| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 4, August 2022, pages 207-216
Trends of Alcohol Withdrawal Delirium in the Last Decade: Analysis of the Nationwide Inpatient Sample
Hisham Laswia, c, Bashar Attara, Robert Kweia, Pius Ojemolona, Ebehiwele Ebhohonb, Hafeez Shakaa
aInternal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, USA
bInternal Medicine, Lincoln Medical Center, Bronx, NY, USA
cCorresponding Author: Hisham Laswi, Internal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, USA
Manuscript submitted June 12, 2022, accepted July 18, 2055, published online August 23, 2022
Short title: Alcohol Withdrawal Trends
doi: https://doi.org/10.14740/gr1550
| Abstract | ▴Top |
Background: Alcohol use disorder, high-risk drinking, and emergency visits for acute and chronic complications of alcohol use have been increasing in the USA recently. Approximately half of patients with alcohol use disorder experience alcohol withdrawal when they reduce or stop drinking. Though alcohol withdrawal is usually mild, 20% of patients experience more severe manifestations such as hallucinations, seizures, and delirium. In this study, we utilized the Nationwide Inpatient Sample to examine the trends of alcohol withdrawal delirium (AWD) in the period 2010 - 2019.
Methods: This was a retrospective longitudinal trends study involving hospitalizations with AWD in the USA from 2010 to 2019. We searched the databases for hospitalizations using the International Classification of Diseases (ICD) codes (291.0 and F10231). We involved all hospitalizations complicated by AWD and hospitalizations with AWD as the principal diagnosis for admission. We excluded hospitalizations involving patients under the age of 18. We calculated the crude admission rate and the incidence of AWD per million adult hospitalizations during each calendar year. In addition, we analyzed trends of inpatient mortality, length of stay (LOS), and total hospital charges (THC).
Results: The incidence of AWD per million hospitalizations increased from 2,671.8 in 2010 to 3,405.6 in 2019, with an annual percentage change (APC) of 3.1% (P < 0.001). Similarly, AWD admission rate per million hospitalizations increased from 1,030.3 in 2010 to 1,556.0 in 2019, with an average APC of 5.0% (P < 0.001). There were statistically significant trends of increasing inpatient mortality, THC, and LOS over the studied period. In general, female gender, younger age, and Black race were associated with better clinical outcomes.
Conclusions: Our study showed an increase in the incidence and admission rates of AWD. Mortality, LOS, and THC increased over the studied period. Younger age, female gender, and Black race were associated with better clinical outcomes.
Keywords: Alcohol withdrawal delirium; Alcohol; Withdrawal; Trends; Nationwide Inpatient Sample
| Introduction | ▴Top |
The lifetime prevalence of alcohol use disorder is estimated to be 29.1% in community-based samples in the USA [1]. In the period 2001 to 2013, there was a noticeable increase in alcohol use disorder and high-risk drinking in the USA [2]. The total per capita consumption of alcohol is expected to increase in the regions of the Americas until 2025 [3].
Alcohol is the third most common modifiable cause of death in the USA after tobacco and poor diet/physical inactivity [4]. It causes approximately 3.8% of all deaths worldwide and accounts for 4.6% of the global burden of disease [5]. The effects of alcohol consumption on mortality are greater than those of diabetes, hypertension, human immunodeficiency virus (HIV), tuberculosis, and violence [3]. Alcohol use results in a significant financial burden on the healthcare system. In 2014, the aggregate costs for all hospitalizations with alcohol-related diagnosis were $30 billion [6].
This study aimed to describe the epidemiologic trends of alcohol withdrawal delirium (AWD) over the last decade using the Nationwide Inpatient Sample (NIS). In addition, we analyzed the demographics and outcomes of these hospitalizations including inpatient mortality, length of stay (LOS), and total hospital charges (THC).
| Materials and Methods | ▴Top |
Design and data source
This was a retrospective longitudinal trends study involving hospitalizations with AWD in the USA from 2010 to 2019. We sourced data from the NIS databases from 2010 to 2019. The NIS is developed by the Healthcare Cost and Utilization Project (HCUP), a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ). The NIS is a database of inpatient stays derived from billing data submitted by hospitals to statewide data organizations across the USA, covering more than 97% of the US population [7]. The provided dataset for a given calendar year approximates a 20% stratified sample of discharges from US community hospitals, excluding rehabilitation and long-term acute care hospitals. This dataset is weighted to obtain US national estimates [8]. Databases before 2016 were coded using the International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System (ICD-9-CM/PCS). Databases from 2016 were coded using the International Classification of Diseases, 10th Revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS). The 2015 NIS has both ICD-9 and 10 codes; hence, requiring a combination of both versions of ICD codes to obtain the studied cohort in accordance with HCUP regulations and methods [9]. In this study, we weighted the 9 months of ICD-9 data in 2015 for the entire year. In the NIS, diagnoses are divided into two separate categories: principal diagnosis and secondary diagnoses. A principal diagnosis was the ICD code that coded for the primary reason for admission. Secondary diagnoses were any ICD code other than the principal diagnosis.
