63% in 2020. They also suggested that the rise in the use of anti-inflammatory drugs, steroids, and anti-coagulants, as well as an aging population is the main contributing factor to this increase in the incidence of UGIB [31].
Several factors may contribute to the increased mortality rates observed in the study. COVID-19 infection can lead to significant respiratory complications, which may result in systemic inflammation and coagulation abnormalities. These factors may increase the risk of bleeding and subsequent mortality in patients with UGIB. Furthermore, the COVID-19 pandemic may have interrupted healthcare systems, resulting in delayed or inadequate care for patients with UGIB [32, 33].
Multiple determinants could contribute to the geographical variations in UGIB mortality rates and certain states’ increase in 2021, like Montana, Wyoming, West Virginia, and Mississippi. These factors include population age, lifestyle, socioeconomic status, and environmental factors. Overall, the reasons for higher UGIB mortality rates in these states are likely multifactorial and may require a combination of a closer look and public health interventions to address. Other factors influence this study’s outcome, including the pandemic’s duration and severity, accessibility to healthcare services, and changes in patient behavior. The findings reveal an increase in mortality rates among the population between 2012 and 2021, suggesting a possible influence of COVID-19 infection on the incidence and mortality of UGIB.
This analysis may provide valuable insights into the impact of the COVID-19 pandemic on UGIB mortality rates in the United States. By analyzing data from the CDC WONDER database, the study sheds light on the significant increase in mortality rates associated with this condition during the pandemic. These findings indicated that the mortality rates were considerably higher during the pandemic than pre-pandemic levels. Researchers attributed this alarming trend to various factors, including limited access to healthcare services, delayed diagnosis and treatment, and the overarching strain on healthcare systems. Additionally, this study highlighted the need for targeted interventions and public health measures to mitigate the increased risks faced by individuals with this condition, emphasizing the importance of timely medical care and continued monitoring even amidst the global crisis.
Overall, this study represents a significant addition to our understanding of the medical and public health implications of the COVID-19 pandemic and underscores the importance of ongoing research and data analysis to guide effective interventions and policy decisions.
This study has several strengths. To our knowledge, the current study is the most comprehensive analysis of the national mortality trends based on gender, age group, and region using unadjusted and adjusted estimates for UGIB as the underlying cause of death.
This analysis has multiple limitations. One of the limitations is the reliance on data from death certificates, which can contain inaccuracies and may not always provide a complete picture of the patient’s medical history.
Also, the analysis used death certificates not always listing the other risk factors contributing to mortality. Another area for improvement is that we could have stratified data by race or ethnicity. Although it was avoided to lower the suppressed data and erroneous estimates. The association between race or ethnicity and UGIB mortality has already been reported in earlier studies. Additionally, the study only looked at mortality rates and did not analyze the incidence of UGIB, which could provide a more comprehensive understanding of the issue. Furthermore, the study’s focus on the COVID-19 era limits the generalizability of the findings to other periods. Finally, the study did not examine the impact of specific risk factors on UGIB, such as medication use or underlying medical conditions.
Finally, these data may not be representative of the entire population or may not capture changes over time or differences across subgroups, which can limit the generalizability of the study findings. Finally, the CDC WONDER database only provides information on mortality rather than on morbidity or other outcomes of interest, which may limit the scope of the study.
In conclusion, the study shows interestingly, the overall mortality increased in 2020 and 2021, which may highlight the effect of COVID-19 infection on the incidence and mortality of UGIB. These results provide essential insights into the impact of COVID-19 infection on UGIB incidence and mortality rates. The study highlights the need for ongoing research to understand the underlying mechanisms better and inform clinical decision-making in the context of the COVID-19 pandemic.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
As the CDC WONDER database lacks patient and hospital identifiers, informed consent was not required for this study.
