| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://www.gastrores.org |
Original Article
Volume 15, Number 6, December 2022, pages 314-324
Expanding the Use of Endoscopic Retrograde Cholangiopancreatography in Pediatrics: A National Database Analysis of Demographics and Complication Rates
Eric Lorioa, g, Chris Moreaub, Joel Edmund Michalekc, Sandeep Pateld, e, f
aDepartment of Gastroenterology and Hepatology, Tulane University School of Medicine, New Orleans, LA, USA
bDivision of Gastroenterology, Hepatology and Nutrition, Department of Medicine, University of Texas Health San Antonio, TX, USA
cDepartment of Population Health Sciences, University of Texas Health San Antonio, TX, USA
dAdvanced Endoscopy Program, University of Texas Health San Antonio, TX, USA
eDepartment of Gastrointestinal Endoscopy, University Hospital, San Antonio, TX, USA
fCHRISTUS Health, San Antonio, TX, USA
gCorresponding Author: Eric Lorio, Department of Gastroenterology and Hepatology, Tulane University School of Medicine, New Orleans, LA 70112, USA
Manuscript submitted June 16, 2022, accepted July 21, 2022, published online December 1, 2022
Short title: Use of ERCP in Pediatrics
doi: https://doi.org/10.14740/gr1503
| Abstract | ▴Top |
Background: This study aimed to aid in risk assessment of pediatric endoscopic retrograde cholangiopancreatography (ERCP) candidates by utilizing a national pediatric database with a large sample to assess how patient characteristics may affect ERCP complication rates.
Methods: The Kids’ Inpatient Database (KID) is a sample of pediatric discharges in states participating in the Healthcare Cost and Utilization Project (HCUP). This database provides demographic information, hospitalization duration, and outcome information for hospitalizations during which an ERCP occurred. International Classification of Diseases (ICD) codes were used to determine the hospitalization indication. ERCP complication rate was ascertained via ICD codes. All statistical analyses were performed using SAS 9.4.
Results: Complications were seen in 5.4% of hospitalizations with mortality observed in less than 0.2%. This analysis captured a large Hispanic population, specifically in the South and West regions. Gallbladder calculus and cholecystitis were more likely to occur in females. A higher percentage of patients in the age 10 - 17 group were female (72.2% vs. 52.7%, P < 0.01) and Hispanic (33.4% vs. 22.7%, P < 0.01) compared to the age 0 - 9 group. Age 0 - 5 and male gender were associated with lower routine home discharge rates and longer lengths of stay. Complications occurred at a higher rate in ages 0 - 5, though the difference was not statistically significant.
Conclusions: ERCP is a safe procedure for pediatric patients with low complication rates and rare mortality. We found statistically significant differences in the procedure indications between pediatric age groups, races, and genders. Age ≤ 5 years and male gender were associated with more complicated healthcare courses.
Keywords: ERCP; Pediatric; Complication; Pancreatitis; Demographic
| Introduction | ▴Top |
Initially described in 1968, endoscopic retrograde cholangiopancreatography (ERCP) has evolved into an essential tool for the evaluation and management of pancreaticobiliary disorders. This technique has become increasingly safe and sophisticated with recent adult complication rates estimated at 6.5-7.3% in the hands of experienced practitioners [1]. Due to its proven efficacy, ERCP is increasingly accepted as a therapeutic modality in pediatric populations, with a 10-year procedure volume growth of 26.1% from 1999 to 2009 [2]. Despite increasing ERCP usage, there remains a startling paucity of information regarding the relationship between demographics and complication rates in pediatric populations, with published evidence only encompassing small sample sizes or lacking head-to-head comparisons [1, 3-5].
Single-center studies often do not report on differences in indications and risks across pediatric age groups. Infants and younger children are naturally more challenging due to limited navigational space and may require smaller endoscopes with instrument channel limits that make intervention difficult [6-8]. Additionally, congenital mutations and anatomic irregularities are present in a higher percentage of infants and young children presenting for ERCP when compared to the adolescents, who are more likely to present with obstructive biliary stones [9].
