| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Short Communication
Volume 15, Number 3, June 2022, pages 136-141
Trends of Readmissions for Gastrointestinal Bleeding After Alcoholic Hepatitis: Analysis of the Nationwide Readmission Database
Hisham Laswia, b, Bashar Attara, Abdul-Rahman Abusalima, Katayoun Khoshbina, Hafeez Shakaa
aDepartment of Internal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL 60612, USA
bCorresponding Author: Hisham Laswi, Department of Internal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL 60612, USA
Manuscript submitted April 6, 2022, accepted May 12, 2022, published online June 2, 2022
Short title: Trends of GIB After AH
doi: https://doi.org/10.14740/gr1526
| Abstract | ▴Top |
Background: Alcohol consumption is associated with numerous hepatic manifestations, including alcoholic fatty liver disease, alcoholic hepatitis (AH), and liver cirrhosis. AH is a common and serious complication of alcohol use. Gastrointestinal bleeding (GIB) remains one of the most common causes of death in these patients. In this article, we studied the trends of GIB after AH.
Methods: This was a retrospective interrupted trend study. We analyzed the 2010, 2012, 2014, 2016, and 2018 Nationwide Readmission Databases. The first AH hospitalization in the year was marked as index hospitalization. We identified subsequent hospitalizations with GIB within 30 days and marked them as readmissions. A multivariate regression analysis was used to calculate the risk-adjusted odds of trends for GIB readmissions, including esophageal varices bleeding (EVB), upper GIB, lower GIB, and all GIB.
Results: The volume of index hospitalizations increased from 10,248 in 2010 to 16,479 in 2018. Similarly, all readmissions increased from 1,838 in 2010 to 3,908 in 2018. Of all readmissions, EVB increased from 3.9% in 2010 to 5.9% in 2018 (odds ratio (OR) trend 1.10; P < 0.001). Readmissions for upper GIB increased from 2.4% in 2010 to 7.8% in 2018 (OR trend 1.22; P < 0.001). On the other hand, lower GIB readmissions decreased from 7.2% in 2010 to 4.7% in 2018 (OR trend 0.95; P = 0.015). There was no statistically significant trend for all GIB readmissions (OR trend 1; P = 0.915).
Conclusion: Further studies are needed to evaluate the patterns of lower GIB in patients with liver disease and the recent trends of corticosteroids use in AH patients.
Keywords: Trends; Alcoholic hepatitis; Gastrointestinal bleeding; Readmission
| Introduction | ▴Top |
Alcohol is the third most common modifiable cause of death in the United States after tobacco and poor diet/physical inactivity [1]. Alcoholic hepatitis (AH) is a common and serious complication of alcohol use. In 2007, more than 50,000 patients were hospitalized with AH in the USA [2]. These patients are at increased risk for complications including infections [3], renal failure [4, 5], progression to liver cirrhosis [6], and death [7]. Studies have shown that the overall mortality rate exceeds 30% [7, 8], with gastrointestinal bleeding (GIB) being the second most common cause of death [7]. In this study, we examined the trends of readmissions for GIB after AH hospitalizations.
| Materials and Methods | ▴Top |
This was a retrospective interrupted trend study. We analyzed the Nationwide Readmission Database (NRD) using the International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System (ICD-9-CM/PCS) and the ICD-10-CM/PCS. The NRD is the largest publicly available readmission database drawn from the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SID). The NRD allows a weighted analysis to obtain 100% of the United States admissions within a given year [9]. We included 2010, 2012, 2014, 2016, and 2018 NRD databases. The codes K70.10, K70.11, and 571.1 were used to identify patients with AH. The first hospitalization in the year was marked as index hospitalization. We identified subsequent hospitalizations within 30 days and marked them as readmissions. Individuals < 18 years, elective, and traumatic hospitalizations were excluded. December hospitalizations were also excluded as they did not contain complete data to assess 30-day readmissions. A multivariate regression analysis was used to calculate the risk-adjusted odds of trends for GIB readmissions, including esophageal varices bleeding (EVB), upper GIB (excluding EVB), lower GIB, and all GIB. P-values ≤ 0.05 were considered statistically significant. Data analysis was performed using Stata® Version 16 software (StataCorp, College Station, TX, USA). As the NRD does not include patient-specific or hospital-specific identifiers [9], this study was exempt from the approval of institutional review board (IRB) and ethics committee and did not require subjects’ consent.