Study population and variables
We searched NIS databases from 2010 to 2019 for this study. The study involved two cohorts of hospitalizations: 1) all hospitalizations complicated by AWD; 2) all hospitalization with AWD as the principal diagnosis for admission. We searched the databases for hospitalizations using ICD codes (291.0 and F10231). We excluded hospitalizations involving patients under the age of 18. The NIS includes variables on patient demographics, including age, sex, race, median household income (MHOI) for patient’s zip code (income quartiles referred to patients as 1: low income; 2: middle income; 3: upper middle income; and 4: high income), and primary payer. We assessed the comorbidity burden using Sundararajan’s adaptation of the modified Deyo’s Charlson comorbidity index (CCI). This modification maps the 17 Charlson comorbidities into ICD-10 codes. The CCI was grouped into four groups in increasing risk for mortality. It has been adapted to population-based research. A score of > 3 has about a 25% 10-year mortality, while a score of 2 or 1 has a 10% and 4% 10-year mortality, respectively. These cut-off points were chosen to assess the risk of mortality [10].
Outcome measures
We highlighted the biodemographic trends over time for AWD hospitalizations. Specifically, we calculated the crude admission rate and the incidence of AWD per million adult hospitalizations during each calendar year. We analyzed trends of mortality, mean LOS, and mean THC over the studied period.
Statistical analysis
We used Stata® Version 16 software (StataCorp, TX, USA) and Joinpoint Regression Program, Version 4.9.1.0 for data analysis. We analyzed and reported the weighted sample following HCUP regulations for using the NIS database. We grouped age in three categories: 18 - 39 years representing young adults, 40 - 64 years representing middle-aged adults, and ≥ 65 years representing elderly. The incidence of AWD among hospitalizations was calculated following the HCUP methodology for disease incidence and prevalence [11]. The crude admission rate was calculated by dividing total hospitalizations with AWD as the principal diagnosis by the total adult hospitalizations for each calendar year and expressed per million hospitalizations. The incidence of AWD per million adult hospitalizations was obtained by dividing the total hospitalizations complicated by AWD by the total number of adult hospitalizations. This was also expressed per million adult hospitalizations. We used multivariable regression analysis to calculate the incidence and admission rates adjusted for age categories, sex, and race using predictive margins. We subsequently used Joinpoint regression analysis to obtain the trends in rates over the study duration, using the adjusted rates and standard errors. Joinpoint regression analysis has been widely used and validated by the National Institute of Health (NIH) National Cancer Institute to model non-linear trends in cancer rates over a given period [12]. This has been adopted in prior HCUP database research [13, 14]. We used multivariable regression trend analysis to obtain trends in mortality, LOS, and THC adjusted for age categories, sex, and race. The study had a threshold of P < 0.05 for statistical significance.
Ethical considerations
The NIS database lacks patient and hospital level identifiers. Therefore, this study did not require Cook County Health Institutional Review Board approval or informed consents. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
A total of 944,162 hospitalizations complicated by AWD were included in our study. The incidence of AWD per million hospitalizations increased from 2,671.8 in 2010 to 3,405.6 in 2019 (Table 1, Fig. 1), with an annual percentage change (APC) of 3.1% (P < 0.001).
