| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 4, August 2022, pages 173-179
The Association Between Gastroesophageal Reflux Disease and Non-Small Cell Lung Cancer: A Retrospective Case-Control Study
Shivantha Amarnatha, Adam Starrb, Divya Chukkalorec, e , Ahmed Elfikya, Mohammad Abureesha, Anum Aqsac, Chetan Singhc, Chanudi Weerasinghec, Dhineshreddy Guralaa, Seleshi Demissied, Liliane Deeba, Terenig Terjanianb
aDepartment of Gastroenterology & Hepatology, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, New York, NY, USA
bDivision of Hematology & Medical Oncology, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, New York, NY, USA
cDepartment of Internal Medicine, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, New York, NY, USA
dDepartment of Biostatistics & Epidemiology, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, New York, NY, USA
eCorresponding Author: Divya Chukkalore, Department of Internal Medicine, Zucker School of Medicine at Hofstra/Northwell at Staten Island University Hospital, Staten Island, NY 10305, USA
Manuscript submitted May 11, 2022, accepted June 27, 2022, published online July 12, 2022
Short title: GERD and NSCLC
doi: https://doi.org/10.14740/gr1537
| Abstract | ▴Top |
Background: Lung cancer is a leading cause of mortality in the USA. Non-small cell lung cancer (NSCLC) contributes to 85% of all lung cancers. It is the most prevalent subtype amongst non-smokers, and its incidence has risen in the last 20 years. In addition, gastroesophageal reflux disease (GERD) has been associated with several lung pathologies, namely idiopathic pulmonary fibrosis and asthma. We aimed to investigate the association between GERD and NSCLC by performing a retrospective, multicenter, case-control study. This is the first study of this nature to be carried out in the USA.
Methods: Data were retrieved from 17 Northwell health care facilities in the New York area between the years 2010 and 2018. Inclusion criteria were patients > 18 years of age with NSCLC (large cell, adenocarcinoma, and squamous cell). They were appropriately matched with controls based on age, gender, weight, comorbidities, and medication use. Our exposure group had a diagnosis of GERD based on the International Classification of Diseases, Ninth/10th Revision (ICD 9/10) codes and endoscopic, in addition to histological evidence if present. We excluded patients with secondary lung cancers, esophageal adenocarcinoma, other primary malignancies, Barrett’s esophagus, and smokers. Logistic regression was conducted to determine the adjusted odds ratio (OR) and corresponding 95% confidence interval (CI) for the association between NSCLC and GERD.
Results: A total of 1,083 subjects were included in our study: 543 (50%) patients were diagnosed with NSCLC. In this population, GERD was twice as prevalent compared to controls (20.4% vs. 11.6%, P < 0.001). Multivariate analysis demonstrated that GERD was associated with a higher risk of NSCLC compared to matched controls (OR = 1.86, 95% CI = 1.26 - 2.73). In addition, GERD patients treated with either antihistamines or proton pump inhibitors did not demonstrate an overall reduced risk of NSCLC (OR = 1.01, 95% CI = 0.48 - 2.12).
Conclusions: Our study demonstrates that GERD is associated with a higher risk of NSCLC, irrespective of GERD treatment. We postulate that GERD patients suffer from chronic micro-aspirations leading to a prolonged inflammatory state within the lung parenchyma, triggering specific proliferative signaling pathways that may lead to malignant transformation.
Keywords: Gastroesophageal reflux disease; Non-small cell lung cancer; Micro-aspiration; Risk factors
| Introduction | ▴Top |
Lung cancer is diagnosed in more than 200,000 people annually and remains one of the leading causes of cancer deaths in the United States [1]. Furthermore, lung cancer remains the leading cause of cancer-related death in the United States and worldwide. In 2020, it was responsible for an estimated 136,000 deaths in the United States alone [1]. This number had decreased since its peak in 2005 when nearly 160,000 individuals died from cancer-related outcomes [2]. The improvement is primarily attributed to increased awareness of the risks of smoking and smoking cessation programs. However, although smoking is believed to cause the majority of lung cancer, according to the American Cancer Society, as many as 20% of people in the United States who died from lung cancer in 2020 (a total of roughly 30,000 people) never smoked [3]. Given the impact of this disease, surprisingly little information is available on the descriptive epidemiology of lung cancer in never smokers.
