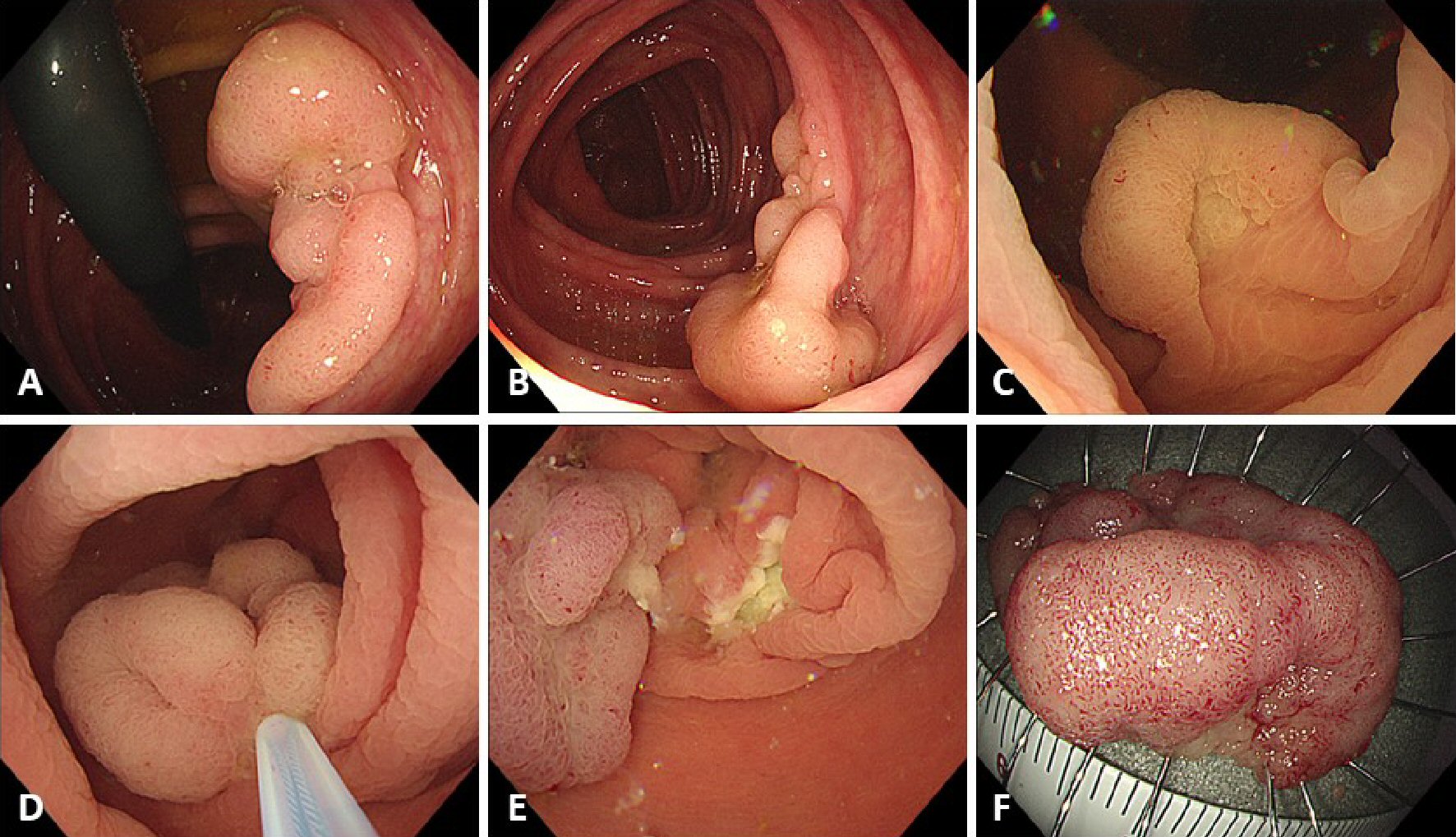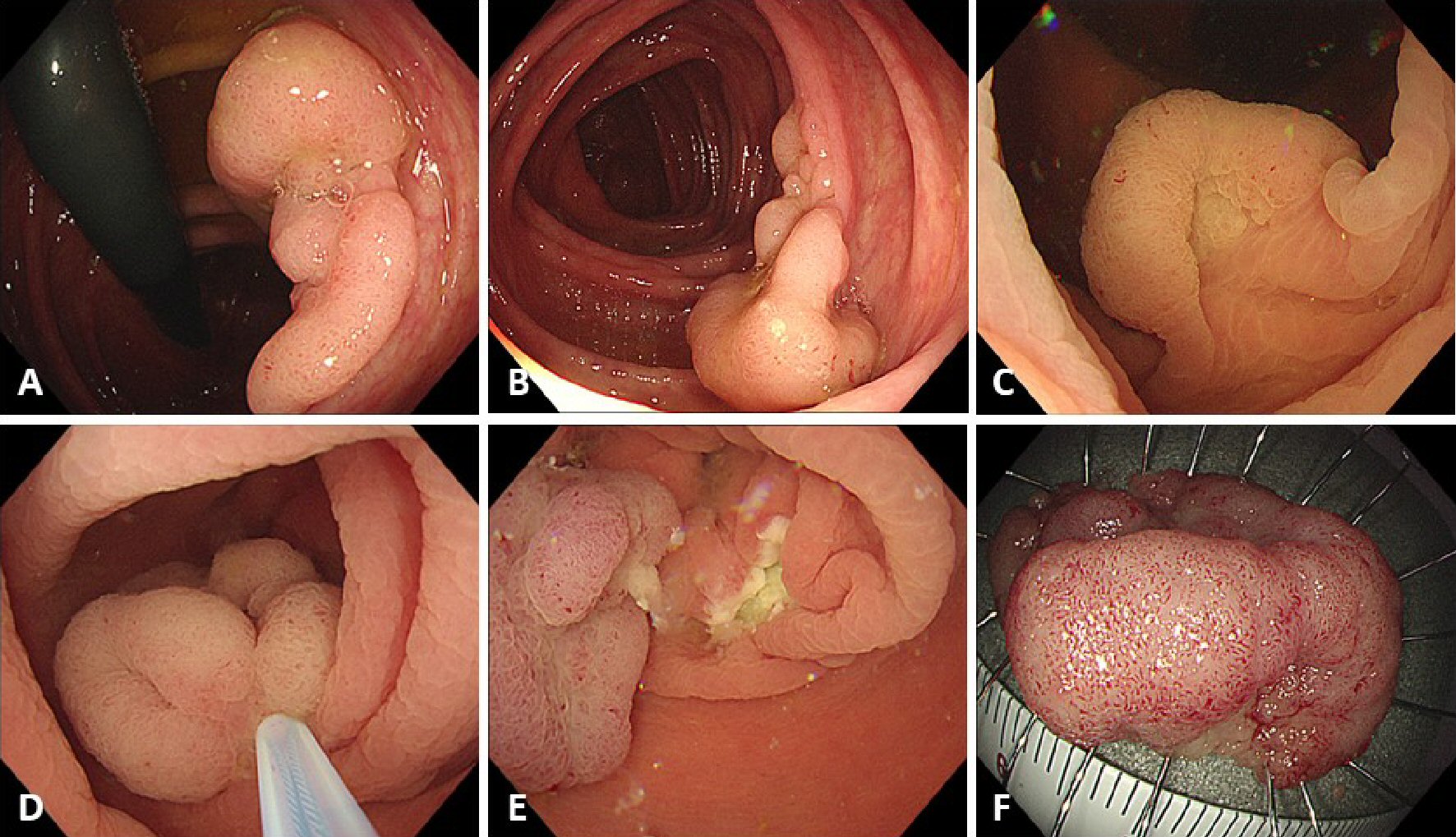
Figure 1. Procedure for underwater endoscopic mucosal resection (U-EMR). (A, B) A sessile lesion about 30 mm located in the ascending colon. (C) The lumen at the site of the lesion was filled with water, using the water-jet system, and the lesion was floated in the lumen. (D) The lesion was snared, using a 33-mm snare, and the lesion was tightened-up. (E) The mucosal defect after U-EMR was usually smaller than after conventional EMR. (F) Resected specimen after successful en bloc resection.