 Click to view | Table 1. Demographics of All Hospitalizations Complicated by Alcohol Withdrawal Delirium (AWD) |
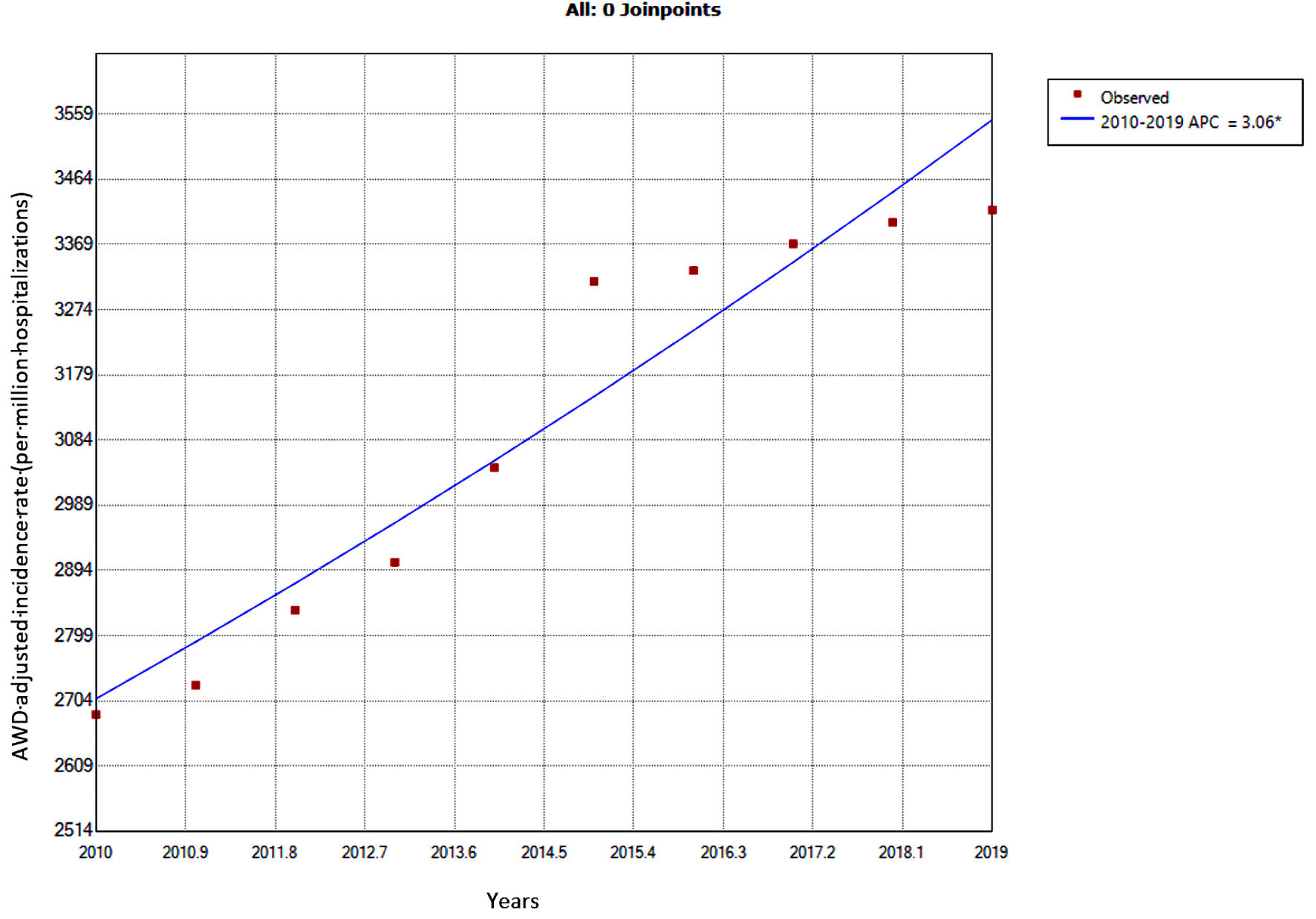 Click for large image | Figure 1. Trends in the adjusted incidence of alcohol withdrawal delirium among all hospitalizations from 2010 to 2019. *Statistically significant. APC = 3.1%, CI: 2.2 - 4.0, P < 0.001. APC: annual percentage change; AWD: alcohol withdrawal delirium. |
Analysis of the outcomes of all hospitalizations complicated by AWD showed a statistically significant trend of increasing inpatient mortality (odds ratio (OR): 1.01, P trend = 0.044) (Table 2). Multivariate analysis showed that hospitalizations for middle aged and elderly patients were associated with higher mortality rates compared to young adults (OR: 2.54 and 5.44, respectively, P < 0.001). Females had lower odds of mortality when compared to males (OR: 0.87, P = 0.001). Hospitalizations for Blacks were associated with lower odds of mortality compared to Whites (OR: 0.81, P < 0.001).
 Click to view | Table 2. Outcomes of All Hospitalizations Complicated by Alcohol Withdrawal Delirium |
There was a statistically significant trend of increasing THC over the studied years (P trend < 0.001) (Table 2). Multivariate analysis showed that hospitalizations for middle aged and elderly patients were associated with higher THC compared to young adults (P < 0.001). Females had lower THC compared to males (P < 0.001). Hospitalizations for Blacks were associated with lower THC compared to Whites; however, this finding did not reach statistical significance (P = 0.114).
LOS increased over the studied period; this trend was statistically significant (P trend = 0.006) (Table 2). Hospitalizations for middle aged adults and elderly patients were associated with longer LOS compared to young adults (P < 0.001). Female gender was associated with shorter LOS (P < 0.001). Hospitalizations for Blacks were associated with longer LOS compared to Whites (P < 0.001).
We included 398,838 hospitalizations with primary diagnosis of AWD (Table 3, Fig. 2). AWD admission rate per million hospitalizations increased from 1,030.3 in 2010 to 1,556.0 in 2019. The APC was 3.3% in the period 2010 - 2012 (P = 0.271), 9.8% in the period 2012 - 2015 (P = 0.016), and 2.2% in the period 2015 - 2019 (P = 0.041). The average APC (AAPC) for the period 2010 - 2019 was 5.0% (P < 0.001).
