| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website http://www.gastrores.org |
Short Communication
Volume 12, Number 2, April 2019, pages 93-95
A Novel Care Model for Neonatal Intestinal Failure Patients Is Associated With Cost Savings and Improved Outcomes
Erin Johnsona, Anna Ermartha, Mark Deneaua, b
aDepartment of Pediatrics, Division of Gastroenterology, Hepatology and Nutrition, University of Utah, Salt Lake City, UT, USA
bCorresponding Author: Mark Deneau, Division of Gastroenterology, Hepatology and Nutrition, University of Utah, 81 N. Mario Capecchi Dr. Salt Lake City, UT 84113, USA
Manuscript submitted January 31, 2019, accepted March 5, 2019
Short title: A Novel Care Model for Intestinal Failure
doi: https://doi.org/10.14740/gr1149
| Abstract | ▴Top |
Background: Neonates with intestinal failure (IF) have prolonged admissions in the neonatal intensive care unit (NICU) and require lifelong follow-up with gastroenterology (GE) as outpatients. Inpatient management of these patients typically relies on many rotating practitioners and currently discharge criteria do not exist. We sought to create standardized discharge criteria with a continuity care model for neonatal IF patients.
Methods: Inpatient care was streamlined to two GE physicians with weekly consultations. We implemented standardized discharge goals for both enteral and total parental nutrition (TPN) by: 1) Enteral feedings of at least 5 mL/h were tolerated; 2) Stable central venous access was intact; 3) TPN was cycled to 20 h/day or less; and 4) No other medical issues required NICU admission. Patient records were reviewed after 18 months of implementing standardized discharge criteria and we compared their outcomes to a historical cohort of IF patients.
Results: Optimal discharge criteria were met in 12 patients and a cohort of 26 historical patients was used for comparison. Patients in optimal versus historical groups had similar baseline characteristics (medians, all P values = non-significant (NS)): gestational age (36 vs. 35 weeks), birth weight (1,990 vs. 2,076 g), birth length (45 vs. 44 cm), and small bowel length after definitive surgery (63 vs. 55 cm). Compared to the historical group, the optimal cohort was discharged earlier (median length of stay 69 vs. 126 days, P < 0.01), with a reduced total stay of 684 NICU days, fewer central line-associated bloodstream infections (CLABSIs) (4 vs. 10 per 1,000 patient days, P = 0.04), and had fewer readmissions (7 vs. 17 per 1,000 patient days, P < 0.01), respectively.
Conclusions: Concentrating the care of IF patients to a GE team invested in long-term care, while implementing safe discharge criteria, resulted in a dramatic length of stay reduction with fewer CLABSIs and readmissions compared to historical management. At approximately 4,000 dollars per day in NICU hospital charges, this program saved over 2.7 million dollars in care costs while allowing families and their infants more time at home. The safety and applicability of the optimal discharge criteria presented here should be studied further. Similar programs may be effective at other large NICUs.
Keywords: Care model; Neonatal intestinal failure patients; Discharge criteria; Cost savings; Improved outcomes
| Introduction | ▴Top |
Inadequate gut absorptive surface area or defective gut motility may lead to total parental nutrition (TPN) dependence, termed intestinal failure (IF). Congenital anatomic abnormalities, necrotizing enterocolitis and severe motility defects account for most cases of IF [1]. Neonates with IF have prolonged admissions in the neonatal intensive care unit (NICU), have increased healthcare expenditures [2], and ultimately require lifelong follow-up with gastroenterology (GE) as outpatients. In most centers, NICU care of these patients is shared between NICU teams, surgeons, and GI consultants who rotate on and off service at least weekly, with variable interest and expertise in IF. Long-term decision making in this complex patient population is thus shared amongst short-term providers who may or may not have an investment in outpatient care, and who may not feel that they have the resources to discharge a patient on parenteral nutrition. In our own NICU, we noticed that this pattern was associated with highly variable discharge criteria and unnecessary increases in length of stay (LOS). Patients were often held to attempt to achieve arbitrary enteral feeding goals when it was clear from their post-operative anatomy that they would never achieve enteral autonomy in the first 6 - 12 months of life. Outpatient-based multidisciplinary care models for IF have been described and were associated with improved patient outcomes [3], but little is published on inpatient care programs or optimal discharge timing from the hospital. We aimed to assess the positive and negative impact of a simple intervention in the NICU to shorten LOS for IF patients.
| Materials and Methods | ▴Top |
We undertook a quality improvement initiative to centralize care in NICU patients with IF and institute standardized discharge criteria. Two gastroenterologists who manage outpatients with IF, central lines and TPN were assigned to rotate weekly in our NICU. They performed all nonurgent consultations, family care conferences, and weekly inpatient follow-up. We implemented standardized, optimal discharge goals for patients with IF (Table 1) to better identify patients who could be safely cared for at home. All post-NICU outpatient care was performed by the same two gastroenterologists. After 18 months, we reviewed medical records of patients who met optimal discharge criteria and compared their outcomes to a historical cohort of IF patients. We assessed frequency of central line-associated bloodstream infection (CLABSI) as well as readmission to the hospital. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration, and with institutional review board approval.