Lung cancers can be divided into small cell (small cell lung cancer (SCLC)) and non-small cell (non-small cell lung cancer (NSCLC)) types. NSCLC contributes to about 85% of all lung cancer, and this category can be further divided into squamous and non-squamous subtypes (adenocarcinoma and large cell carcinoma) [4]. While both SCLC and NSCLC types are highly associated with smoking, almost all never smokers have NSCLC. These patients generally have the non-squamous sub-type, specifically adenocarcinoma [5].
Although overall rates of NSCLC are decreasing, there has been no improvement in the incidence rate of lung cancer among never smokers [6]. Environmental factors are the most significant contributor to lung cancer in never smokers, with secondhand smoke exposure believed to cause about 25% of the cases in this group [7]. Radon is also thought to be a significant carcinogen in those exposed, and pollution, asbestos, and arsenic have been implicated [8]. Family members of never smokers with lung cancer are also at higher risk of developing NSCLC, suggesting there are hereditary factors. Epidermal growth factor receptor (EGFR) mutations play a crucial role in lung cancer. While these mutations are usually somatic, germline mutations are reported, and the incidence rates of lung cancer in these never smokers are higher than incidence rates in smokers [9]. Although many risk factors are reported, the strength of the correlation is often unclear and may not explain a significant proportion of lung cancers among never smokers.
Gastroesophageal reflux disease (GERD) has been proposed as a new possible risk factor. A population-based cohort study from Taiwan demonstrated that patients with GERD had a 50% increased risk of lung cancer compared to the non-GERD population; however, this study did not exclude smokers [10]. GERD is a known risk factor for the development of esophageal adenocarcinoma, where the chronic reflux of stomach acids into the esophagus causes metaplasia, dysplasia, and eventually carcinoma in the distal esophagus [11]. Chronic micro-aspiration from GERD has also been associated with multiple pulmonary pathologies, including interstitial pulmonary fibrosis (IPF) and asthma [9]. Therefore, it is plausible that if stomach acid is reaching the lung parenchyma from GERD and chronic aspiration, then the same malignant transformation may be occurring in the lungs that occurs in the esophagus. Hence this large case-control study of never smokers was designed to investigate the association between GERD and NSCLC.
| Materials and Methods | ▴Top |
We performed a retrospective, case-control study using data from the 17 Northwell health care facilities in the New York metropolitan area between the years 2010 and 2018. Statistical analysis was carried out using SAS (SAS Institute, NC, USA). Cases were selected using the following inclusion criteria: patients aged 18 years and older with a diagnosis of NSCLC. The patients were initially screened using the International Classification of Diseases, Ninth/10th Revision (ICD 9/10) codes for lung cancer and then confirmed by a chart review to confirm the specific histology. Patients were excluded if the diagnosis was either SCLC or a metastatic lesion to the lung from a non-lung primary. Additionally, those with any history of smoking, Barrett’s esophagus (BE), esophageal adenocarcinoma, or a second primary cancer were excluded based on ICD codes and if noted during the chart review.
It was calculated that a sample size of 1,300 subjects (650 per group) was sufficient to detect a clinically significant difference of 6% between cases and controls in the exposure rate of GERD, using a two-sided Z-test of the difference between proportions with 80% power and a 5% significance level. This 6% difference represents the difference between a 15% prevalence rate in the control group and a 21% rate in the lung cancer group. Univariate and multivariate analyses were then performed to identify an association between GERD and NSCLC among never-smokers. P values < 0.05 were considered to be statistically significant.
A total of 650 cases were selected after the initial screen. After an extensive chart review and data collection based on the criteria stated above, 543 patients remained. The lack of documentation of ICD codes for NSCLC and smoking history were the common causes of exclusion during chart review. The controls were then matched for age, gender, body mass index (BMI), comorbidities, and medication use. Controls had the same exclusion criteria, with the addition of primary lung cancer. The baseline demographics of the patients are shown in Table 1. GERD exposure was identified either by the presence of an ICD 9/10 code, or endoscopy, along with histologic evidence if present.