Multiple retrospective studies have attempted to illustrate the efficacy and safety of diagnostic and therapeutic ERCP in infants and children, with technical success and complication rates thought to be comparable to adult populations [10]. Much of the lack of US data is owed to the relative infrequency of ERCP performance in pediatrics, with one survey estimating that only 0.1% of all pediatric endoscopies were ERCPs [11]. The relatively small amount of pediatric ERCP experience and research forces providers to extrapolate adult risk factors and preventive strategies to children despite population-based ERCP studies suggesting differences in common indications and patient characteristics [12]. This database analysis aimed to use a large sample population to aid in the understanding of pediatric patient characteristics and to examine pediatric utilization of ERCP in the United States.
| Materials and Methods | ▴Top |
Data for this project were obtained from the 2016 Kids’ Inpatient Database (KID), the largest publicly available all-payer pediatric inpatient care database in the United States. The KID is a sample of pediatric discharges from hospitals in states participating in the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ). HCUP data are based on administrative data - discharge abstracts created by hospitals for billing. Approximately 8 million hospitalizations in 1,000 hospitals are captured in the KID, representing a 20% stratified sample of all US community hospitals. Unweighted, it contains data from approximately 3 million pediatric discharges each year. Four thousand and two hundred US community hospitals are sampled (defined as short-term, non-federal, general and specialty hospitals, excluding hospital units of other institutions and rehabilitation hospitals). The KID contains charge information for pediatric populations covered by private insurance, Medicaid, Medicare, and the uninsured and has been produced every 3 years (1997, 2000, 2003, 2006, 2009, 2012). The KID contains a full calendar year of data with diagnosis and procedure codes reported using the ICD-9/10-Clinical Modification (CM)/Procedure Coding System (PCS). Hospital discharge data for 2015 contained a mix of ICD-9 and ICD-10 data. Because of the complexities of analyzing a mixed data year, the 2015 KID was not released. Instead, the next KID production was released in 2016, with the 2016 statistics comprised of ICD-10 CM/PCS data only.
Using the KID, we identified pediatric (age ≤ 20 years) hospitalizations during which ERCP was performed. Presenting diagnosis, age, sex, race/ethnicity, hospital region, hospitalization duration, and presence or absence of in-hospital mortality were provided by the database for individual hospitalizations. ICD procedure codes (Fig. 1) were used to determine the occurrence of an ERCP. Repeat ERCPs were recognized by identifying a second ERCP coded on a subsequent day after the initial ERCP. Complication related to ERCP was ascertained via a recorded procedure complication occurring on the same day as the ERCP or by pancreatitis diagnosed within 24 h of the documented ERCP (Fig. 1).