 Click to view | Table 1. Optimal Discharge Timing Criteria for Neonates With Intestinal Failure |
| Results | ▴Top |
During the study period, optimal discharge criteria were met in 12 patients with IF (optimal group). Three patients with IF did not meet discharge criteria due to needs surrounding care of a tracheostomy, progressive liver disease, and lack of a safe home environment, respectively. A cohort of 26 historical patients was identified (historical group) for comparison. The etiology of IF in the optimal versus historical group was gastroschisis with bowel atresias in 75% vs. 53%, volvulus in 8% vs. 11%, necrotizing enterocolitis in 9% vs. 27%, and other in 8% vs. 9%, respectively (all P = NS). Patients in optimal and historical groups had similar baseline characteristics (medians, all P = NS): gestational age (36 vs. 35 weeks), birth weight (1,990 vs. 2,076 g), birth length (45 vs. 44 cm), and small bowel length after definitive surgery (63 vs. 55 cm), respectively (Fig. 1). Compared with the historical group, the optimal group was discharged much earlier (median LOS 69 vs. 126 days, P < 0.01) (Fig. 2), experienced fewer CLABSIs (4 vs. 10 per 1,000 patient days, P = 0.04), and was readmitted less frequently (7 vs. 17 per 1,000 patient days, P < 0.01). Both groups achieved enteral autonomy during the first year after discharge at similar rates: 5/12 (42%) in optimal and 8/26 (31%) in historical groups (P = NS). There were no deaths in 1 year of post-discharge follow-up in either group.
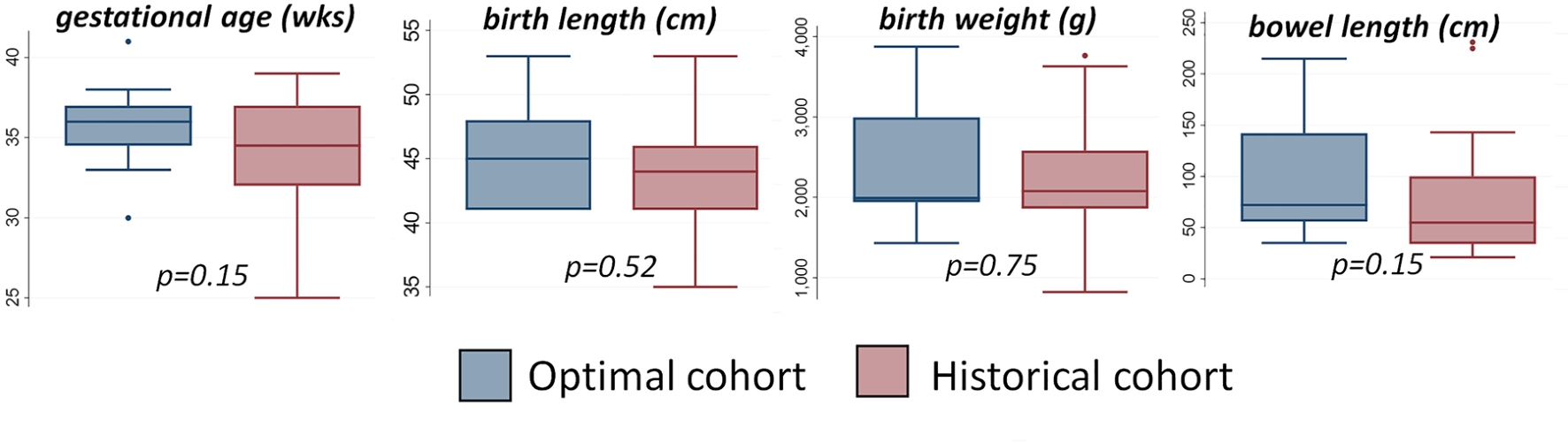 Click for large image | Figure 1. Baseline patient characteristics in the optimal discharge versus historical cohorts. |
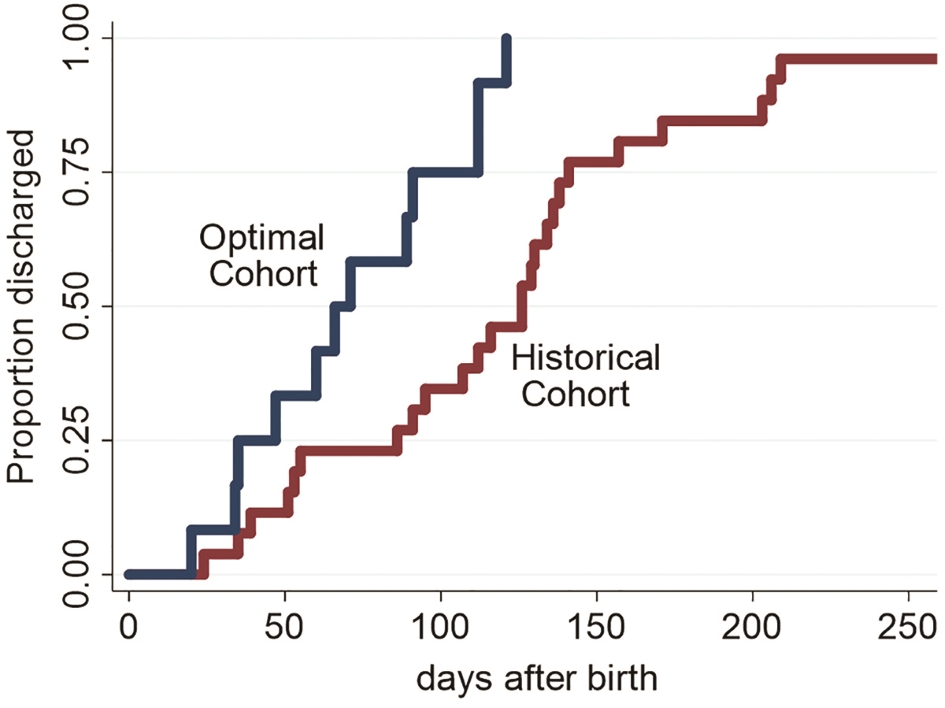 Click for large image | Figure 2. Time to NICU discharge amongst infants with intestinal failure utilizing optimal discharge criteria versus historical management practices. |
| Discussion | ▴Top |
