| Two-component gallbladder mixed neuroendocrine non-neuroendocrine neoplasms |
| 1 | M/50 | Symptomatic cholelithiasis | A | NA/< 1 | LCNEC, AC | A | A | Chol | DF (12) | [1] |
| 2 | F/48 | Abdominal pain | A | Fundus/3.5 | LCNEC, AC | P | A | Chol, Ehx | NA | [5] |
| 3 | F/68 | Jaundice | P | Fundus/3.1 | LCNEC, AC | P | LN | Chol, Ehx | DF (12) | [8] |
| 4 | F/55 | Back pain, fever | P | Body/4.9 | LCNEC, SCNEC, AC | A | A | Chol | DF (20) | [15] |
| 5 | M/85 | Anorexia, weight loss | P | Fundus/1.5 | LCNEC, AC | A | Liver | Chol, Chem (Carb, Eto), Lant | Died (21) | [16] |
| 6 | F/55 | Abdominal pain | P | Gallbladder bed/14 | SCNEC, AC | P | Pancreas, omentum | Chol, Oct | DF (7) | [17] |
| 7 | M/59 | Abdominal pain | NA | Body/4 | LCNEC, AC | P | LN | Chol | NA | [18] |
| 8 | M/45 | Abdominal pain, jaundice | P | Fundus/5.7 | LCNEC, AC | P | NA | Chol | NA | [19] |