 Click to view | Table 1. Baseline Demographic Characteristics of Patients With Non-Small Cell Lung Cancer (NSCLC) and Controls |
The study was approved by the institutional review board (IRB) with the number #19-0400. The data extracted and manuscript were reviewed by the Research Department and Ethics Committee. No experimental intervention was performed, and any specification of guidelines, legislations, or permissions were not required. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
From 2010 to 2018, a total of 1,083 subjects were included in our study: 543 (50%) cases were diagnosed with NSCLC, and 542 (50%) controls did not have NSCLC after patients were censored due to missing data. Overall, 805 (74%) were female, and 278 (26%) were male, which was consistent between the cases and controls. Ninety-three percent of the patients had adenocarcinoma, 6% were squamous, and 1% were large cell (Fig. 1). GERD was twice as prevalent compared to the controls (20.4% vs. 11.6%, P < 0.001) (Table 1). Multivariate analysis demonstrated that GERD was associated with a higher risk of NSCLC compared to matched controls (odds ratio (OR) = 1.86, 95% confidence interval (CI) = 1.26 - 2.73) (Table 2). GERD patients treated with either antihistamines or proton pump inhibitors (PPIs) did not demonstrate a reduced risk of NSCLC (OR = 1.01, 95% CI = 0.2 - 1.34) (Fig. 2).