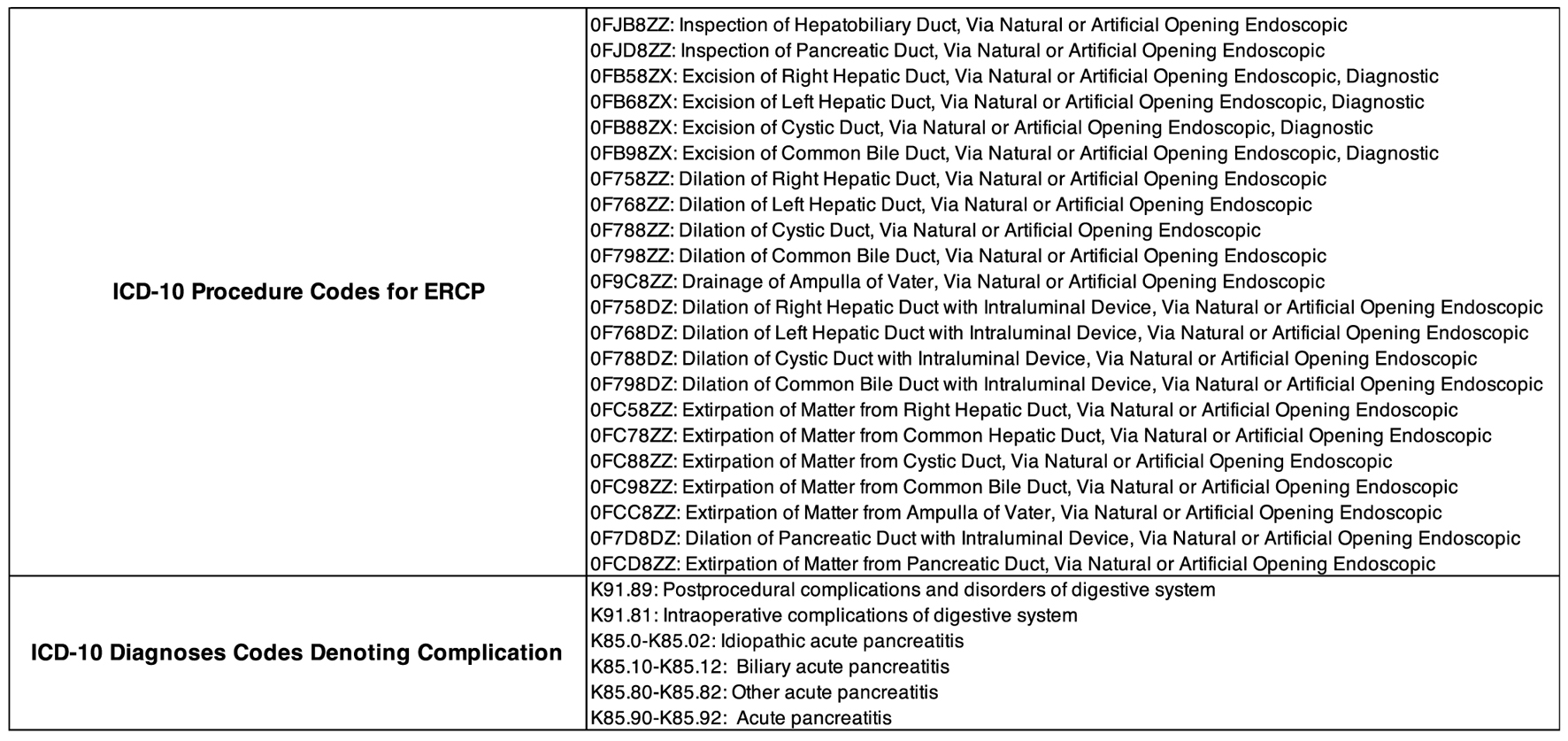 Click for large image | Figure 1. ICD10 procedure codes used to identify an ERCP during a hospitalization. Presenting diagnoses are provided by the KID for each individual hospitalization. Also shown are the codes used to define complication associated with performed ERCP. *A diagnosis code for pancreatitis was captured as a complication if the diagnosis code was entered within 24 h of the documented ERCP. ERCP: endoscopic retrograde cholangiopancreatography; KID: Kids’ Inpatient Database. |
Categorical and binary data were summarized with frequencies and percentages, and length of stay was depicted with the medians, minimum, and maximum. Analyses were carried out with adjustment for hospital clustering with logit, cumulative logit, and identity links for binary, categorical, and continuously distributed dependent variables, respectively. Associations between binary outcomes were summarized with the odds ratio (OR), a 95% confidence interval (CI), and associated P-value. All multivariate analyses were accomplished with mixed effects weighted GEE models with a logit link adjustment for hospital clustering. Disposition and length of stay were analyzed with Wilcoxon tests stratified by hospital. Weights were provided by the HCUP. Age groups 0 - 5 (preschool), 6 - 10 (school age), 11 - 15 (preadolescence), and 16 - 20 (adolescence) were used for comparison in order to provide suitable samples for comparison while capturing distinct pediatric developmental stages. Minors age 0 - 9 and 10 - 17 were also compared to differentiate children from adolescents (as defined by the World Health Organization) [13]. Corrections for multiple testing were not applied. SAS version 9.4 for Windows (SAS Institute, Cary, NC) was used throughout. As part of the HCUP user agreement for patient privacy, frequencies ≤ 10 cannot be reported.
This analysis was approved by the UT Health San Antonio Institutional Review Board. This study does not contain any studies with human or animal subjects performed by any of the authors.
| Results | ▴Top |
The query of the KID 2016 yielded 4,484 discharges that had coded documentation of a performed ERCP. Overall demographic information is depicted in Table 1. Procedure complications were documented in 5.41% of hospitalizations with mortality observed in less than 10 of the hospitalizations. The captured population was overwhelmingly female and adolescent (75.00% over the age of 15). A robust Hispanic population (33.09%) was identified with a large portion of hospitalizations occurring in Western and Southern states (68.12% combined). Acute cholecystitis and calculus of the gallbladder represented the bulk of the admitting diagnoses (49.93%), with pancreatitis only accounting for 12.19% of admissions. Of pediatric patients with a documented ERCP during the hospitalization, 30.03% required a repeat ERCP during the same hospitalization. Of the hospitalizations, 95.2% resulted in a routine home discharge, with a mean length of stay of 4 days.