| 9 | M/56 | Exophthalmos | P | Entire gallbladder/9 | LCNEC, AC | P | Multiple organs, LN | Chem, Rad | Died (36) | [20] |
| 10 | F/54 | Postprandial epigastric pain | A | Fundus and body/NA | LCNEC, AC | A | LN | Cho, EHBD resection | DF (24) | [21] |
| 11 | F/63 | Abdominal pain | P | Body/2 | LCNEC, AC | A | A | Chol, Phx, Lnd | DF (12) | [22] |
| 12 | F/62 | Asymptomatic | A | Fundus/2 | NEC, AC | A | A | Chol, Phx, Lnd | NA | [23] |
| 13 | F/55 | Postprandial RUQ pain | P | Fundus/3.5 | LCNEC, AC | A | A | Chol, Revision | NA | [24] |
| 14 | F/62 | Abdominal and RUQ pain | A | Fundus/5.3 | LCNEC, AC | A | A | Chol, Phx, Lnd, Rad, Chem (Cis, Eto) | Died (2) | [25] |
| 15 | F/42 | RUQ pain | A | Gallbladder fossa/7.4 | SCNEC, AC | P | A | Chol, Phx, Lnd, Chem (Cis: 75 mg/m2; Eto: 120 mg/m2), Som | Died (21) | [26] |
| 16 | F/70 | Cholecystolithiasis | P | NA/3.5 | SCNEC, WDAC | P (NEC) | LN (NEC) | NA | NA | [27] |
| 17 | F/70 | NA | NA | NA/4.5 | LCNEC, PAC | A | NA | NA | NA | [27] |