 Click to view | Table 3. Demographics of Hospitalizations With Alcohol Withdrawal Delirium (AWD) as the Principal Diagnosis |
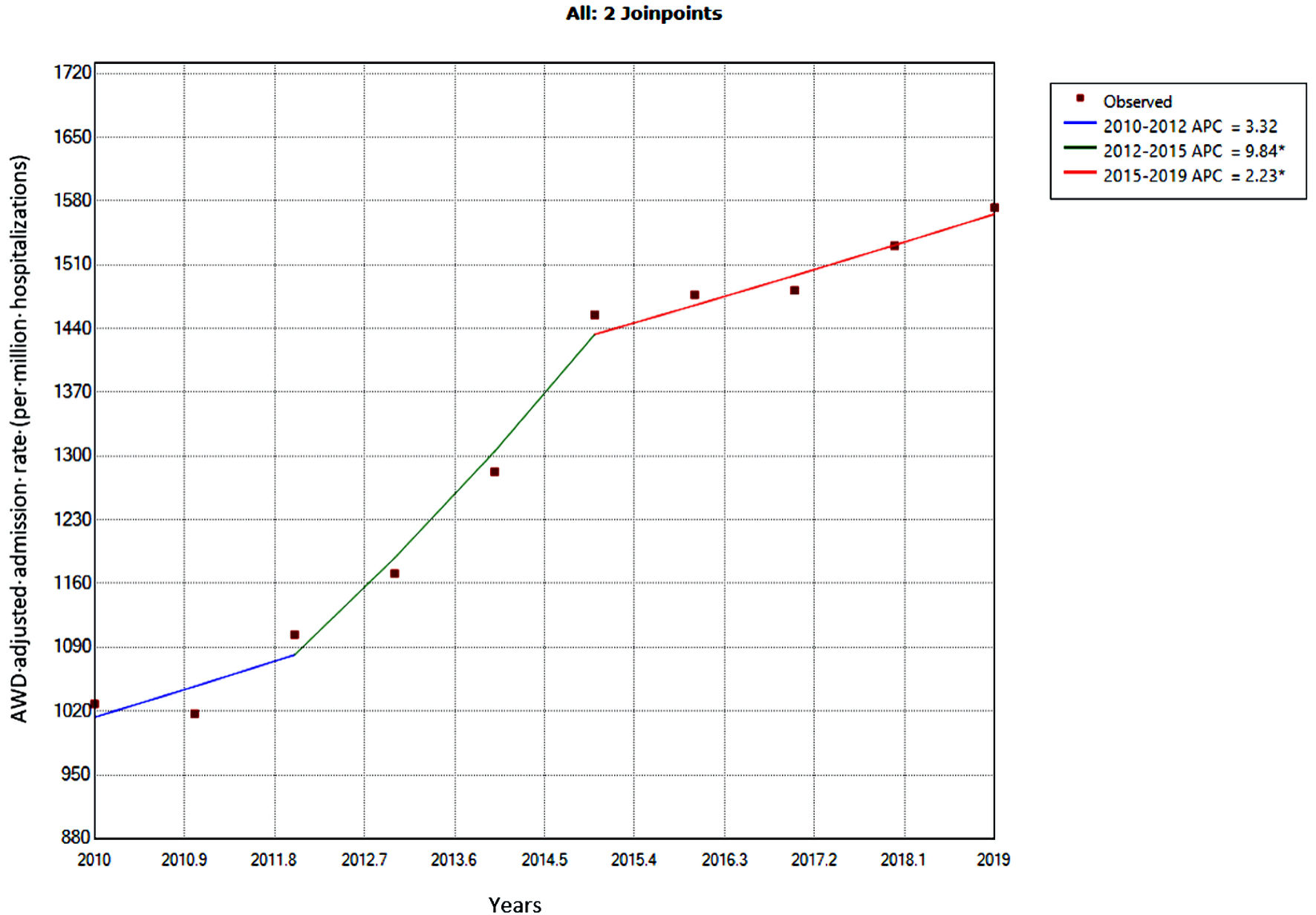 Click for large image | Figure 2. Trends in adjusted alcohol withdrawal delirium admission rate from 2010 to 2019. *Statistically significant. (2010 - 2012) APC = 3.3%, CI: 5.9 - 13.4, P = 0.271; (2012 - 2015) APC = 9.8%, CI: 4.3 - 15.7, P = 0.016; (2015 - 2019) APC = 2.2%, CI: 0.2 - 4.3, P = 0.041; (2010 - 2019) average APC = 5.0%, CI: 3.6 - 6.3, P < 0.001. APC: annual percentage change; AWD: alcohol withdrawal delirium; CI: CI: confidence interval. |
As shown in Table 4, there was no statistically significant trend for inpatient mortality over the studied period (P trend = 0.797). Multivariate analysis showed that hospitalizations for middle aged and elderly patients were associated with higher mortality rates when compared to young adults (OR: 3.26 and 11.27, respectively, P < 0.001). Females had lower odds of morality when compared to males (OR: 0.60, P = 0.001). Hospitalizations for Blacks were associated with lower odds of mortality compared to Whites; however, this finding was not statistically significant (P = 0.683).