| Results | ▴Top |
We observed an increase in the number of index hospitalizations and all readmissions over the studied period. The volume of index hospitalizations increased from 10,248 in 2010 to 16,479 in 2018 (Fig. 1 and Table 1). Similarly, all readmissions increased from 1,838 in 2010 to 3,908 in 2018 (Fig. 1 and Table 1). There were statistically significant trends of increasing readmissions for EVB and upper GIB (Fig. 2 and Table 2). Of all readmissions, EVB increased from 3.9% in 2010 to 5.9% in 2018 (odds ratio (OR) trend 1.10; P < 0.001). Readmissions for upper GIB increased from 2.4% in 2010 to 7.8% in 2018 (OR trend 1.22; P < 0.001). On the other hand, there was a statistically significant trend of decreasing readmissions for lower GIB (Fig. 2 and Table 2). Lower GIB readmissions decreased from 7.2% in 2010 to 4.7% in 2018 (OR trend 0.95; P = 0.015). There was no statistically significant trend for all GIB readmissions (OR trend 1; P = 0.915). Compared to young adults (18 - 44 years), middle aged adults (45 - 64 years) and older adults (65 years and older) had higher mortality when readmitted after AH (OR 2.1; P < 0.001 and OR 2.7; P < 0.001, respectively).
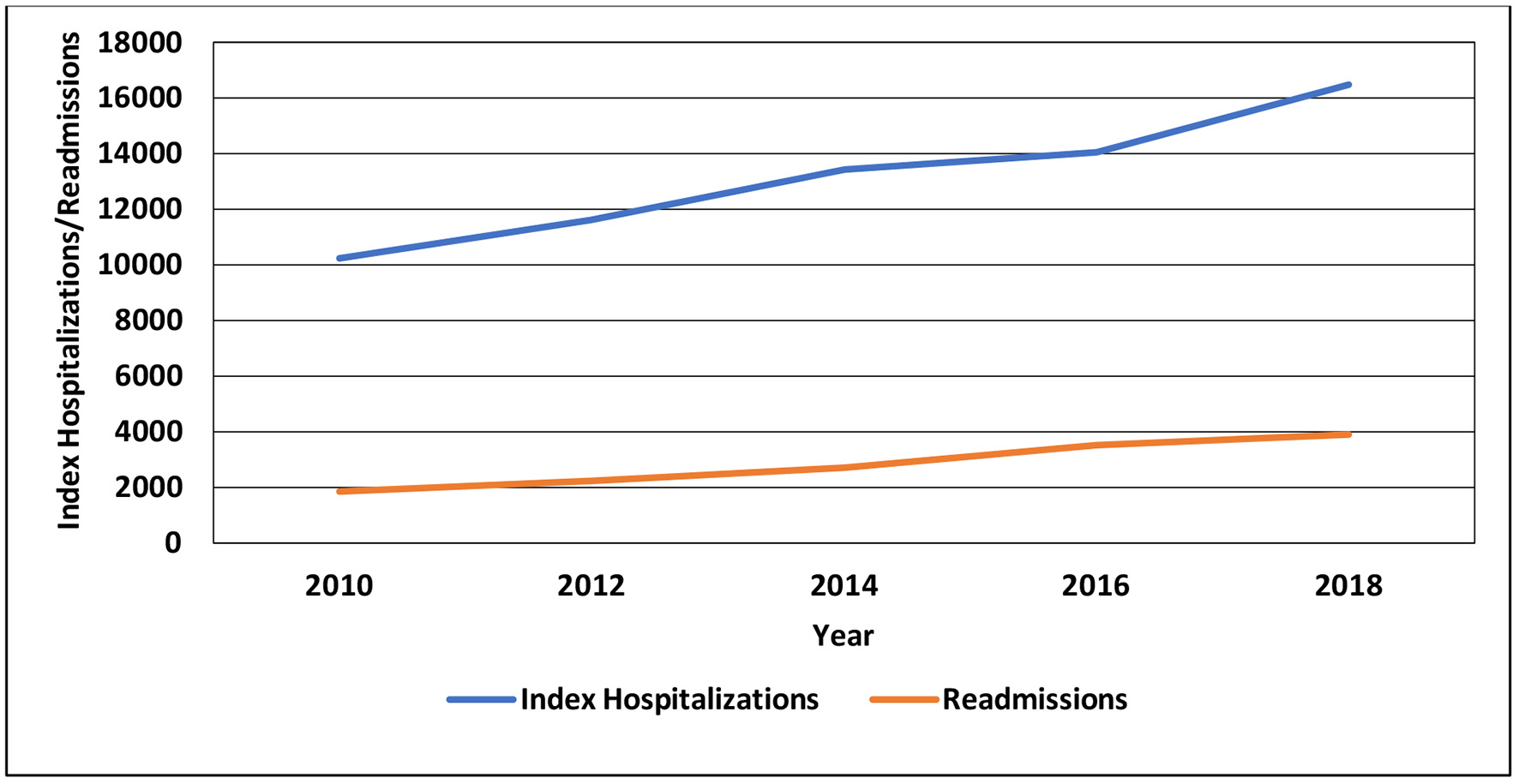 Click for large image | Figure 1. Index hospitalizations for alcoholic hepatitis and all readmissions during 2010 - 2018. |
 Click to view | Table 1. Index Hospitalizations for Alcoholic Hepatitis and All Readmissions During 2010 - 2018 |
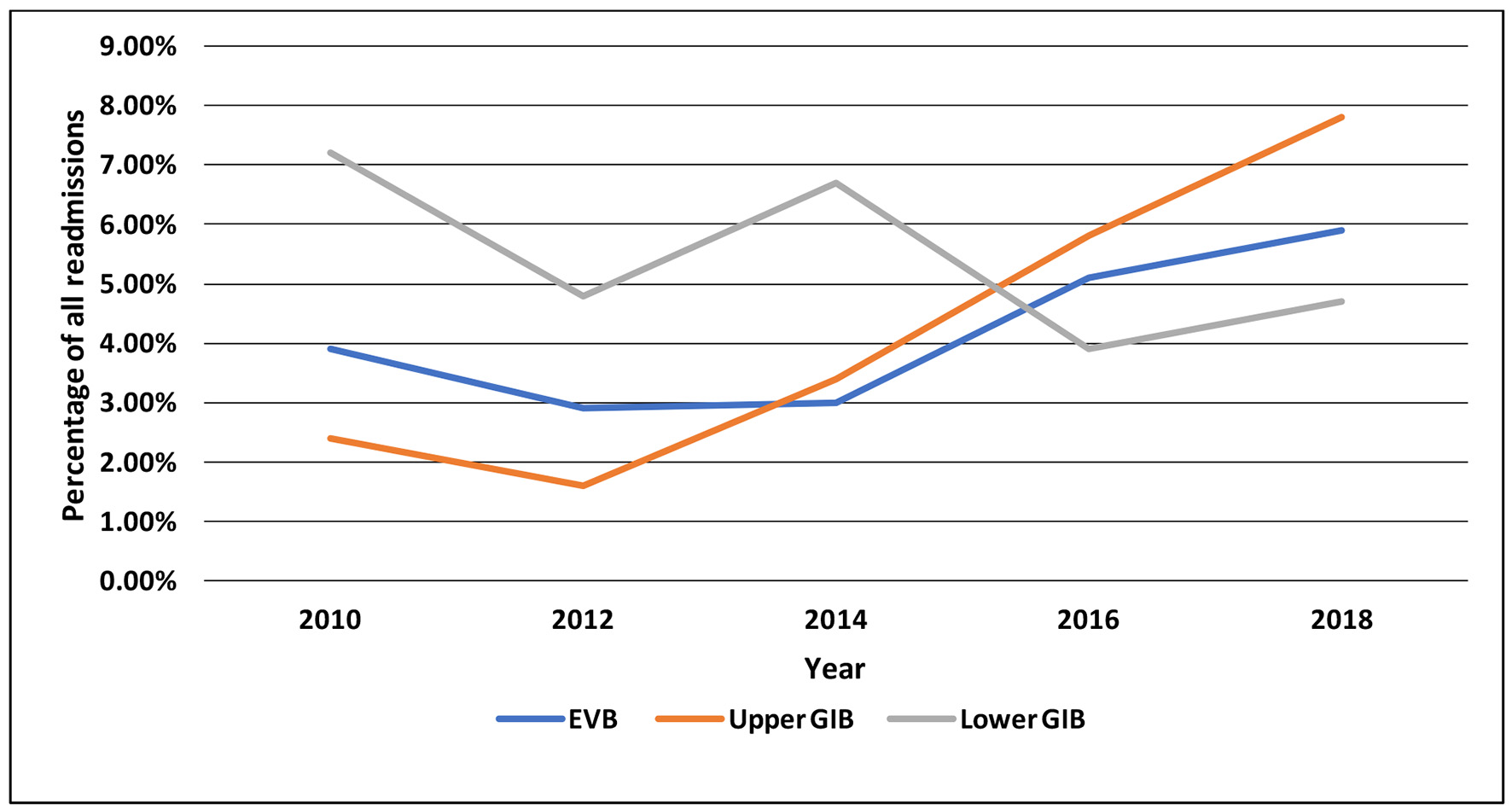 Click for large image | Figure 2. Trends of EVB (P < 0.001) and upper GIB (P < 0.001) and lower GIB (P = 0.015) during 2010 - 2018. GIB: gastrointestinal bleeding; EVB: esophageal varices bleeding. |
 Click to view | Table 2. Trends of EVB, Upper GIB, Lower GIB, and All GIB During 2010 - 2018 |
| Discussion | ▴Top |
Alcohol consumption per capita has increased globally and nationally [10, 11]. Between 2001 - 2002 and 2012 - 2013, high-risk alcohol drinking and alcohol use disorder increased by 29.9% and 49.4%, respectively [12]. Moreover, in the period 2006 - 2014, both acute and chronic alcohol-related emergency visits increased by 51.5% and 75.7%, respectively [13]. These changes might in part account for the increase in the number of index hospitalizations and readmissions over the studied period. Our findings are consistent with the available data from the last two decades [14-16]. We used ICD codes to identify index hospitalizations and readmissions; therefore, coding errors can affect the results. Pang et al found that the positive predictive value of the ICD-10 code used for AH is 67% [17]. This might have resulted in a modest over- or underestimation of the incidence of AH; however, we do not believe that such inaccuracy has produced the observed trends.
Consistent with the available data from AH and cirrhosis patients [18, 19], we observed an increase in the proportion of patients readmitted for EVB over the studied period. Recently, the severity, comorbidities, and complications associated with AH have worsened [6]. Nguyen et al found a recent trend of increasing model for end-stage liver disease (MELD) score in AH patients [6]. The same study also found an increase in the Charlson comorbidity index over the past decade. Higher MELD score has been associated with increased upper GIB [20]. Similarly, Crooks et al found that non-gastrointestinal comorbidities defined using the Charlson comorbidity index was associated with upper GIB [21].