 Click to view | Table 1. Overall Clinical and Demographic Characteristics of Patients From the 2016 Kids’ Inpatient Database |
Age
When comparing multiple age groups, 0 - 5, 6 - 10, 11 - 15, and 16 - 20, a significantly longer length of stay (P < 0.001) and a lower rate of routine home discharge (P < 0.001) were observed in the younger groups (Table 2). Though the highest rate of complication was seen in the 0 - 5 age group (7.9% of cases), there was no statistical difference in complication rate between age groups (P = 0.68). Younger age was associated with more frequent admission diagnoses of acute pancreatitis (P = 0.001), chronic pancreatitis (P < 0.001), primary sclerosing cholangitis (P = 0.003), malignancy/tumor (P < 0.001), obstruction of the bile duct (P < 0.001), traumatic injury (P < 0.001), and cholangitis (P = 0.01). Patients aged 10 and older more frequently presented with acute cholecystitis (P < 0.001) and calculus of the gallbladder (P = 0.01). There was no statistical difference between age group rates of repeat ERCP.
 Click to view | Table 2. ERCP Age Group Comparison |
There were 1,936 patients identified with an age < 18 years. Overall complication rates were 5.48% in this sample with no difference in complications when comparing age 0 - 9 to 10 - 17 (6.3% vs. 5.4%, P = 0.56). The older age group was predominantly female (72.2% vs. 52.7%, P < 0.001) and Hispanic (33.40% vs. 22.73%, P < 0.001) compared to the younger age group.
Gender
Female gender comprised 77.53% of all patients, though females only made up 52.7% of patients aged 0 - 9. Male gender was associated with an increased rate of complication (female 5%, male 6.9%, P = 0.04), longer hospital stays (median number of days, female 3, male 4, P < 0.001), and decreased rates of routine home discharge (female 96.5%, male 91.9%, P = 0.001) despite similar racial demographics and regional distribution to female gender (Table 3). Male gender was also associated with increased rates of repeat ERCP (male 32.4%, female 29.3%, P = 0.004).
 Click to view | Table 3. Gender Comparison |