 Click to view | Table 4. Outcomes of Hospitalizations With Alcohol Withdrawal Delirium as the Principal Diagnosis |
There was a statistically significant trend of increasing THC over the studied years (P trend < 0.001) (Table 4). Multivariate analysis showed that hospitalizations for middle aged and elderly patients were associated with higher THC compared to young adults (P < 0.001). Hospitalizations for Blacks were associated with lower THC compared to Whites; however, this finding did not reach statistical significance (P = 0.473).
LOS of stay increased over the studied period; this trend was statistically significant (P < 0.001) (Table 4). Hospitalizations for middle aged adults and elderly patients were associated with longer LOS compared to young adults (P < 0.001). Female gender was associated with shorter LOS compared to males (P < 0.001). Hospitalizations for Black patients had longer LOS compared to Whites (P = 0.034).
| Discussion | ▴Top |
In the period 2000 to 2016, the percentage of drinkers in the world has decreased by almost 5%. However, since the world’s population has increased, the decrease in the prevalence of drinking did not translate into fewer current drinkers [3]. In the period 2006 to 2014, the number of acute and chronic alcohol-related emergency department (ED) visits increased significantly [15]. Furthermore, between 2001 - 2002 and 2012 - 2013, 12-month alcohol use, high-risk drinking, and alcohol use disorder increased significantly. The increase in these outcomes were greatest among women, older adults, and racial/ethnic minorities [2].
The incidence and the admission rates of AWD increased significantly over the studied period. There was also a trend of worsening clinical outcomes (inpatient mortality, LOS, and THC) in our analysis. Dose-response relationships could be quantified for all alcohol-related disease categories, with the relative risk increasing with increased level of alcohol consumption for most diseases [16]. It has been found that the likelihood of experiencing withdrawal symptoms increased with increasing alcohol consumption [17]. These trends likely reflect the changes in alcohol consumption observed in the last two decades.
Our analysis showed that middle aged adults and elderly patients had higher mortality rates, LOS, and THC when compared to young adults. Alcohol consumption has been increasing in the elderly population particularly in women [18]. In addition, there has been a recent increase in binge drinking in this population [19]. Evidence suggests that elderly have higher mortality from alcoholic liver disease compared to younger patients [20-23]. Liskow et al found that elderly patients had more severe withdrawal and required higher doses of benzodiazepines [24]. Wonjar et al found the elderly patients had longer hospital stays for AWD and more electrolytes abnormalities compared to younger patients [25]. Similarly, Brower et al found that elderly patients had more withdrawal symptoms for longer duration [26]. The etiology of the worse outcomes in this population is multifactorial. Elderly patients with alcohol use disorder have higher rates of respiratory, endocrine, cardiovascular and central nervous system (CNS) diseases, and dementia compared to young patients [27]. In addition, older patients are at higher risk for cognitive and functional impairment during withdrawal [28]. Older adults have increased sensitivity to benzodiazepines and decreased metabolism of long-acting agents. Benzodiazepines are associated with increased risk of delirium and cognitive impairment in older adults [29]. Furthermore, many older adults drink alcohol and take medications that may interact with alcohol. Some of these interactions are due to age-related changes in the absorption, distribution, and metabolism of alcohol and medications [30]. Exacerbation of therapeutic and adverse effects of medications when combined with alcohol likely contributes to the observed outcomes in our study. Admissions for substance use including cocaine/crack, marijuana/hashish, heroin, non-prescription methadone, and other opiates have increased in the elderly population in the last decade [31, 32].
Our study showed that females had better clinical outcomes in terms of inpatient mortality, LOS, and THC when compared to males, a finding that is consistent with the available evidence [33, 34]. It has been found that withdrawal seizures were significantly more frequent among men than among women [35]. Canales et al found that men with AWD had higher rates of sepsis and longer LOS compared to women [36]. Benedict et al found that male gender was associated with 2.6-fold increase in the risk of benzodiazepine resistant withdrawal [37]. Drinking patterns differ between males and females. According to the global status report on alcohol and health, females are less often current drinkers than males and they drink less on average and engage less often in heavy episodic drinking [3]. Women prefer mild types of alcoholic beverages such as wine and beer [38-40]. They become intoxicated less frequently and are less likely to abandon personal control while drinking [41]. On the other hand, women tend to present with more severe liver disease, particularly alcoholic hepatitis, and do so after a shorter period of excessive drinking and at a lower daily alcohol intake [42, 43]. They also have higher mortality from alcoholic liver cirrhosis compared to men [44]. Interestingly, Goodson et al found that the presence of liver disease was not predictive of alcohol withdrawal [45].