It has been found that in patients with AH, the diagnosis of cirrhosis increased significantly between 2000 (28%) and 2011 (32%) [6]. Recently, hospitalizations and readmissions for liver cirrhosis have been increasing in the USA [22, 23]. Moreover, Fan et al found that during year 2000 - 2014, portal vein thrombosis (PVT) prevalence among alcoholic cirrhosis patients was increasing with an annual percent change of 8.9% [24]. The increases in the prevalence of liver cirrhosis and PVT likely have contributed to the observed increase in EVB. In addition, evidence suggests that patients with cirrhosis and PVT who receive anticoagulant therapy have increased recanalization and reduced progression of thrombosis [25]. The increase in the use of anticoagulants for PVT would also increase the risk of EVB [26]. Obesity is common in AH and associated with a greater than two-fold increase in short-term mortality [27, 28]. Berzigotti et al found that body mass index (BMI) was an independent predictor of decompensation (including EVB) in cirrhotic patients [29]. From 1999 - 2000 through 2017 - 2018, obesity prevalence in the USA increased from 30.5% to 42.4% [30]. It is unclear if this increase has affected the observed EVB trends.
We found a statistically significant trend of increasing readmissions for upper GIB. The etiology of this trend is likely multifactorial and overlapping with EVB. As discussed above, the increase in the prevalence of cirrhosis and PVT likely have resulted in higher rates of portal gastropathy. In addition, we speculate that the recent increase in alcohol consumption has resulted in more alcohol-induced gastritis. Many studies showed improved short-term mortality with steroids use in patients with severe disease [31-33]. The American Association for the Study of Liver Diseases (AASLD) [34], the American Gastroenterological Association (AGA) [35], and the American College of Gastroenterology (ACG) [36] recommend the use of corticosteroids in the treatment of severe AH. The use of steroids is associated with increased risk of GIB [37, 38], with the highest rates occurring within the first month after initiation [38]. Data on the trends of steroids use in AH patients are lacking.
We observed a trend of decreasing lower GIB over the studied period. Studies showed variable results for the trends of lower GIB in the last decade [39-41]. Data on lower GIB in patients with liver disease are very scarce. Khalifa et al found that the most common causes of lower GIB in cirrhotic patients were hemorrhoids followed by portal hypertensive enteropathy or colopathy [42], with 72% of patients with hemorrhoids having either a clinical or radiological evidence of portal hypertension. Similarly, Rabinovitz et al found that esophageal varices were present in most patients with hemorrhoids and that the degree of portal hypertension was associated with the presence of hemorrhoids [43]. On the other hand, a smaller study found no significant difference in the hepatic venous pressure gradient between cirrhotic patients with and without hemorrhoids [44]. The etiology of observed trend is unclear, especially its divergence from EVB trend. Khalifa et al found that 33% of lower GIB patients with cirrhosis had severe bleeding requiring packed red blood cell (PRBC) transfusion and 17% died during hospitalization [42]. In addition, two studies found a trend of increasing lower GIB in elderly patients [40, 45]. Devani et al found that age was an independent predictor of mortality in patients with lower GIB [46]. It is unclear if higher mortality played a role in the observed trend. Further studies are needed to clarify the etiologies of lower GIB in patients with liver disease and their association with portal hypertension.
Conclusion
We noticed trends of increasing readmissions for EVB and upper GIB and a trend of decreasing readmissions for lower GIB. However, there was no statistically significant trend for all GIB over the studied period. The etiology of these trends is likely multifactorial as discussed above. Further studies are needed to evaluate the recent trends of corticosteroids use in AH patients and the patterns of lower GIB in patients with liver disease. Our study has some limitations. Given the use of ICD codes, the database may contain errors related to miscoding. The criteria used to establish the diagnosis of AH cannot be obtained from NRD. In addition, the NRD reports information on hospitalizations rather than individual patients; therefore, patients with many readmissions would be included more than once in the dataset. The NRD does not include any information on laboratory values, medications, nutritional support, or therapeutic interventions. Lastly, we were unable to calculate the MELD, Maddrey’s, or Child-Pugh score from the data available in NRD.
