| Definition | Bleeding from the pancreatic duct into duodenum via the ampulla of Vater. | Bleeding from the biliary tract into duodenum via ampulla of Vater. | Bleeding from the aorta into the duodenum (most common) via fistula between aorta and duodenum. |
| Source | Pancreas, pancreatic pseudocyst. | Intrahepatic, extrahepatic like gall bladder or bile duct. | Aorta. |
| Bleeding vessel | Peripancreatic vessels like splenic, gastroduodenal, pancreaticoduodenal, splenic and sometimes hepatic artery. | Hepatic artery, branch of right or left hepatic artery. | Aorta. |
| Site of bleeding into the gastrointestinal tract | Second part of duodenum (ampulla of Vater). | Second part of duodenum (ampulla of Vater). | Third part of duodenum (most common). |
| Classic triad | Abdominal pain, gastrointestinal hemorrhage and hyperamylasemia. | Abdominal pain, gastrointestinal hemorrhage and jaundice. | Abdominal pain, gastrointestinal hemorrhage and pulsatile abdominal mass. |
| Characteristic picture | Crescendo-decrescendo abdominal pain followed by hemorrhage with a repeat cycle of pain followed by hemorrhage. | Abdominal pain and hemorrhage usually with a recent history of instrumentation. | “Herald” hemorrhage followed hours, days, or weeks later by catastrophic hemorrhage. |
| Causes | Chronic pancreatitis, pancreatic pseudocyst, pancreatic tumors, iatrogenic like EUS/ERCP, vascular malformations, and so on. | Iatrogenic (liver biopsy, percutaneous transhepatic cholangiography, instrumentation, and so on), trauma, hepatobiliary malignancy, inflammation (cholangitis, vasculitis, gallstone disease), parasitic infection, vascular malformation, and so on. | Aortic aneurysm (majority atherosclerotic, followed by mycotic aneurysms), septic aortitis, radiation, carcinoma, ulcers, and so on. |
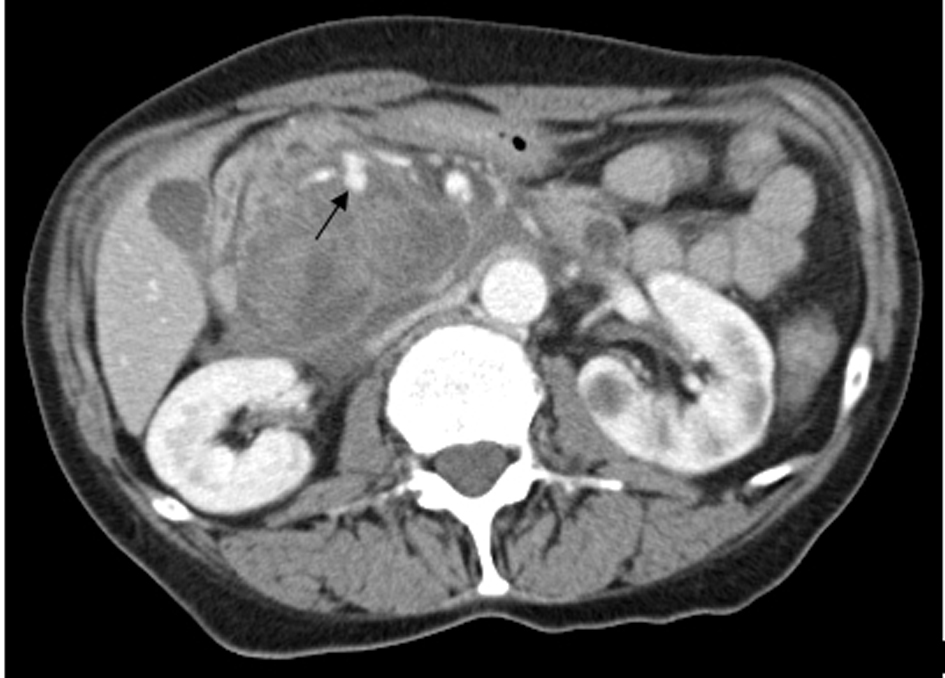
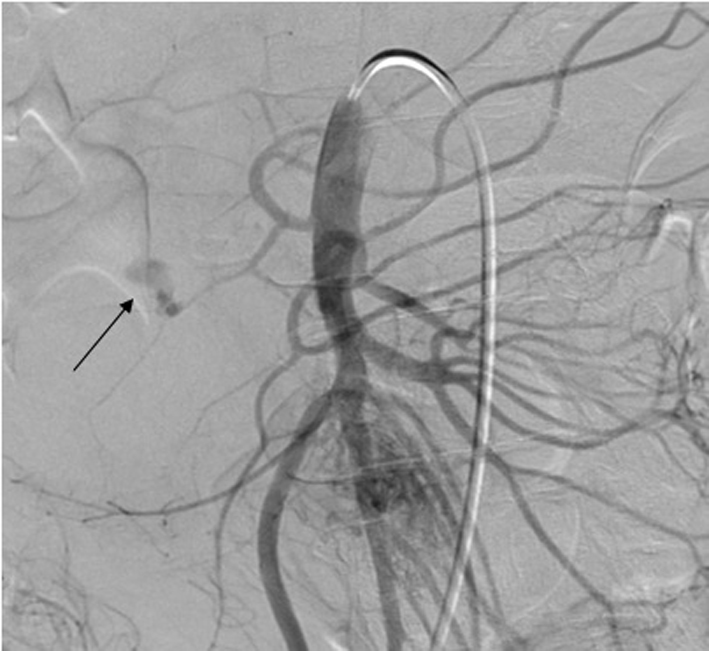
| Diagnostic test | Contrast CT scan very helpful, EGD (diagnostic in 30%), angiography. | Contrast CT scan very helpful, EGD (diagnostic in 12%), ERCP in some cases, technitium red cell scan in some cases, angiography. | Contrast CT scan the most diagnostic. EGD in initial phase when bleeding is herald. Angiography usually not performed as most patients are critically ill when considered for angiography. |
| Treatment | Transcatheter arterial embolization of the pancreatic vessel, Surgery is TAE fails; includes ligation of bleeding vessel, excision of aneurysm, central/distal pancreatectomy. | Transcatheter arterial embolization of hepatic artery (first approach). Surgery if TAE fails; includes ligation of bleeding vessel, excision of aneurysm. Further options depend on site of bleeding; partial hepatectomy, cholecystectomy. | Emergent laparotomy. Debridement of diseased aorta and repair with prosthetic graft along with primary repair of the gastrointestinal tract. |