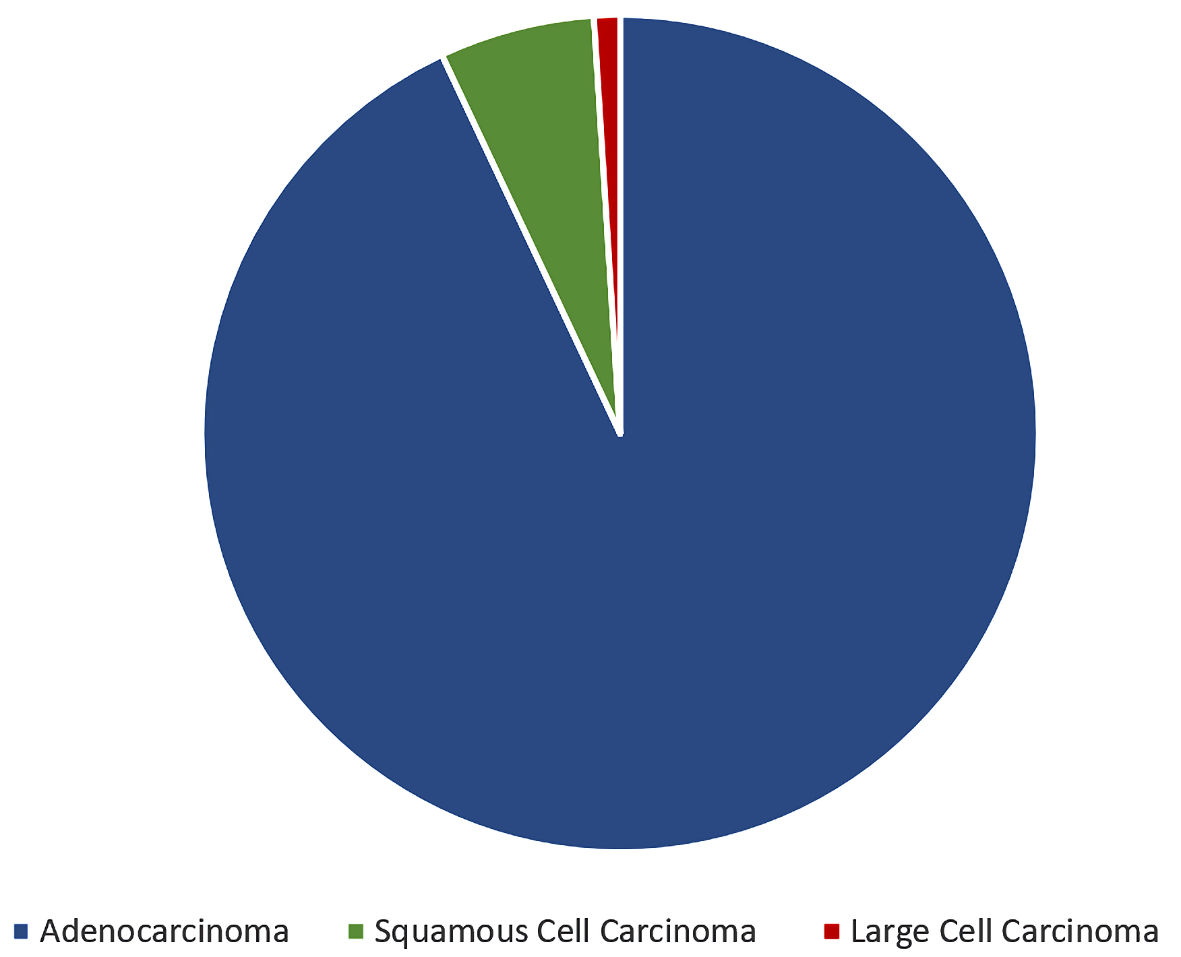 Click for large image | Figure 1. Pie chart depicting histological subtypes amongst 543 patients diagnosed with NSCLC: 93% of the patients had adenocarcinoma, 6% had squamous cell carcinoma and 1% had large cell carcinoma. NSCLC: non-small cell lung cancer. |
 Click to view | Table 2. Multivariate Analysis of Variables Associated Between GERD and NSCLC |
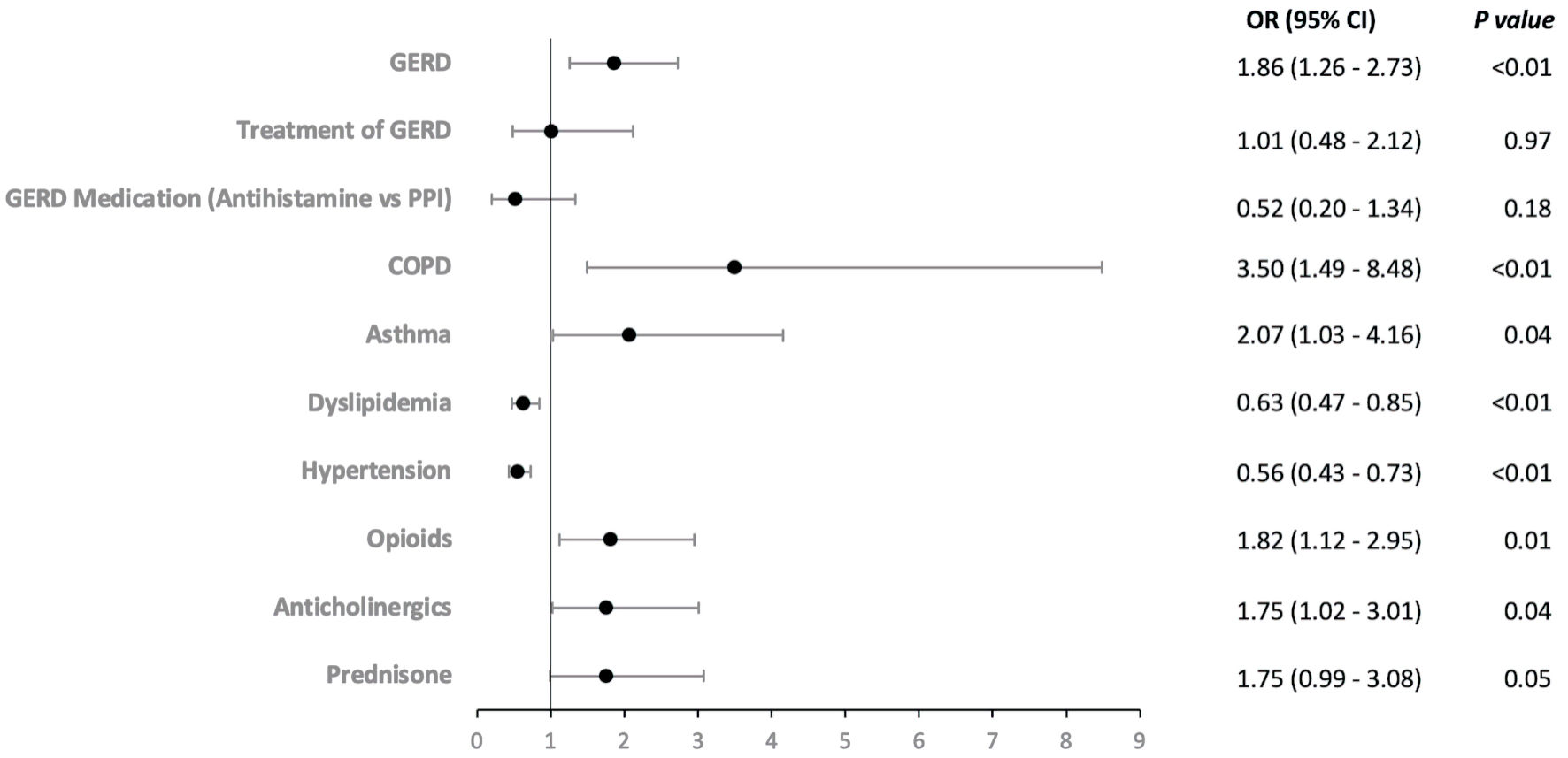 Click for large image | Figure 2. Forest plot of odds ratio (OR) values (x-axis) according to the independent risk predictors (y-axis) of non-small cell lung cancer. COPD: chronic obstructive pulmonary disease; GERD: gastroesophageal reflux disease; PPI: proton pump inhibitors; OR: odds ratio; CI: confidence interval. |
Other variables were also found to be associated with NSCLC (Table 2) such as chronic obstructive pulmonary disease (COPD) having an association with NSCLC. There was a total of 33 patients with COPD in the study; 26 patients (4.3%) in the cases arm and seven patients (1.3%) in the control arm; the adjusted OR was 3.5 (P < 0.01, CI = 1.49 - 8.48). Regarding the family history of lung cancer, 114 (21%) with NSCLC had a family history when compared to 87 (16%) in those without NSCLC (P = 0.023) (Table 1). However, this failed to remain statistically significant in the multivariate analysis (adjusted OR = 0.73, P = 0.06, CI: 0.53 - 1.01) (Table 2).