Acknowledgments
We would like to thank the Gastroenterology and Hepatology Department at John H. Stroger Jr. Hospital of Cook County for the tremendous support and help in completing this project.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Dr. Attar supervised the entire project including the design, analysis, and writing the manuscript. Dr. Laswi and Dr. Shaka designed the study, performed data analysis, and reviewed the final manuscript. Dr. Abusalim and Dr. Khoshbin wrote the manuscript in consultation with Dr. Laswi.
Data Availability
The Nationwide Readmission Database is publicly available as stated in the methods. Any inquiries regarding supporting data of this study should be directed to the corresponding author.
Abbreviations
AASLD: American Association for the Study of Liver Diseases; ACG: American College of Gastroenterology; AGA: American Gastroenterological Association; AH: alcoholic hepatitis; AHRQ: Agency for Healthcare Research and Quality; EVB: esophageal varices bleeding; GIB: gastrointestinal bleeding; HCUP: Healthcare Cost and Utilization Project; ICD-10-CM/PCS: International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Coding System; ICD-9-CM/PCS: International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System; IRB: institutional review board; MELD: model for end-stage liver disease; NRD: Nationwide Readmissions Database; OR: odds ratio; PRBC: packed red blood cell; PVT: portal vein thrombosis; SID: State Inpatient Databases
| References | ▴Top |
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238-1245.
doi pubmed - Liangpunsakul S. Clinical characteristics and mortality of hospitalized alcoholic hepatitis patients in the United States. J Clin Gastroenterol. 2011;45(8):714-719.
doi pubmed - Karakike E, Moreno C, Gustot T. Infections in severe alcoholic hepatitis. Ann Gastroenterol. 2017;30(2):152-160.
- Altamirano J, Fagundes C, Dominguez M, Garcia E, Michelena J, Cardenas A, Guevara M, et al. Acute kidney injury is an early predictor of mortality for patients with alcoholic hepatitis. Clin Gastroenterol Hepatol. 2012;10(1):65-71.e63.
doi pubmed - Verma S, Ajudia K, Mendler M, Redeker A. Prevalence of septic events, type 1 hepatorenal syndrome, and mortality in severe alcoholic hepatitis and utility of discriminant function and MELD score in predicting these adverse events. Dig Dis Sci. 2006;51(9):1637-1643.
doi pubmed - Nguyen TA, DeShazo JP, Thacker LR, Puri P, Sanyal AJ. The Worsening Profile of Alcoholic Hepatitis in the United States. Alcohol Clin Exp Res. 2016;40(6):1295-1303.
doi pubmed - Yu CH, Xu CF, Ye H, Li L, Li YM. Early mortality of alcoholic hepatitis: a review of data from placebo-controlled clinical trials. World J Gastroenterol. 2010;16(19):2435-2439.
doi pubmed - Altamirano J, Lopez-Pelayo H, Michelena J, Jones PD, Ortega L, Gines P, Caballeria J, et al. Alcohol abstinence in patients surviving an episode of alcoholic hepatitis: Prediction and impact on long-term survival. Hepatology. 2017;66(6):1842-1853.
doi pubmed - Overview of the Nationwide Readmissions Database (NRD). https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
- Global status report on alcohol and health 2018: https://www.who.int/publications/i/item/9789241565639.
- Apparent per capita alcohol consumption: National, state, and regional trends, 1977-2012. https://pubs.niaaa.nih.gov/publications/surveillance98/cons12.htm.