Glutamate-N-methyl-D-aspartic acid (NMDA), γ-aminobutyric acid (GABA), and many other receptors are involved in the adaptive changes in the brain during chronic ethanol exposure [46]. Evidence from animal studies suggests the alcohol induces gender-selective adaptations at the molecular level. It has been found that alcohol-dependent females did not show the same alterations in gene expression for GABA or NMDA receptors as did alcohol-dependent males [47]. Female rats recover more quickly from withdrawal than male rats, even with a greater volume per weight alcohol intake [48, 49]. Differences at the hormonal level also play a role; Devaud et al suggested that the differences between men and women in AWD may be mediated by allopregnanolone [50], an endogenous GABA receptor ligand with anxiolytic and anticonvulsant properties [51].
Our analysis showed that hospitalizations for Blacks were associated with lower mortality and THC, however, they had longer LOS. Caetano et al found that the prevalence of withdrawal symptoms was generally lower among Blacks than among Whites and Hispanics [17]. It has been found that Caucasian race was 3.6 times more likely to be develop benzodiazepine resistant withdrawal [37]. Chan et al found that White patients have twice the odds of having severe alcohol withdrawal when compared to non-White patients, and Black patients have smaller odds of having severe alcohol withdrawal when compared to non-Black patients [52].
The prevalence of alcohol abuse is greater among Whites than among Blacks [53]. In addition, Naimi et al and Herd et al found that Blacks consistently had the lowest rates of binge drinking episodes compared to other ethnicities [54, 55]. Evidence suggests a racial variation in the toxic effects of alcohol. Stewart et al found that Black non-Hispanic and Mexican Americans were more likely to have a 2-fold elevation in aspartate aminotransferase levels when compared with White non-Hispanic Americans [56].
The reason for the longer LOS observed in Blacks is unclear. It has been found that Black patients were more likely to be cocaine dependent than alcohol dependent and were more likely to experience cocaine withdrawal symptoms rather than alcohol withdrawal symptoms [17]. Whether withdrawal from other drugs have led to the observed higher LOS in this population needs further investigations. The lower mortality rate in this population might also contribute to the observed longer LOS.
Our study showed an increase in the incidence and the admission rates for AWD in the period 2010 to 2019. Mortality, LOS, and THC increased over the studied period. Younger age, female gender, and Black race were associated with better clinical outcomes. Our study has some important limitations. The NIS reports information on hospitalizations rather than individual patients, as a result, one patient can be included more than once in the analysis. The severity of AWD could not be determined from the NIS. We could not determine what proportion of patients were managed in the intensive care setting (which may impact outcomes). Therapeutic interventions, medications given, laboratory results, and imaging are not provided in NIS. Finally, the study used ICD codes; therefore, the database may contain errors related to miscoding.
Acknowledgments
We would like to thank the Gastroenterology and Hepatology Department at John H. Stroger, Jr. Hospital of Cook County for the tremendous support and help in completing this project.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Dr. Attar supervised the entire project including the design and the analysis. Dr. Laswi and Dr. Shaka designed the study, performed data analysis, and reviewed the final manuscript. Dr. Kwei, Dr. Ojemolon, and Dr. Ebhohon wrote the manuscript in consultation with Dr. Laswi.
Data Availability
The NIS is a large publicly available inpatient database in the United States, containing data on more than 7 million hospital stays per year. Its large sample size is ideal for developing national and regional estimates and enables analyses of rare conditions, uncommon treatments, and special populations. The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
AAPC: average annual percentage change; AHRQ: Agency for Healthcare Research and Quality; APC: Annual percentage change; AWD: alcohol withdrawal delirium; CCI: Charlson comorbidity index; CI: confidence interval; CNS: central nervous system; GABA: γ-aminobutyric acid; HCUP: Healthcare Cost and Utilization Project; HIV: human immunodeficiency virus; ICD: International Classification of Diseases; ICD-10-CM/PCS: International Classification of Diseases10th Revision, Clinical Modification/Procedure Coding System; ICD-9-CM/PCS: International Classification of DiseasesNinth Revision, Clinical Modification/Procedure Coding System; LOS: length of stay; MHOI: median household income; NIS: Nationwide Inpatient Sample; NMDA: N-methyl-D-aspartic acid; OR: odds ratio; SD: standard deviation; THC: total hospital charges
| References | ▴Top |
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, et al. Epidemiology of DSM-5 alcohol use disorder: results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry. 2015;72(8):757-766.
doi pubmed - Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017;74(9):911-923.
doi pubmed - Global Status Report on Alcohol and Health 2018. https://www.who.int/publications/i/item/9789241565639.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238-1245.
doi pubmed - Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223-2233.
doi - Trends in alcohol-related morbidity among community hospital discharges, United States, 2000-2014. https://pubs.niaaa.nih.gov/publications/surveillance106/hds14.pdf.