| Discussion | ▴Top |
This large, case-control study of never smokers was designed to investigate the association between GERD and NSCLC. We found the rate of GERD in patients with NSCLC was twice the rate of GERD in patients without NSCLC, suggesting that GERD is a risk factor for lung cancer in never smokers. This was demonstrated in both the univariate and multivariate analyses, where both comorbidities and medications were accounted for separately.
A retrospective cohort study in Taiwan is one of the only other studies that looked at the estimated risks of lung cancer in patients with GERD [10]. The researchers used its National Health Insurance Research Database and included patients diagnosed endoscopically with GERD [10]. The rate of lung cancer among patients with GERD in this study was 0.0020 per person-years vs. 0.0013 per person-years among patients developing lung cancer without GERD (hazard ratio (HR) = 1.53, 95% CI = 1.19 - 1.98) and had significantly more comorbidities, such as osteoporosis, diabetes mellitus, depression, chronic liver disease and chronic kidney disease [10]. The authors showed that the crude HRs of the potential confounders were non-significant, and Cox regression analysis was performed to control for these factors.
A separate study from Norway investigated if GERD was associated with higher all-cause mortality using a questionnaire of symptoms to determine if patients had severe GERD and compared these patients to those without GERD symptoms. This study was negative; however, it did show a non-statistically significant trend towards increased rates of head and neck and lung cancer among those with GERD [12].
Our study supports the conclusion that GERD is associated with a higher risk of NSCLC, irrespective of GERD treatment. We postulate that GERD patients suffer from chronic micro-aspirations leading to a prolonged inflammatory state within the lung parenchyma, triggering specific proliferative signaling pathways that may lead to malignant transformation. Several mechanisms can help explain this significant relationship between GERD and lung cancer from various studies. One study has shown gastric reflux that reaches into the upper airway causing cellular damage in the epithelial lining and introducing chronic inflammation resulting in laryngopharyngeal malignant transformation [13]. Another study demonstrated reflux material such as hydrochloric acid, pepsin, bile, bile acids and trypsin inducing cellular proliferation, apoptosis and DNA damage all promoting carcinogenesis of the larynx and pharynx [14]. These pathogeneses may occur in the lower respiratory tract resulting in chronic inflammation thus contributing to the development of NSCLC.
In our study by excluding smokers, we were able to achieve two goals. First, it allowed us to explore a new risk factor for never smokers with lung cancer, and it removed the most significant confounder present in the study from Taiwan [10]. Second, we excluded all patients with BE and any other primary lung tumor to minimize any confounding factors.
Additionally, we individually reviewed all the charts for any mention of smoking to improve the fidelity of the data, as ICD codes for smoking are often missing in many electronic medical records (EMRs). Similarly, charts were manually reviewed for the pathology of the lung cancer to ensure all cases were NSCLC. As these were done after the initial data collection, these patients were excluded to minimize confounding factors and not replaced, so our total number of patients is below the initial target. Despite being underpowered, GERD was still statistically significantly associated with lung cancer.