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017;74(9):911-923.
doi pubmed - White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: results from the nationwide emergency department sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352-359.
doi pubmed - Jinjuvadia R, Liangpunsakul S, Translational R, Evolving Alcoholic Hepatitis Treatment C. Trends in alcoholic hepatitis-related hospitalizations, financial burden, and mortality in the United States. J Clin Gastroenterol. 2015;49(6):506-511.
doi pubmed - Sandahl TD, Jepsen P, Thomsen KL, Vilstrup H. Incidence and mortality of alcoholic hepatitis in Denmark 1999-2008: a nationwide population based cohort study. J Hepatol. 2011;54(4):760-764.
doi pubmed - Dahiya DS, Kichloo A, Singh J, Singh G, Wani F, Shaka H. Declining inpatient mortality despite increasing thirty-day readmissions of alcoholic hepatitis in the United States from 2010 to 2018. Gastroenterology Res. 2021;14(6):334-339.
doi pubmed - Pang JX, Ross E, Borman MA, Zimmer S, Kaplan GG, Heitman SJ, Swain MG, et al. Validation of coding algorithms for the identification of patients hospitalized for alcoholic hepatitis using administrative data. BMC Gastroenterol. 2015;15:116.
doi pubmed - Sempokuya T, Zhang G, Nakagawa K. Temporal trends of cirrhosis associated conditions. World J Hepatol. 2019;11(1):74-85.
doi pubmed - Solanki S, Haq KF, Chakinala RC, Khan Z, Aronow WS, Ali Khan M, Siddiqui MT, et al. Inpatient burden of esophageal varices in the United States: analysis of trends in demographics, cost of care, and outcomes. Ann Transl Med. 2019;7(18):480.
doi pubmed - Rodriguez-Luna HMD; JDAMD; RFCMD. MELD score as a predictor of esophageal varices re-bleeding risk.
- Crooks CJ, West J, Card TR. Comorbidities affect risk of nonvariceal upper gastrointestinal bleeding. Gastroenterology. 2013;144(7):1384-1393.E2.
doi pubmed - Kichloo A, El-Amir Z, Dahiya DS, Wani F, Singh J, Solanki D, Edigin E, et al. Trends of alcoholic liver cirrhosis readmissions from 2010 to 2018: Rates and healthcare burden associated with readmissions. World J Hepatol. 2021;13(12):2128-2136.
doi pubmed - Hirode G, Saab S, Wong RJ. Trends in the burden of chronic liver disease among hospitalized US adults. JAMA Netw Open. 2020;3(4):e201997.
doi pubmed - Fan X, Huang X, Hershman M, Zheng X, Jiang C, Yue B, Weisberg I. Portal vein thrombosis prevalence and mortality among alcoholic cirrhosis in a nationwide inpatient cohort. Eur J Gastroenterol Hepatol. 2020;32(9):1160-1167.
doi pubmed - Loffredo L, Pastori D, Farcomeni A, Violi F. Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis: a systematic review and meta-analysis. Gastroenterology. 2017;153(2):480-487.e481.
doi pubmed - Sasso R, Rockey DC. Anticoagulation therapy in patients with liver cirrhosis is associated with an increased risk of variceal hemorrhage. Am J Med. 2019;132(6):758-766.
doi pubmed - Parker R, Kim SJ, Im GY, Nahas J, Dhesi B, Vergis N, Sinha A, et al. Obesity in acute alcoholic hepatitis increases morbidity and mortality. EBioMedicine. 2019;45:511-518.
doi pubmed - Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25(1):108-111.
doi pubmed - Berzigotti A, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Morillas R, Escorsell A, et al. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology. 2011;54(2):555-561.
doi pubmed - Obesity is a common, serious, and costly disease. https://www.cdc.gov/obesity/data/adult.html#:∼:text=The%20US%20obesity%20prevalence%20was,from%204.7%25%20to%209.2%25.