| 18 | F/70 | Cholecystolithiasis | P | NA/4.5 | NEC G2, WDAC | A | Duodenum invasion (NET) | NA | NA | [27] |
| 19 | F/60 | Cholecystolithiasis | P | NA/1.5 | SCNEC, PAC | A | LN (NEC & AC) | NA | NA | [27] |
| 20 | F/50 | NA | NA | NA/15 | LCNEC, WDAC | P | LN(NEC) | NA | NA | [27] |
| 21 | M/58 | Epigastric pain | NA | NA/15 | SCNEC, WDAC | P | Liver (portal vein) | RHT | Died (4) recurrence | [28] |
| 22 | F/56 | RUQ pain and weight loss | NA | NA | SCNEC, AC | P | Liver (Recurrence) | Chol, EHX, Chem (Carb, Eto), Som | Alive (24), good response to Chem | [29] |
| Three-component gallbladder mixed neuroendocrine non-neuroendocrine neoplasms |
| 23 | F/62 | RUQ pain, anorexia, jaundice | A | NA/6.5 | AC, SCC, SCNEC | P | Liver | Palliative Chol | Died (5) (septicemia) | [7] |
| 24 | F/70 | Epigastric pain | NA | Fundus/3.6 | AC, SCC, NEC | A | LN, liver | Chol, Phx | Died (32) | [9] |