Rates of calculus of the gallbladder (P < 0.001), acute cholecystitis (P < 0.001), and chronic cholecystitis (P = 0.006) were significantly higher in females (Fig. 2). Male patients were more likely to present with traumatic injury (P < 0.001), sepsis (P < 0.001), obstruction of the bile duct (P < 0.001), cholangitis (P < 0.001), and primary sclerosing cholangitis (P < 0.001) (Table 3). Males were also found to have a higher rate of chronic pancreatitis in our analysis, with drastically higher rates of chronic pancreatitis in the male subset of the 0 - 9 group (5.8% vs. 1.5%, P = 0.004). Increasing age correlated with increasing rates of acute cholecystitis in both genders. Female gender uniquely demonstrated decreasing diagnosis of traumatic injury (P < 0.001), acute pancreatitis (P = 0.001), cholangitis (P = 0.004), and malignancy (P < 0.001) with increasing age. Alternatively, a diagnosis of obstruction of the bile duct was less frequently seen in male patients with increasing age (P < 0.001).
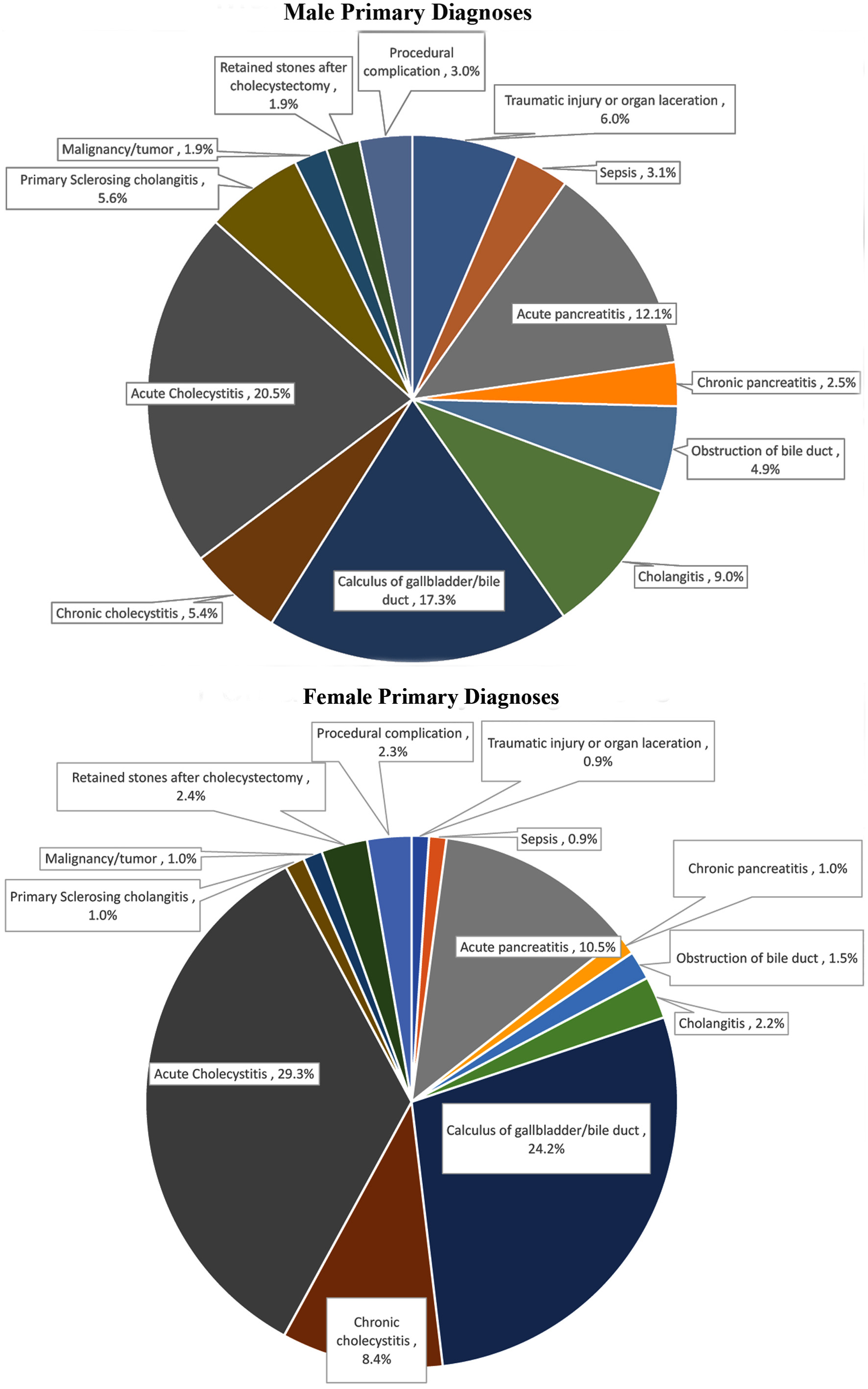 Click for large image | Figure 2. Differences in admission primary diagnosis between genders. Females had statistically higher rates of calculus of the gallbladder/bile duct (P = 0.03) and chronic cholecystitis (P = 0.02). Males had higher rates of traumatic injury (P < 0.001), obstruction of the bile duct (P < 0.001), cholangitis (P = 0.002), and primary sclerosing cholangitis (P = 0.02). |
Race
Of the 4,484 patients in the database, 3,275 self-identified themselves as either non-Hispanic White (NHW) (1,792) or Hispanic (1,483). Only 12.49% and 1.82% identified themselves as Black or Asian/Pacific Islander, respectively (Table 1). The bulk of the Hispanic patients were found in the West and South, comprising 53.9% and 30.0% of those regions, respectively. Compared to Hispanic patients, the NHW group had increased rates of complication (Hispanic 4.4%, NHW 7.1%, P = 0.008), driven primarily by the 16 - 20 age group (Hispanic 4.2%, NHW 7.0%, P = 0.01). Neither median length of stay (Hispanic: 4 days, NHW: 3 days, P = 0.23) nor repeat ERCP rate (Hispanic 27.8%, NHW 31%, P = 0.096) differed significantly between Hispanic and NHW groups (Table 4). The presenting diagnosis for Hispanic patients was more likely to be acute cholecystitis (P < 0.001), and less likely to be traumatic injury (P = 0.002), cholangitis (P = 0.008), primary sclerosing cholangitis (P = 0.005), or due to a procedural complication (P = 0.003) compared to NHW patients.