- Mathurin P, O'Grady J, Carithers RL, Phillips M, Louvet A, Mendenhall CL, Ramond MJ, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60(2):255-260.
doi pubmed - Imperiale TF, McCullough AJ. Do corticosteroids reduce mortality from alcoholic hepatitis? A meta-analysis of the randomized trials. Ann Intern Med. 1990;113(4):299-307.
doi pubmed - Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: glucocorticosteroids for alcoholic hepatitis—a Cochrane Hepato-Biliary Group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther. 2008;27(12):1167-1178.
doi pubmed - Diagnosis and treatment of alcohol-associated liver diseases: 2019 practice guidance from the American Association for the Study of Liver Diseases. https://aasldpubs.onlinelibrary.wiley.com/doi/full/10.1002/hep.30866.
- Medical management of severe alcoholic hepatitis: expert review from the clinical practice updates Committee of the AGA Institute. https://www.cghjournal.org/article/S1542-3565(16)30798-4/fulltext#relatedArticles.
- ACG Clinical Guideline: Alcoholic Liver Disease. https://journals.lww.com/ajg/Fulltext/2018/02000/ACG_Clinical_Guideline_Alcoholic_Liver_Disease.9.aspx.
- Butler E, Moller MH, Cook O, Granholm A, Penketh J, Rygard SL, Aneman A, et al. The effect of systemic corticosteroids on the incidence of gastrointestinal bleeding in critically ill adults: a systematic review with meta-analysis. Intensive Care Med. 2019;45(11):1540-1549.
doi pubmed - Yao TC, Huang YW, Chang SM, Tsai SY, Wu AC, Tsai HJ. Association between oral corticosteroid bursts and severe adverse events: a nationwide population-based cohort study. Ann Intern Med. 2020;173(5):325-330.
doi pubmed - Vora P, Pietila A, Peltonen M, Brobert G, Salomaa V. Thirty-year incidence and mortality trends in upper and lower gastrointestinal bleeding in Finland. JAMA Netw Open. 2020;3(10):e2020172.
doi pubmed - Guo CG, Zhang F, Wu JT, Cheung KS, Li B, Law SYK, Leung WK. Divergent trends of hospitalizations for upper and lower gastrointestinal bleeding based on population prescriptions of aspirin, proton pump inhibitors and Helicobacter pylori eradication therapy: Trends of upper and lower gastrointestinal bleeding. United European Gastroenterol J. 2021;9(5):543-551.
doi pubmed - Charilaou P, Devani K, Enjamuri D, Radadiya D, Reddy CM, Young M. Epidemiology of lower GI bleed in the United States - an update from the national inpatient survey 2005-2014. American Journal of Gastroenterology. 2018;113(Supplement):S319.
doi - Khalifa A, Rockey DC. Lower Gastrointestinal Bleeding in Patients With Cirrhosis-Etiology and Outcomes. Am J Med Sci. 2020;359(4):206-211.
doi pubmed - Rabinovitz M, Schade RR, Dindzans VJ, Belle SH, Van Thiel DH, Gavaler JS. Colonic disease in cirrhosis. An endoscopic evaluation in 412 patients. Gastroenterology. 1990;99(1):195-199.
doi - Wang TF, Lee FY, Tsai YT, Lee SD, Wang SS, Hsia HC, Lin WJ, et al. Relationship of portal pressure, anorectal varices and hemorrhoids in cirrhotic patients. J Hepatol. 1992;15(1-2):170-173.
doi - Lanas A, Garcia-Rodriguez LA, Polo-Tomas M, Ponce M, Alonso-Abreu I, Perez-Aisa MA, Perez-Gisbert J, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104(7):1633-1641.
doi pubmed - Devani K, Radadiya D, Charilaou P, Aasen T, Reddy CM, Young M, Brahmbhatt B, et al. Trends in hospitalization, mortality, and timing of colonoscopy in patients with acute lower gastrointestinal bleeding. Endosc Int Open. 2021;9(6):E777-E789.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