The exclusion of patients with BE may have underestimated the association. We excluded these patients to help minimize the effects of any confounding factors that could have had a high impact on the study. Nevertheless, those with BE are likely the patients with the most significant GERD. Therefore, if the proposed mechanism is correct, patients with BE will probably have micro-aspiration into the lungs and develop NSCLC. Therefore, by excluding these patients, we likely excluded the population most likely to have both GERD and NSCLC. If they were included, the association might have been even more robust.
While the focus of this paper was to determine the association between GERD and lung cancer in never smokers, GERD should be further looked at in smokers as well. Smoking is known to cause GERD, so there is likely a higher percentage of smokers with GERD [15]. There may be an additive effect or even synergistic effect of having these two insults, smoking and acid exposure, which might even further raise the risk in smokers. Therefore, this should be evaluated in future studies as well.
There were several limitations of this study. GERD exposure was identified either by the presence of an ICD 9/10 code, or endoscopy, along with histologic evidence if present. The initial protocol called for all ICD diagnoses to be confirmed with further testing, such as esophagogastroduodenoscopy (EGD) reports, pathology reports, or pH monitoring. However, there was an insufficient number of patients with complete documentation, and censoring these patients would have biased results, so all patients with an ICD diagnosis of GERD were included in the final analysis. Also, with symptoms of GERD often being nonspecific definitive diagnosis usually requires invasive testing such as 24-h pH monitoring or EGD with biopsy. In addition, patients are often empirically treated with PPIs or histamine H2-receptor blockers (H2 blockers) and never go for further testing if they respond well to treatment. Many people are diagnosed with the GERD who may not have the condition. We tried to confirm the ICD diagnoses with histologic evidence and pH monitoring by chart review in which most patients either did not have invasive testing performed, or we lacked access to this information. Although, many of these patients diagnosed with GERD that may not have had significant reflux were included in the study. This could also underestimate the effect size if the association was proven correct suggesting an even stronger link than the study showed. Performing a cohort study and starting with patients with confirmed GERD by invasive testing would solve this problem. However, this would require an extensive database to include enough never smokers with NSCLC and confirmed GERD. Another limitation was the method by which never smoker status was determined. Since all patients without a smoking history listed in the EMR were included, it likely allowed many patients who were smokers but with inaccurate documentation in their chart to be included. One way we corrected for this was to perform a separate analysis excluding those patients with documented COPD, assuming these patients likely represented patients who were smokers but without it recorded in the chart.
Large, multifaceted public health efforts have contributed to the decline in overall lung cancer mortality. Per the Centers for Disease Control and Prevention (CDC), mass media campaigns have decreased smoking rates by 5.0% in adults and increasing taxes and expanding smoke-free zones have further lowered smoking rates and lung cancer rates [16]. Additionally, lung cancer screening efforts have also made an impact. The US Preventive Services Task Force (USPSTF) has recently expanded the eligible population increasing the age span to 50 - 80 from 55 - 80 and decreasing the minimum pack years required from 30 to 20. The initial National Cancer Screening Trial, which changed the screening standard from chest X-ray to low-dose computerized tomography (CT) scan, showed a 9.8% decrease in all-cause mortality [17]. While this is a significant improvement, efforts need to be made to help decrease the incidence and mortality of never smokers. Therefore, finding modifiable risk factors is paramount. Our study suggests GERD is one of contributing risk factors leading to NSCLC, and efforts to treat GERD can potentially reduce the risk of developing NSCLC.
Learning points
Question: Is there an association between GERD and the development of NSCLC?
Findings: In this retrospective case-control study, 1,083 subjects were included, in which 543 (50%) patients were diagnosed with NSCLC. In this population, GERD was twice as prevalent compared to controls (20.4% vs. 11.6%, P < 0.001). Multivariate analysis demonstrated that GERD was associated with a higher risk of NSCLC compared to matched controls (OR = 1.86, 95% CI = 1.26 - 2.73). In addition, GERD patients treated with either antihistamines or PPIs did not demonstrate an overall reduced risk of NSCLC (OR = 1.01, 95% CI = 0.48 - 2.12).
Meaning: There is a positive association between GERD and NSCLC as GERD patients suffer from chronic micro-aspirations.
Acknowledgments
None to declare.
Financial Disclosure
No funding was obtained from any organization or personnel during any stage of manuscript writing or submission.
Conflict of Interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants, or patents received or pending, or royalties.
Informed Consent
The data extracted and manuscript were reviewed with Research Department and Ethics Committee. No experimental intervention was performed, and any specification of guidelines, legislations, or permissions were not required.