- Healthcare Cost and Utilization Project. Introduction to the HCUP National Inpatient Sample (NIS). The National (Nationwide) Inpatient Sample Database Documentation. Available at: hcup-us.ahrq.gov/db/nation/nis/nis_introduction_2018.jsp.
- Nationwide Inpatient Sample (NIS) Redesign Final Report. 2014. HCUP Methods Series Report # 2014-04 ONLINE. U.S. Agency for healthcare research and quality. Available: hcup-us.ahrq.gov/reports/methods/methods.jsp.
- Healthcare Cost and Utilization Project (HCUP) recommendations for reporting trends using ICD-9-CM and ICD-10-CM/PCS data. Online. Revised July 5, 2017. U.S. Agency for healthcare research and quality. Available: hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp.
- Sundararajan V, Quan H, Halfon P, Fushimi K, Luthi JC, Burnand B, Ghali WA. International Methodology Consortium for Coded Health Information (IMECCHI). Cross-National Comparative Performance of Three Versions of the ICD-10 Charlson Index. Med Care. 2007;45:1210.
doi pubmed - Population denominator data sources and data for use with the HCUP databases (Updated with 2019 Population Data) 2020 HCUP methods series report # 2020-02 Online. U.S. Agency for healthcare research and quality. Available: https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp, (unpublished).
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351.
doi - Ikedionwu CA, Dongarwar D, Williams C, Odeh E, Peh MPN, Hooker H, Wiseman S, et al. Trends and risk factors for leishmaniasis among reproductive aged women in the United States. Int J MCH AIDS. 2021;10(2):166-173.
doi pubmed - Zoorob RJ, Salemi JL, Mejia de Grubb MC, Modak S, Levine RS. A nationwide study of breast cancer, depression, and multimorbidity among hospitalized women and men in the United States. Breast Cancer Res Treat. 2019;174(1):237-248.
doi pubmed - White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: results from the nationwide emergency department sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352-359.
doi pubmed - Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, Parry CD, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105(5):817-843.
doi pubmed - Caetano R, Clark CL, Greenfield TK. Prevalence, trends, and incidence of alcohol withdrawal symptoms: analysis of general population and clinical samples. Alcohol Health Res World. 1998;22(1):73-79.
- Breslow RA, Castle IP, Chen CM, Graubard BI. Trends in alcohol consumption among older Americans: national health interview surveys, 1997 to 2014. Alcohol Clin Exp Res. 2017;41(5):976-986.
doi pubmed - Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, Hartz S, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939-1950.
doi pubmed - Potter JF, James OF. Clinical features and prognosis of alcoholic liver disease in respect of advancing age. Gerontology. 1987;33(6):380-387.
doi pubmed - Woodhouse KW, James OF. Alcoholic liver disease in the elderly: presentation and outcome. Age Ageing. 1985;14(2):113-118.
doi pubmed - Laswi H, Abusalim AR, Warraich MS, Khoshbin K, Shaka H. Trends and outcomes of alcoholic liver cirrhosis hospitalizations in the last two decades: analysis of the nationwide inpatient sample. Gastroenterology Res. 2022;15(2):91-99.
doi pubmed - Yoon YH, Chen CM, Slater ME, Jung MK, White AM. Trends in premature deaths from alcoholic liver disease in the U.S., 1999-2018. Am J Prev Med. 2020;59(4):469-480.
doi pubmed - Liskow BI, Rinck C, Campbell J, DeSouza C. Alcohol withdrawal in the elderly. J Stud Alcohol. 1989;50(5):414-421.
doi pubmed - Wojnar M, Wasilewski D, Zmigrodzka I, Grobel I. Age-related differences in the course of alcohol withdrawal in hospitalized patients. Alcohol Alcohol. 2001;36(6):577-583.
doi pubmed - Brower KJ, Mudd S, Blow FC, Young JP, Hill EM. Severity and treatment of alcohol withdrawal in elderly versus younger patients. Alcohol Clin Exp Res. 1994;18(1):196-201.
doi pubmed - Shahpesandy H, Pristasova J, Janikova Z, Mojzisova R, Kasanicka V, Supalova O. Alcoholism in the elderly: a study of elderly alcoholics compared with healthy elderly and young alcoholics. Neuro Endocrinol Lett. 2006;27(5):651-657.