 Click to view | Table 4. Hispanic vs. White Race Comparison |
Region
Over two-thirds of the documented procedures were performed in the West and South. Higher complication rates were recorded in the Northeast region when compared to the West region (7.7% vs. 4.5%, P = 0.03), with a notable complication rate of 9.8% in Northeast patients aged 17 and younger. Regional complication rates did not vary significantly elsewhere (Table 5). There was a lower rate of routine home discharge in the Northeast region (Northeast (NE) 92.3%, Midwest (M) 94.9%, South (S) 95.7%, West (W) 96.9%, P = 0.001), with increased repeat ERCP rates in the Northeast and Midwest regions (NE 35%, M 34.5%, S 28.4%, W 26.3%, NE vs. S, P = 0.01, NE vs. W, P = 0.002). In-hospital mortality and length of stay (P = 0.13) were similar between all four regions. The West had the most unique racial demographic, with a significantly higher number of Hispanic patients (56.6%) compared to NHW (27%) and Black (5.3%) patients. There was a higher incidence of procedural complication as a presenting diagnosis in the Northeast compared to the South and West (NE 7.7%, M 6.2%, S 4.9%, W 4.5%, NE vs. S, P = 0.05, NE vs. W, P = 0.03). Acute cholecystitis was the most common presenting diagnosis for all regions except for the Northeast, which had a higher rate of calculus of the gallbladder.
 Click to view | Table 5. Region Comparison |
| Discussion | ▴Top |
This database proved useful in its ability to compare trends and outcomes amongst different demographics. Overall complication rates were on the lower end of what has been reported, with recent retrospective studies estimating complications in pediatric ERCP to be as high as 9.4-20.7% [1, 8, 10, 14, 15].
Despite no significant variation in the complication risk between pediatric age groups, it bears consideration that the highest complication rate occurred in the youngest age group (0 - 5), and younger patients were less likely to undergo routine home discharge. The increasing risk of ERCP complications in younger patients has been demonstrated elsewhere, with decreases in success rates and increased rates of complication in ages less than 3 years old [15]. This has been attributed to the smaller endoscopes required for infant populations and challenges with this age group. Thanks to the availability of noninvasive testing such as MRCP, ERCP is now rarely attempted solely for the diagnosis of congenital biliary abnormalities in these infant populations [15].
An important factor in pediatric ERCP outcomes lies in the presenting diagnosis [16]. Pancreatitis remains the most frequently observed post-ERCP complication, reported elsewhere in 1.2-12% of pediatric patients [10, 14]. Our dataset’s most common presenting diagnoses, acute cholecystitis and choledocholithiasis, typically exhibit low rates of post-ERCP pancreatitis [14]. This analysis found that both acute cholecystitis and choledocholithiasis overwhelmingly occurred in older children (ages 11 - 20), as would be expected with the increasing impact of childhood obesity with age and use of oral contraception in adolescents [12, 16]. Rates of complication in this group were lower than those found in the younger pediatric age groups. The presenting diagnosis of pancreatitis, which has been associated with increased rates of post-ERCP pancreatitis, was more often found in ages 0 - 5 [17-19]. When combined, these indication differences between age groups greatly contributed to the elevated complication rate and increased rate of repeat ERCP in ages ≤ 5.
Our results reinforce previous observations that females more frequently present with gallstone disease. This difference increases with age, likely owed to hormone driven increases in levels of biliary cholesterol seen in females during puberty [20]. Pubertal hormone changes also play a role in promoting biliary dyskinesia which may contribute to the impairment of gallbladder motility [20].
The finding that male gender is associated with increased complication risk and longer hospitalizations in pediatrics differs from what has been observed in adults [17, 21]. Procedure indication again plays a role in interpreting these results. Our analysis found a correlation between male gender and chronic pancreatitis, a diagnosis that carries increased rate of complication. A variety of anatomic obstacles can develop in chronic pancreatitis due to the local effects of inflammation or glandular fibrosis [22]. These patients represent a distinct challenge, as there is known difficulty in ERCP with pancreatic anatomic abnormalities [9, 23]. Females were much more likely to present with diagnoses with lower complication rates, such as cholecystitis and choledocholithiasis [14]. While both genders demonstrated an increasing incidence of acute cholecystitis with age, adolescent females experienced a higher overall rate of acute cholecystitis. Females also had significantly lower rates of pancreatitis with age. These factors largely explain the gender difference in our dataset.
The KID contains a large subset of Hispanic patients due to a substantial number of ERCPs reported in the West and South. This provided critical representation of a racial demographic that is often under-reported in population-based studies [24]. A larger percentage of patients aged 11 - 20 were Hispanic, and the primary diagnosis of acute cholecystitis was more prevalent in Hispanic patients compared to Caucasian patients. This highlights the role of ERCP in Hispanic adolescents, as this subgroup appears to be more susceptible to the biliary stone disease.
