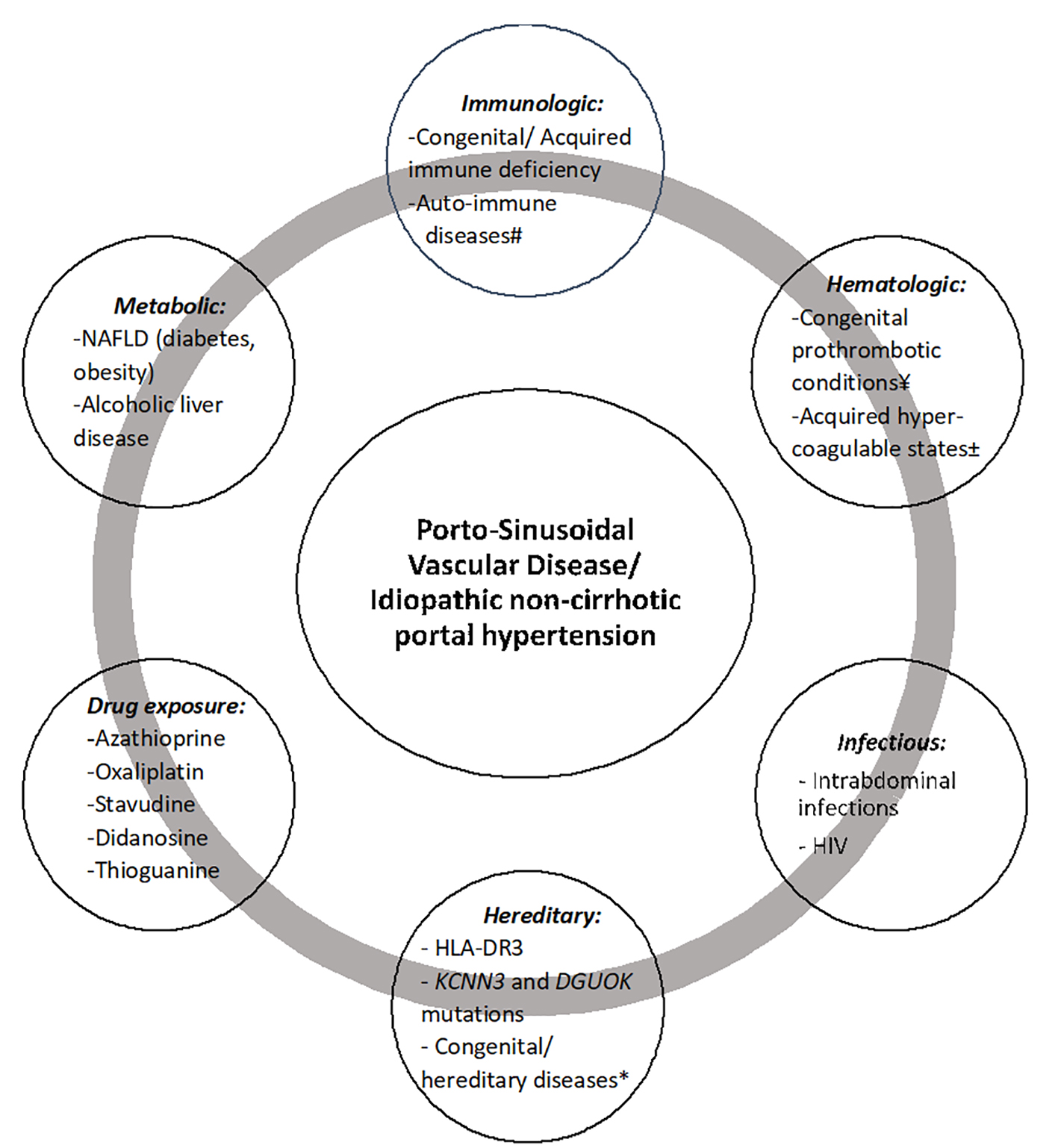
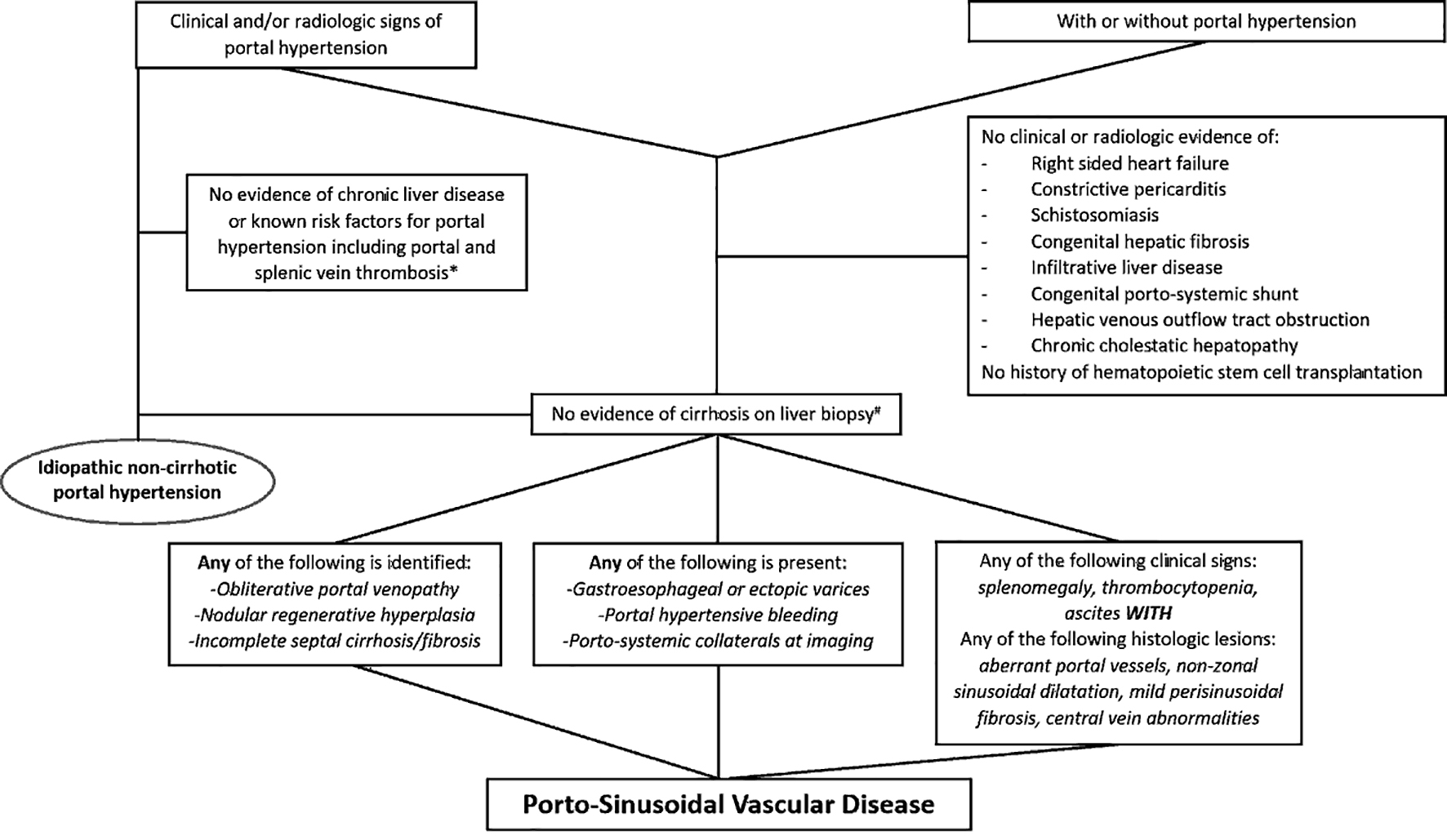
| Idiopathic portal hypertension | Kobayashi et al (1976) [19], Okuda et al (1982) [22], Nakanuma et al (1989) [23], Saito et al (1993) [24], Oikawa et al (1998) [25], Yamaguchi et al (1999) [26], Okudaira et al (2002) [27], Tsuneyama et al (2002) [28], Kogawa et al (2005) [29], Matsutani et al (2005) [30], Chang et al (2009) [31], Seijo et al (2012) [32], Furuichi et al (2013) [33], Siramolpiwat et al (2014) [34], Kotani et al (2015) [35] |
| Non-cirrhotic portal fibrosis | Sarin et al (1987) [36], Mukta et al (2017) [20], Sood et al (2017) [37] |
| Obliterative portal venopathy | Mikkelsen et al (1965) [38], Nayak et al (1969) [39], Cazals-Hatem et al (2011) [40], Glatard et al (2012) [41], Aggarwal et al (2013) [42], Franchi-Abella et al (2014) [43], Arora et al (2015) [44], Guido et al (2016) [12], Besmond et al (2018) [45] |
| Hepatoportal sclerosis | Mikkelsen et al (1965) [38], Girard et al (2005) [46], Fiel et al (2007) [47], Krishnan et al (2012) [48] |
| Benign intrahepatic portal hypertension | Levison et al (1982) [49] |
| Intrahepatic non-cirrhotic portal hypertension | Kingham et al (1981) [50], Krasinskas et al (2005) [6], Eapen et al (2011) [51] |
| Non-cirrhotic portal hypertension | Ohbu et al (1994) [52], Nakanuma et al (1996) [16], Rajekar et al (2011) [3], Rajesh et al (2018) [53], Gioia et al (2018) [54], Nicoara-Farcau et al (2020) [55], Gioia et al (2020) [56] |
| Idiopathic non-cirrhotic intrahepatic portal hypertension | Hillaire et al (2002) [21], Goel et al (2011) [57] |
| Partial nodular transformation | Sherlock et al (1966) [58], Wanless et al (1985) [59] |
| Nodular regenerative hyperplasia | Steinert et al (1959) [60], Wanless et al (1990) [61], Radomski et al (2000) [62], Austin et al (2004) [63], Malamut et al (2008) [64], Leung et al (2009) [65], Jharap et al (2015) [66] |
| Idiopathic presinusoidal portal hypertension | Polish et al (1962) [67] |
| Incomplete septal cirrhosis | Sciot et al (1988) [68] |