When management of IF in the NICU was restricted to a small team of gastroenterologists with an investment in outpatient care who instituted standardized discharge criteria, LOS decreased substantially without untoward safety events. This change in practice resulted in savings of 684 NICU days (57 days per patient), with fewer CLABSIs after discharge and fewer readmissions compared to historical management practices. At approximately 4,000 dollars per day in hospital charges to stay in a NICU, this program saved over 2.7 million dollars in care costs while allowing families and their infants more time at home. Providers established early relationships with families over multiple encounters prior to discharge, with repeated opportunities for education, anticipatory guidance and shared decision making. Many patients with IF can be managed safely at home, at substantial cost savings. The safety and applicability of the optimal discharge criteria presented here should be studied further. Similar programs may be effective at other large academic medical centers.
Acknowledgments
None to declare.
Financial Disclosure
MD is funded by the Primary Children’s Hospital Foundation, and the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Numbers KL2TR001065 and 8UL1TR000105 (formerly UL1RR025764). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
MD has consulted for HighTide Biopharmaceuticals USA. EJ and AE have nothing to declare.
Informed Consent
Not applicable.
Author’s Contribution
All authors participated in study design, data collection, data analysis, and manuscript preparation.
| References | ▴Top |
- Salvia G, Guarino A, Terrin G, Cascioli C, Paludetto R, Indrio F, Lega L, et al. Neonatal onset intestinal failure: an Italian Multicenter Study. J Pediatr. 2008;153(5):674–676.e2.
- Kosar C, Steinberg K, de Silva N, Avitzur Y, Wales PW. Cost of ambulatory care for the pediatric intestinal failure patient: One-year follow-up after primary discharge. J Pediatr Surg. 2016;51(5):798-803.
doi pubmed - Stanger JD, Oliveira C, Blackmore C, Avitzur Y, Wales PW. The impact of multi-disciplinary intestinal rehabilitation programs on the outcome of pediatric patients with intestinal failure: a systematic review and meta-analysis. J Pediatr Surg. 2013;48(5):983-992.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.