Over 30% of children in this dataset required a same-stay repeat ERCP, which is much higher than other studies have quoted. Early repeat ERCP is thought to be performed in 2.3-10.0% of adult patients [25]. Repeat ERCP is associated with increased complication rates, with 13.4-33% experiencing complication after re-exploration of the pancreaticobiliary system in other studies [26]. This could contribute to the increased rate of in-hospital complication and decreased routine home discharge seen in the Northeast region, where we found a higher rate of repeat ERCP. The exact reason for the regional difference in repeat ERCP rate is unclear, though it should be noted that a larger sample of NHW patients were recorded in the Northeast. A higher number of patients in the Northeast also presented with a primary diagnosis of “procedure complication”, perhaps indicating that these hospitalizations captured a high number of presentations for repeat ERCP, which carries increased complication risk.
A limitation of this study was an inability to identify complications beyond 24 h, which likely underestimates the overall complication rate. The decision to only assign complications up to this mark was made in order to ensure that all recorded complications and cases of post-procedure pancreatitis were associated with the procedure. The KID database also does not contain information on whether individual patients received further surgical or endoscopic interventions after discharge, and complications which occurred after discharge are not captured. Barakat et al examined 30-day readmission rates in the HCUP database, finding readmission rates of 13.3% in patients ≤ 20 years old, with a significantly higher number of male readmissions and readmitted patients under age 5 [12]. This speaks to the number of patients that experience prolonged, fragmented healthcare courses and corroborated the trends we discussed above: that males and younger children represent more challenging subgroups. Our dataset does not provide information on individual procedure interventions (i.e., stent placement, sphincterotomy, etc.) or the types of complications that occurred, and we are unable to directly compare the outcomes of procedure indications due to small subgroup sizes. The dataset also does not include information whether the biliary duct, pancreatic duct, or both were cannulated during the procedure. Only associations, not causal relationships, can be defined using administrative data.
The quality of information contained within this dataset is dependent on proper documentation of complications and accurate coding of presenting diagnoses. Discrepancies may contribute to underreporting of true complication rates. Despite this, we can be confident that mortality resulting from pediatric ERCP is exceedingly rare, with less than 10 patients experiencing in-hospital mortality in our analysis [1, 15].
In conclusion, this study documents that the overall risk of complications after pediatric ERCP is comparable to accepted ERCP complication levels in other groups. Female and Hispanic patients make up a larger percentage of those requiring ERCP in adolescence, and younger patients and males are more likely to experience prolonged lengths of stay and complication. The indication for an ERCP plays a significant role in the subsequent procedure outcome, and further study is needed to clearly outline how particular interventions affect both short and long-term complication rates.
Acknowledgments
None to declare.
Financial Disclosure
This project was funded, in part, by the 2020 American College of Gastroenterology Resident Clinical Research Award.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
As a retrospective database analysis, informed consent from individuals included was not obtained.
Author Contributions
Eric Lorio planned study, assisted in collection and interpretation of data, and drafted the manuscript. Chris Moreau planned study, and assisted in interpretation of data and manuscript revisions. Joel Edmund Michalek assisted in planning of study and collection and interpretation of data, and performed analysis of dataset. Sandeep Patel planned study, assisted in data interpretation, and manuscript revisions.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Giefer MJ, Kozarek RA. Technical outcomes and complications of pediatric ERCP. Surg Endosc. 2015;29(12):3543-3550.
doi pubmed - Pant C, Sferra TJ, Barth BA, Deshpande A, Minocha A, Qureshi WA, Olyaee M, et al. Trends in endoscopic retrograde cholangiopancreatography in children within the United States, 2000-2009. J Pediatr Gastroenterol Nutr. 2014;59(1):57-60.
doi pubmed - Yildirim AE, Altun R, Ocal S, Kormaz M, Ozcay F, Selcuk H. The safety and efficacy of ERCP in the pediatric population with standard scopes: Does size really matter? Springerplus. 2016;5:128.
doi pubmed - Halvorson L, Halsey K, Darwin P, Goldberg E. The safety and efficacy of therapeutic ERCP in the pediatric population performed by adult gastroenterologists. Dig Dis Sci. 2013;58(12):3611-3619.
doi pubmed - Issa H, Al-Haddad A, Al-Salem AH. Diagnostic and therapeutic ERCP in the pediatric age group. Pediatr Surg Int. 2007;23(2):111-116.