Author Contributions
Conceptualization: Nooraldin Merza, Ahmed Taher Masoud, Dushyant Singh Dahiya, Zohaib Ahmed, Ali Nawras, and Abdallah Kobeissy. Data curation: Nooraldin Merza. Formal analysis: Nooraldin Merza. Project administration: Nooraldin Merza and Ahmed Taher Masoud. Resources: Dushyant Singh Dahiya and Zohaib Ahmed. Software: Nooraldin Merza. Supervision: Nooraldin Merza, Abdallah Kobeissy, Ali Nawras. Visualization: Nooraldin Merza, and Dushyant Singh Dahiya. Investigation, methodology, validation, writing-original draft, writing-review and editing: all authors.
Data Availability
WONDER is an online system that makes the CDC resources available to public health professionals and the public. The system provides access to a wide array of public health information. CDC WONDER furthers CDC’s mission of health promotion and disease prevention by speeding up and simplifying access to public health information. CDC WONDER is valuable in public health research, decision-making, priority setting, program evaluation, and resource allocation. The CDC wonder is publicly available at https://wonder.cdc.gov/wonder/help/faq.html#1.
Abbreviations
CDC WONDER: Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research; NVSS: National Vital Statistics System; UGIB: upper gastrointestinal bleeding
| References | ▴Top |
- van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22(2):209-224.
doi pubmed - Rockall TA, Logan RF, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ. 1995;311(6999):222-226.
doi pubmed pmc - Sostres C, Lanas A. Epidemiology and demographics of upper gastrointestinal bleeding: prevalence, incidence, and mortality. Gastrointest Endosc Clin N Am. 2011;21(4):567-581.
doi pubmed - Ting KH, Shiu BH, Yang SF, Liao PL, Huang JY, Chen YY, Yeh CB. Risk of mortality among patients with gastrointestinal bleeding with early and late treatment with tranexamic acid: a population-based cohort study. J Clin Med. 2022;11(6):1741.
doi pubmed pmc - Sehested TSG, Carlson N, Hansen PW, Gerds TA, Charlot MG, Torp-Pedersen C, Kober L, et al. Reduced risk of gastrointestinal bleeding associated with proton pump inhibitor therapy in patients treated with dual antiplatelet therapy after myocardial infarction. Eur Heart J. 2019;40(24):1963-1970.
doi pubmed - Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157-160.
doi pubmed pmc - WHO Director-General’s opening remarks at the media briefing on COVID-19. March 11, 2020.
- Zhu N, Wang W, Liu Z, Liang C, Wang W, Ye F, Huang B, et al. Morphogenesis and cytopathic effect of SARS-CoV-2 infection in human airway epithelial cells. Nat Commun. 2020;11(1):3910.
doi pubmed pmc - Tang Y, Liu J, Zhang D, Xu Z, Ji J, Wen C. Cytokine storm in COVID-19: the current evidence and treatment strategies. Front Immunol. 2020;11:1708.
doi pubmed pmc - Kumar S, Ramos C, Garcia-Carrasquillo RJ, Green PH, Lebwohl B. Incidence and risk factors for gastrointestinal bleeding among patients admitted to medical intensive care units. Frontline Gastroenterol. 2017;8(3):167-173.
doi pubmed pmc - Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, Fang Z, Gu Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69(6):997-1001.
doi pubmed pmc - Kohansal Vajari M, Shirin M, Pourbagheri-Sigaroodi A, Akbari ME, Abolghasemi H, Bashash D. COVID-19-related coagulopathy: A review of pathophysiology and pharmaceutical management. Cell Biol Int. 2021;45(9):1832-1850.
doi pubmed pmc - Jenner WJ, Kanji R, Mirsadraee S, Gue YX, Price S, Prasad S, Gorog DA. Thrombotic complications in 2928 patients with COVID-19 treated in intensive care: a systematic review. J Thromb Thrombolysis. 2021;51(3):595-607.
doi pubmed pmc - Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in Hospitalized Patients with COVID-19. N Engl J Med. 2021;384(8):693-704.
doi pubmed pmc - Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, the Northwell C-RC, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059.
doi pubmed pmc - Mauro A, De Grazia F, Lenti MV, Penagini R, Frego R, Ardizzone S, Savarino E, et al. Upper gastrointestinal bleeding in COVID-19 inpatients: Incidence and management in a multicenter experience from Northern Italy. Clin Res Hepatol Gastroenterol. 2021;45(3):101521.