- Kraemer KL, Mayo-Smith MF, Calkins DR. Impact of age on the severity, course, and complications of alcohol withdrawal. Arch Intern Med. 1997;157(19):2234-2241.
doi pubmed - By the American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227-2246.
doi pubmed - Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. Am J Geriatr Pharmacother. 2007;5(1):64-74.
doi pubmed - Wang YP, Andrade LH. Epidemiology of alcohol and drug use in the elderly. Curr Opin Psychiatry. 2013;26(4):343-348.
doi pubmed - Chhatre S, Cook R, Mallik E, Jayadevappa R. Trends in substance use admissions among older adults. BMC Health Serv Res. 2017;17(1):584.
doi pubmed - Schuckit MA, Tipp JE, Reich T, Hesselbrock VM, Bucholz KK. The histories of withdrawal convulsions and delirium tremens in 1648 alcohol dependent subjects. Addiction. 1995;90(10):1335-1347.
doi pubmed - Deshmukh A, Rosenbloom MJ, Sassoon S, O'Reilly A, Pfefferbaum A, Sullivan EV. Alcoholic men endorse more DSM-IV withdrawal symptoms than alcoholic women matched in drinking history. J Stud Alcohol. 2003;64(3):375-379.
doi pubmed - Wojnar M, Wasilewski D, Matsumoto H, Cedro A. Differences in the course of alcohol withdrawal in women and men: a Polish sample. Alcohol Clin Exp Res. 1997;21(8):1351-1355.
doi pubmed - Canales FJ, Davis J, Girgla N, Emami M, Cooper T, Carlson RW. Alcohol Withdrawal Syndrome in Women vs Men: Analysis of 1496 Cases at a Single Site. Am J Crit Care. 2022;31(3):212-219.
doi pubmed - Benedict NJ, Wong A, Cassidy E, Lohr BR, Pizon AF, Smithburger PL, Falcione BA, et al. Predictors of resistant alcohol withdrawal (RAW): A retrospective case-control study. Drug Alcohol Depend. 2018;192:303-308.
doi pubmed - Christie MM, Bamber D, Powell C, Arrindell T, Pant A. Older adult problem drinkers: who presents for alcohol treatment? Aging Ment Health. 2013;17(1):24-32.
doi pubmed - Minagawa Y. Gender differences in alcohol choice among Russians: evidence from a quantitative study. Eur Addict Res. 2013;19(2):82-88.
doi pubmed - Bobrova N, West R, Malyutina D, Malyutina S, Bobak M. Gender differences in drinking practices in middle aged and older Russians. Alcohol Alcohol. 2010;45(6):573-580.
doi pubmed - Robbins CA, Martin SS. Gender, styles of deviance, and drinking problems. J Health Soc Behav. 1993;34(4):302-321.
doi - Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. 2010;29(4):437-445.
doi pubmed - Saunders JB, Davis M, Williams R. Do women develop alcoholic liver disease more readily than men? Br Med J (Clin Res Ed). 1981;282(6270):1140-1143.
doi pubmed - Kamper-Jorgensen M, Gronbaek M, Tolstrup J, Becker U. Alcohol and cirrhosis: dose—response or threshold effect? J Hepatol. 2004;41(1):25-30.
doi pubmed - Goodson CM, Clark BJ, Douglas IS. Predictors of severe alcohol withdrawal syndrome: a systematic review and meta-analysis. Alcohol Clin Exp Res. 2014;38(10):2664-2677.
doi pubmed - Crews FT, Morrow AL, Criswell H, Breese G. Effects of ethanol on ion channels. Int Rev Neurobiol. 1996;39:283-367.
doi - Devaud LL, Matthews DB, Morrow AL. Gender impacts behavioral and neurochemical adaptations in ethanol-dependent rats. Pharmacol Biochem Behav. 1999;64(4):841-849.
doi - Devaud LL, Alele P, Ritu C. Sex differences in the central nervous system actions of ethanol. Crit Rev Neurobiol. 2003;15(1):41-59.
doi pubmed - Devaud LL, Chadda R. Sex differences in rats in the development of and recovery from ethanol dependence assessed by changes in seizure susceptibility. Alcohol Clin Exp Res. 2001;25(11):1689-1696.
doi - Devaud LL, Risinger FO, Selvage D. Impact of the hormonal milieu on the neurobiology of alcohol dependence and withdrawal. J Gen Psychol. 2006;133(4):337-356.
doi pubmed - Martin-Garcia E, Pallares M. Effects of intrahippocampal nicotine and neurosteroid administration on withdrawal in voluntary and chronic alcohol-drinking rats. Alcohol Clin Exp Res. 2005;29(9):1654-1663.
doi pubmed - Chan GM, Hoffman RS, Gold JA, Whiteman PJ, Goldfrank LR, Nelson LS. Racial variations in the incidence of severe alcohol withdrawal. J Med Toxicol. 2009;5(1):8-14.
doi pubmed - Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004;74(3):223-234.
doi pubmed - Herd D. Predicting drinking problems among black and white men: results from a national survey. J Stud Alcohol. 1994;55(1):61-71.
doi pubmed - Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289(1):70-75.
doi pubmed - Stewart SH. Racial and ethnic differences in alcohol-associated aspartate aminotransferase and gamma-glutamyltransferase elevation. Arch Intern Med. 2002;162(19):2236-2239.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