Author Contributions
Shivantha Amarnath, BSc, MRSB, MD, conceived the idea, contributed to article draft writing, draft revision, and created and edited figures and tables. Adam Starr, DO, conceived the idea, and contributed to article draft writing, and draft revision. Divya Chukkalore, MD contributed to literature review, article draft writing, draft revision, created and edited figures and tables. Ahmed Elfiky, MD contributed to study design, literature search, literature review, and created tables and figures. Mohammad Abureesh, MD, Anum Aqsa, MD, Chetan Singh, MD, Chanudi Weerasinghe, MD, Dhineshreddy Gurala, MD and Seleshi Demissie DrPH: data collection and analysis. Liliane Deeb, MD and Terenig Terjanian, MD: writing supervision and draft revision.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
doi pubmed - Haddad DN, Sandler KL, Henderson LM, Rivera MP, Aldrich MC. Disparities in lung cancer screening: a review. Ann Am Thorac Soc. 2020;17(4):399-405.
doi pubmed - Siegel DA, Fedewa SA, Henley SJ, Pollack LA, Jemal A. Proportion of never smokers among men and women with lung cancer in 7 US States. JAMA Oncol. 2021;7(2):302-304.
doi pubmed - Smolle E, Pichler M. Non-smoking-associated lung cancer: a distinct entity in terms of tumor biology, patient characteristics and impact of hereditary cancer predisposition. Cancers (Basel). 2019;11(2):204.
doi pubmed - Basumallik N, Agarwal M. Small cell lung cancer. In: StatPearls. Treasure Island (FL), 2022.
- Islami F, Ward EM, Sung H, Cronin KA, Tangka FKL, Sherman RL, Zhao J, et al. Annual report to the nation on the status of cancer, part 1: national cancer statistics. J Natl Cancer Inst. 2021;113(12):1648-1669.
doi pubmed - Vineis P, Hoek G, Krzyzanowski M, Vigna-Taglianti F, Veglia F, Airoldi L, Overvad K, et al. Lung cancers attributable to environmental tobacco smoke and air pollution in non-smokers in different European countries: a prospective study. Environ Health. 2007;6:7.
doi pubmed - Gorlova OY, Weng SF, Zhang Y, Amos CI, Spitz MR. Aggregation of cancer among relatives of never-smoking lung cancer patients. Int J Cancer. 2007;121(1):111-118.
doi pubmed - Yamamoto H, Yatabe Y, Toyooka S. Inherited lung cancer syndromes targeting never smokers. Transl Lung Cancer Res. 2018;7(4):498-504.
doi pubmed - Hsu CK, Lai CC, Wang K, Chen L. Risk of lung cancer in patients with gastro-esophageal reflux disease: a population-based cohort study. PeerJ. 2016;4:e2753.
doi pubmed - Zhang HY, Spechler SJ, Souza RF. Esophageal adenocarcinoma arising in Barrett esophagus. Cancer Lett. 2009;275(2):170-177.
doi pubmed - Ness-Jensen E, Gottlieb-Vedi E, Wahlin K, Lagergren J. All-cause and cancer-specific mortality in GORD in a population-based cohort study (the HUNT study). Gut. 2018;67(2):209-215.
doi pubmed - Langevin SM, Michaud DS, Marsit CJ, Nelson HH, Birnbaum AE, Eliot M, Christensen BC, et al. Gastric reflux is an independent risk factor for laryngopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2013;22(6):1061-1068.
doi pubmed - Li Y, Xu G, Zhou B, Tang Y, Liu X, Wu Y, Wang Y, et al. Effects of acids, pepsin, bile acids, and trypsin on laryngopharyngeal reflux diseases: physiopathology and therapeutic targets. Eur Arch Otorhinolaryngol. 2022;279(6):2743-2752.
doi pubmed - Kahrilas PJ, Gupta RR. Mechanisms of acid reflux associated with cigarette smoking. Gut. 1990;31(1):4-10.
doi pubmed - Wakefield MA, Durkin S, Spittal MJ, Siahpush M, Scollo M, Simpson JA, Chapman S, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98(8):1443-1450.
doi pubmed - Marshall RC, Tiglao SM, Thiel D. Updated USPSTF screening guidelines may reduce lung cancer deaths. J Fam Pract. 2021;70(7):347-349.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