doi pubmed pmc - Makker J, Mantri N, Patel HK, Abbas H, Baiomi A, Sun H, Choi Y, et al. The Incidence and Mortality Impact of Gastrointestinal Bleeding in Hospitalized COVID-19 Patients. Clin Exp Gastroenterol. 2021;14:405-411.
doi pubmed pmc - Trindade AJ, Izard S, Coppa K, Hirsch JS, Lee C, Satapathy SK, Northwell C-RC. Gastrointestinal bleeding in hospitalized COVID-19 patients: a propensity score matched cohort study. J Intern Med. 2021;289(6):887-894.
doi pubmed - Kwei-Nsoro R, Ojemolon P, Laswi H, Ebhohon E, Ufeh AO, Nieto A, Mir WA, et al. Effect of the COVID-19 pandemic on the epidemiological trends and outcomes of gastrointestinal bleeding: a nationwide study. Proc (Bayl Univ Med Cent). 2023;36(2):145-150.
doi pubmed pmc - von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499.
doi pubmed - Centers for Disease Control and Prevention. General help for CDC WONDER. 2013. Available from: http://wonder.cdc.gov/wonder/help/main.html.
- Centers for Disease Control and Prevention. CDC WONDER (Wide-Ranging Online Data for Epidemiologic Research) Database. 2022. Available from: https://wonder.cdc.gov/.
- Murphy SL, Xu J, Kochanek KD, Arias E, Tejada-Vera B. Deaths: final data for 2018. Natl Vital Stat Rep. 2021;69(13):1-83.
pubmed - Vora P, Pietila A, Peltonen M, Brobert G, Salomaa V. Thirty-year incidence and mortality trends in upper and lower gastrointestinal bleeding in Finland. JAMA Netw Open. 2020;3(10):e2020172.
doi pubmed pmc - Peiro Moreno S, Cervera-Casino P, Sanfelix-Gimeno G, Librero Lopez J. Trends in gastrointestinal bleeding in the Region of Valencia (2000-2005). Relationship to sales of nonsteroidal anti-inflammatory drugs and acid suppression medication. Farm Hosp. 2011;35(6):289-297.
doi pubmed - Aljarad Z, Mobayed BB. The mortality rate among patients with acute upper GI bleeding (with/without EGD) at Aleppo University Hospital: A retrospective study. Ann Med Surg (Lond). 2021;71:102958.
doi pubmed pmc - Laine L, Yang H, Chang SC, Datto C. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am J Gastroenterol. 2012;107(8):1190-1195.
doi pubmed - Lanas A, Garcia-Rodriguez LA, Polo-Tomas M, Ponce M, Alonso-Abreu I, Perez-Aisa MA, Perez-Gisbert J, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104(7):1633-1641.
doi pubmed - Taefi A, Cho WK, Nouraie M. Decreasing trend of upper gastrointestinal bleeding mortality risk over three decades. Dig Dis Sci. 2013;58(10):2940-2948.
doi pubmed - Abougergi MS, Travis AC, Saltzman JR. The in-hospital mortality rate for upper GI hemorrhage has decreased over 2 decades in the United States: a nationwide analysis. Gastrointest Endosc. 2015;81(4):882-888.e881.
doi pubmed - Mohammed A, Trujillo S, Ghoneim S, Paranji N, Waghray N. Small bowel adenocarcinoma: a nationwide population-based study. J Gastrointest Cancer. 2023;54(1):67-72.
doi pubmed - Iqbal U, Patel PD, Pluskota CA, Berger AL, Khara HS, Confer BD. Outcomes of acute gastrointestinal bleeding in patients with COVID-19: a case-control study. Gastroenterology Res. 2022;15(1):13-18.
doi pubmed pmc - Negro A, Villa G, Rolandi S, Lucchini A, Bambi S. Gastrointestinal bleeding in COVID-19 patients: a rapid review. Gastroenterol Nurs. 2022;45(4):267-275.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