doi pubmed - Iqbal CW, Baron TH, Moir CR, Ishitani MB. Post-ERCP pancreatitis in pediatric patients. J Pediatr Gastroenterol Nutr. 2009;49(4):430-434.
doi pubmed - Tagawa M, Morita A, Imagawa K, Mizokami Y. Endoscopic retrograde cholangiopancreatography and endoscopic ultrasound in children. Dig Endosc. 2021;33(7):1045-1058.
doi pubmed - Avitsland TL, Aabakken L. Endoscopic retrograde cholangiopancreatography in infants and children. Endosc Int Open. 2021;9(3):E292-E296.
doi pubmed - Shah R, Cohen RZ, Mekaroonkamol P, Taylor A, Freeman AJ, Fritzen C, Sauer C, et al. Retrospective multicenter matched controlled comparison of endoscopic retrograde cholangiopancreatography in pediatric patients: a 10-year experience. J Pediatr Gastroenterol Nutr. 2020;70(5):568-573.
doi pubmed - Mercier C, Pioche M, Albuisson E, Ponchon T, Gonzalez JM, Barthet M, Boytchev I, et al. Safety of endoscopic retrograde cholangiopancreatography in the pediatric population: a multicenter study. Endoscopy. 2021;53(6):586-594.
doi pubmed - Kudo T, Abukawa D, Nakayama Y, Segawa O, Uchida K, Jimbo K, Shimizu T. Nationwide survey of pediatric gastrointestinal endoscopy in Japan. J Gastroenterol Hepatol. 2021;36(6):1545-1549.
doi pubmed - Barakat MT, Cholankeril G, Gugig R, Berquist WE. Nationwide evolution of pediatric endoscopic retrograde cholangiopancreatography indications, utilization, and readmissions over time. J Pediatr. 2021;232:159-165.e151.
doi pubmed - Age limits and adolescents. Paediatr Child Health. 2003;8(9):577-578.
doi pubmed - Deng Z, Zeng J, Lv C, Jiang L, Ji J, Li X, Hao L, et al. Prevalence and Factors Associated with Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis in Children. Dig Dis Sci. 2021;66(1):224-230.
doi pubmed - Keil R, Drabek J, Lochmannova J, Stovicek J, Koptova P, Wasserbauer M, Frybova B, et al. ERCP in infants, children, and adolescents-Different roles of the methods in different age groups. PLoS One. 2019;14(1):e0210805.
doi pubmed - Frybova B, Drabek J, Lochmannova J, Douda L, Hlava S, Zemkova D, Mixa V, et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS One. 2018;13(5):e0196475.
doi pubmed - Ding X, Zhang F, Wang Y. Risk factors for post-ERCP pancreatitis: A systematic review and meta-analysis. Surgeon. 2015;13(4):218-229.
doi pubmed - Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54(4):425-434.
doi pubmed - Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60(5):721-731.
doi - Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics. 2012;129(1):e82-88.
doi pubmed - Koseoglu H, Solakoglu T, Basaran M, Ozer Sari S, Tahtaci M, Yaman S, Selvi E, et al. Risk factors for post-ERCP pancreatitis: it depends on the ERCP indication. Acta Gastroenterol Belg. 2020;83(4):598-602.
- Hart PA, Conwell DL. Chronic pancreatitis: managing a difficult disease. Am J Gastroenterol. 2020;115(1):49-55.
doi pubmed - Balan GG, Arya M, Catinean A, Sandru V, Moscalu M, Constantinescu G, Trifan A, et al. Anatomy of Major Duodenal Papilla Influences ERCP Outcomes and Complication Rates: A Single Center Prospective Study. J Clin Med. 2020;9(6):1637.
doi pubmed - Sharma A, Rakholiya JH, Madapu A, Sharma S, Jha A. Trend and predictors of the utilization of endoscopic retrograde cholangiopancreatography in acute pancreatitis hospitalizations. Cureus. 2020;12(11):e11420.
doi - Cote GA, Imler TD, Xu H, Teal E, French DD, Imperiale TF, Rosenman MB, et al. Lower provider volume is associated with higher failure rates for endoscopic retrograde cholangiopancreatography. Med Care. 2013;51(12):1040-1047.
doi pubmed - Sugiyama M, Suzuki Y, Abe N, Masaki T, Mori T, Atomi Y. Endoscopic retreatment of recurrent choledocholithiasis after sphincterotomy. Gut. 2004;53(12):1856-1859.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