| 25 | F/81 | Abdominal pain, weight loss, jaundice | P | Neck/5 | AC, SCC, LCNEC | P | Bone | Palliative Chol | NA | [10] |
| 26 | F/80 | Asymptomatic | A | Fundus/8.2 | AC, SCC, NEC G2 SARC | A | A | Chol, Lnd | Alive (8) | [11] |
| 27 | F/81 | Asymptomatic | P | Fundus/4 | AC, SCC, LCNEC, SARC | A | LN | Chol, Phx | Alive (48) | [12] |
| 28 | M/52 | Epigastric pain, fever | NA | NA | AC (40%), SCC (50%), LCNEC (10%) | A | A | Chol, Chem (Gem, Oxa) | NA | [13] |
| 29 | F/54 | Epigastric pain | P | Fundus/4.3 | AC (10%), SCC (80%), LCNEC (10%) | A | Liver, LN | Chol, Phx, Chem (Cis, Gem, Epir), Rad | Died (13) | [14] |
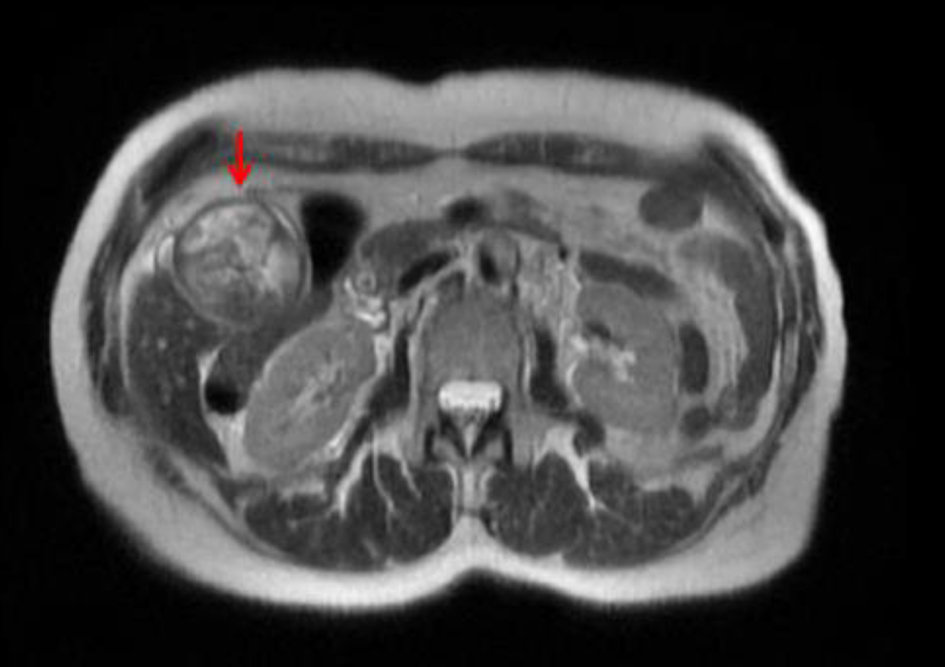
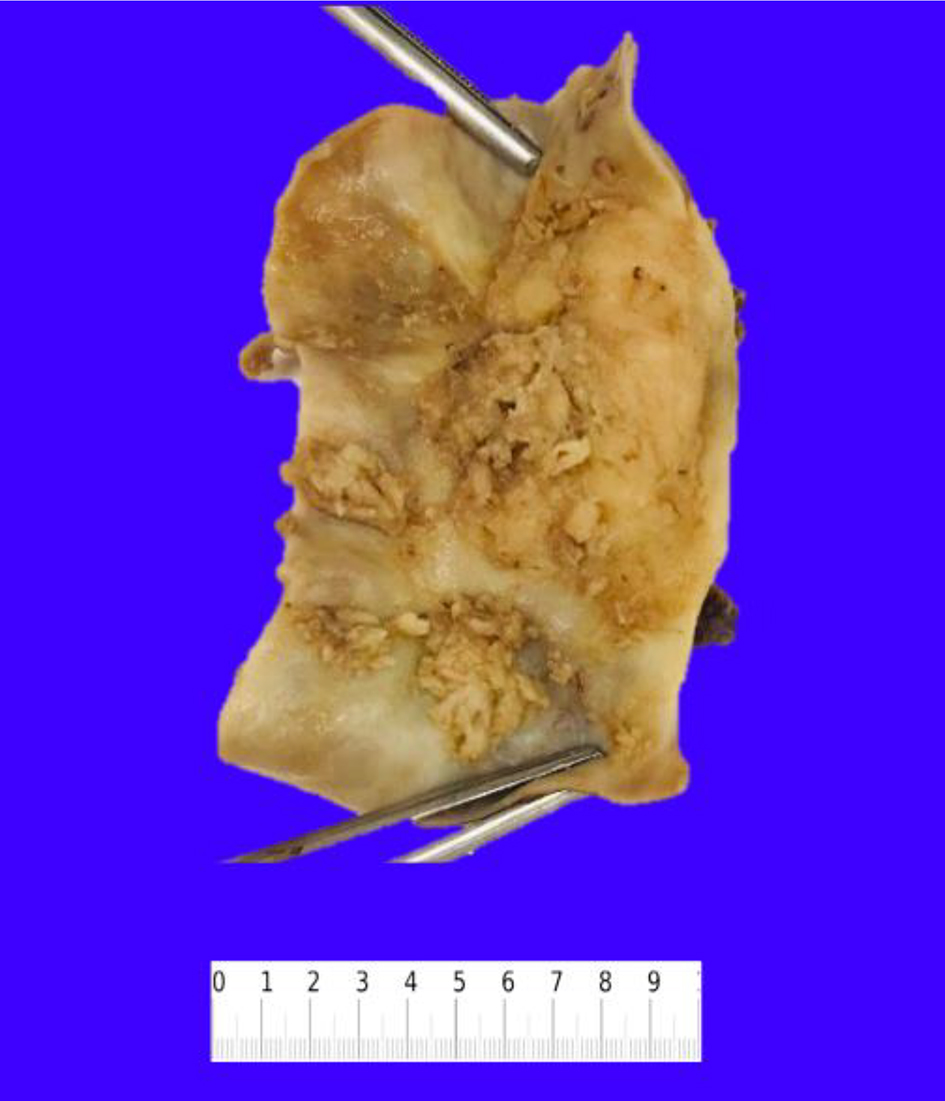
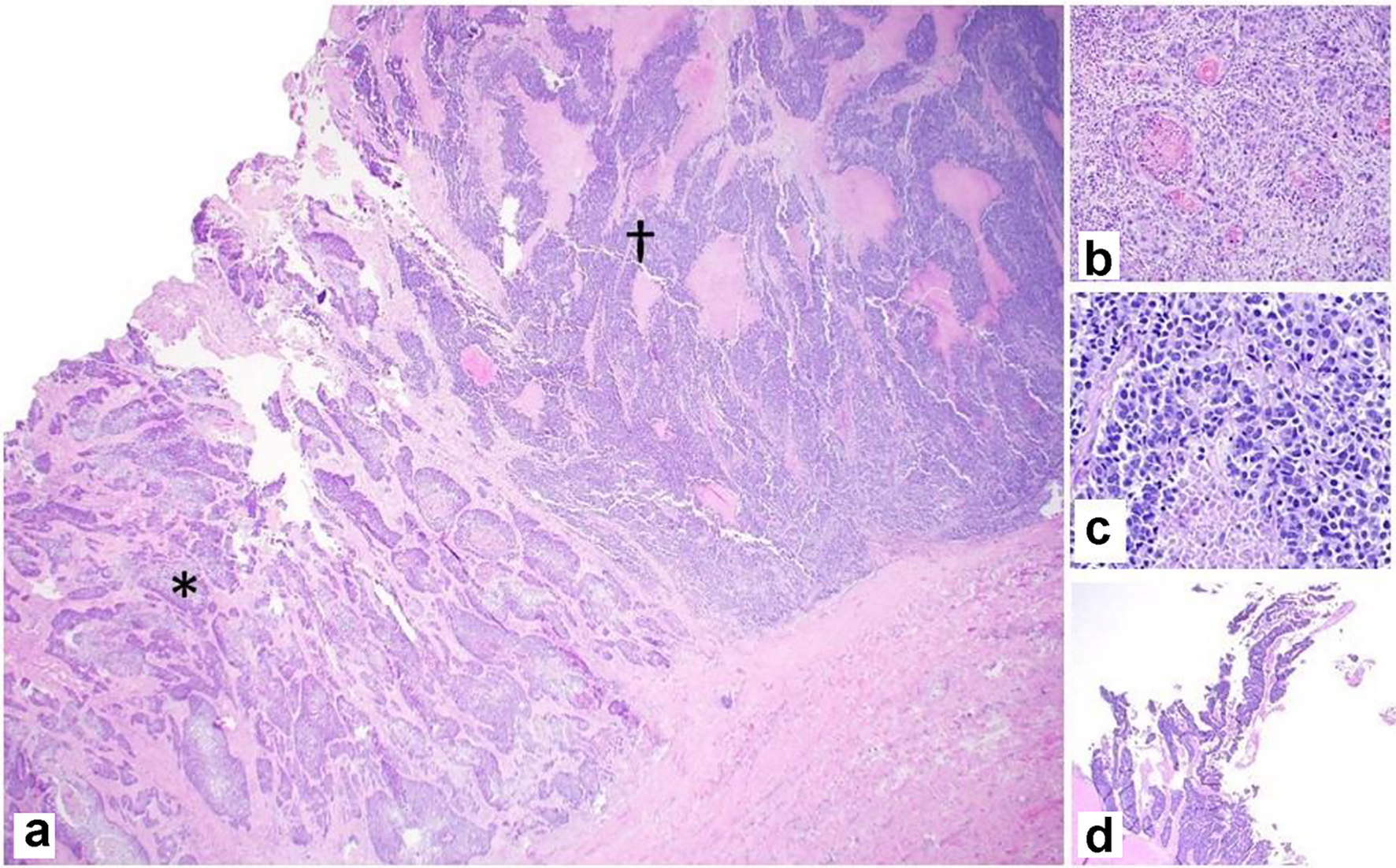
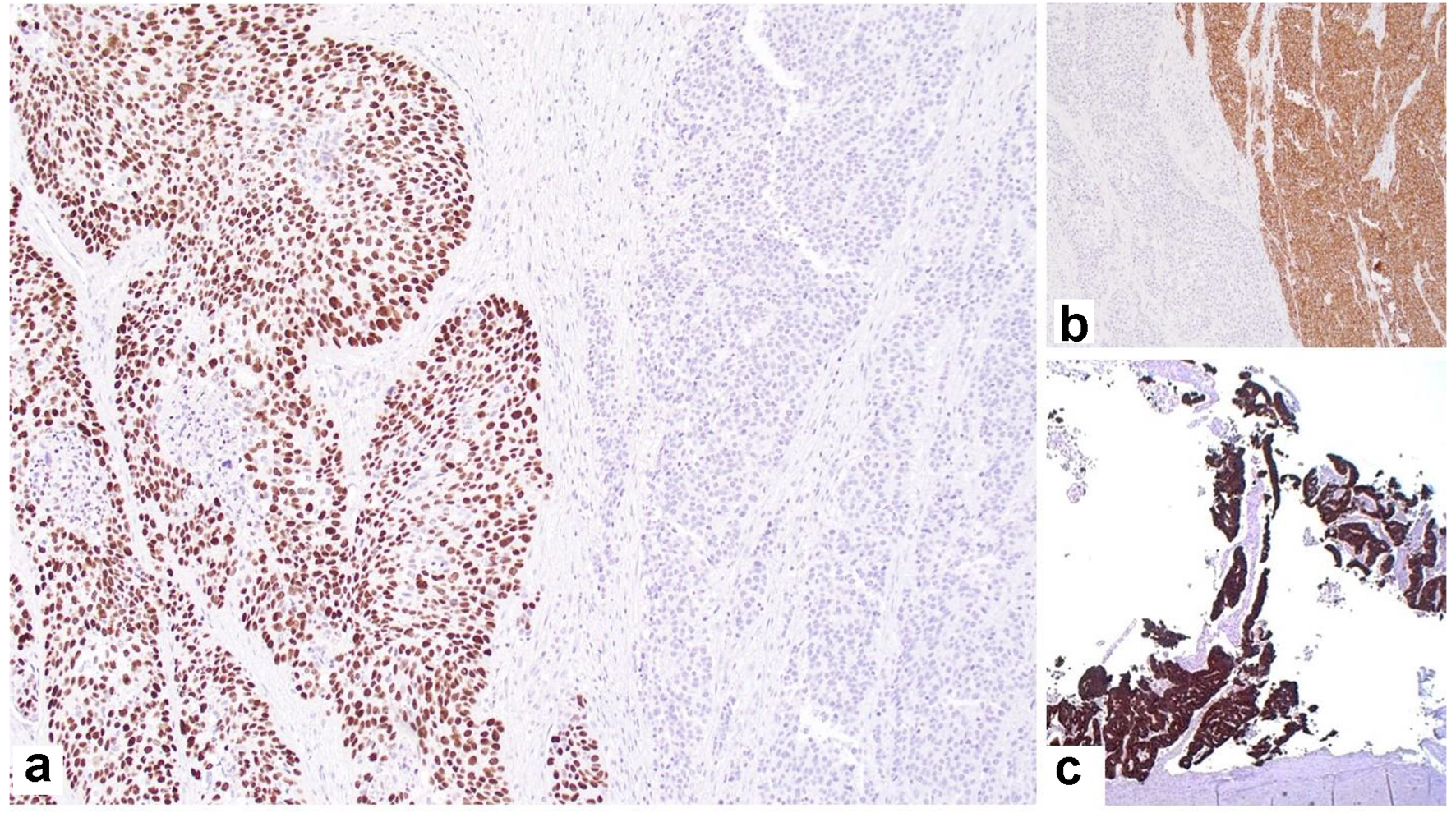
| 30 | F/62 | RUQ pain | P | Fundus/5 | AC (10%), SCC (60%), NEC (30%) | A | Umbilicus | Chol, Phx, Chem (5-FU, Leuc, Oxa) | Alive (14) | Present patient |