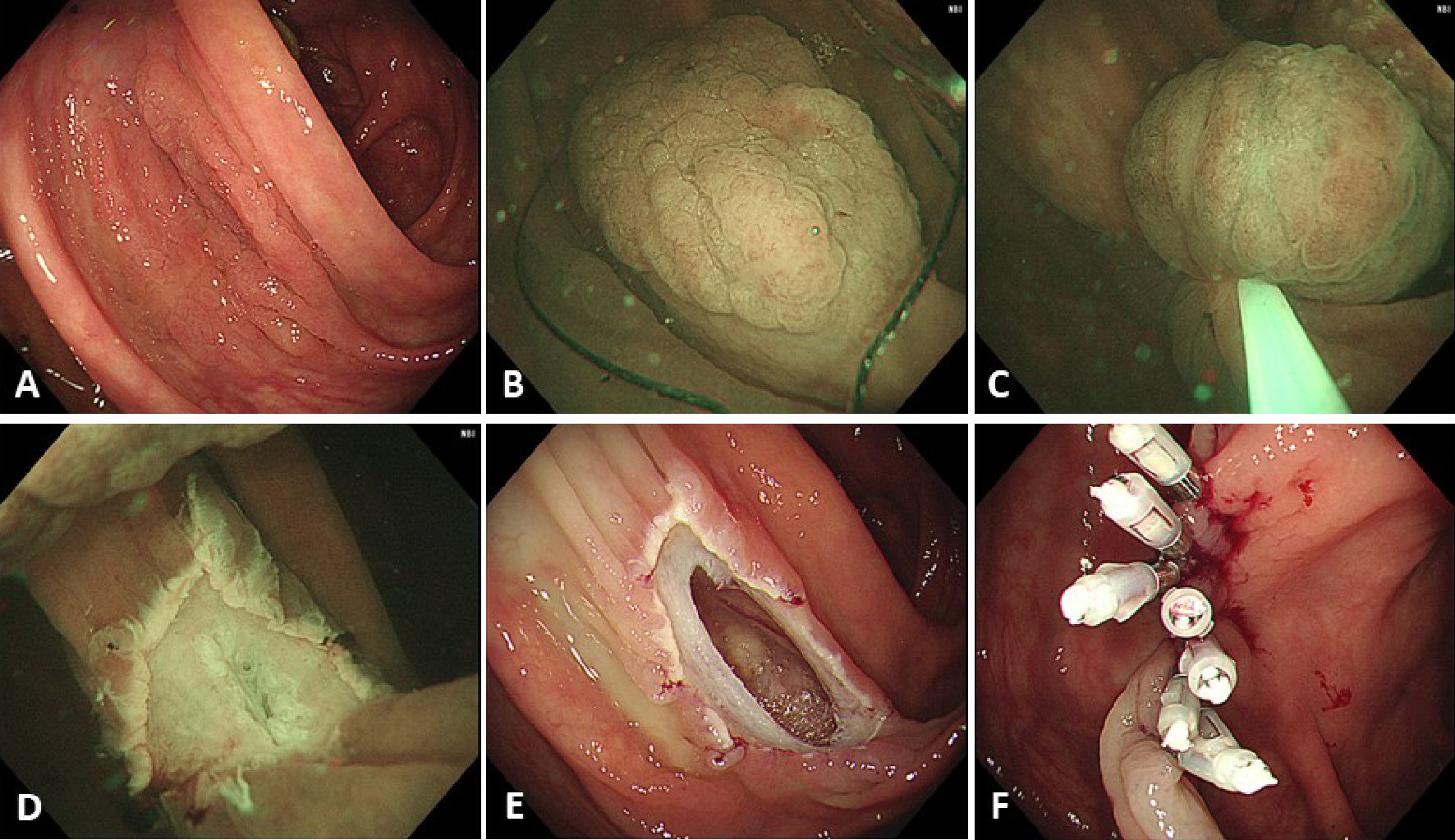
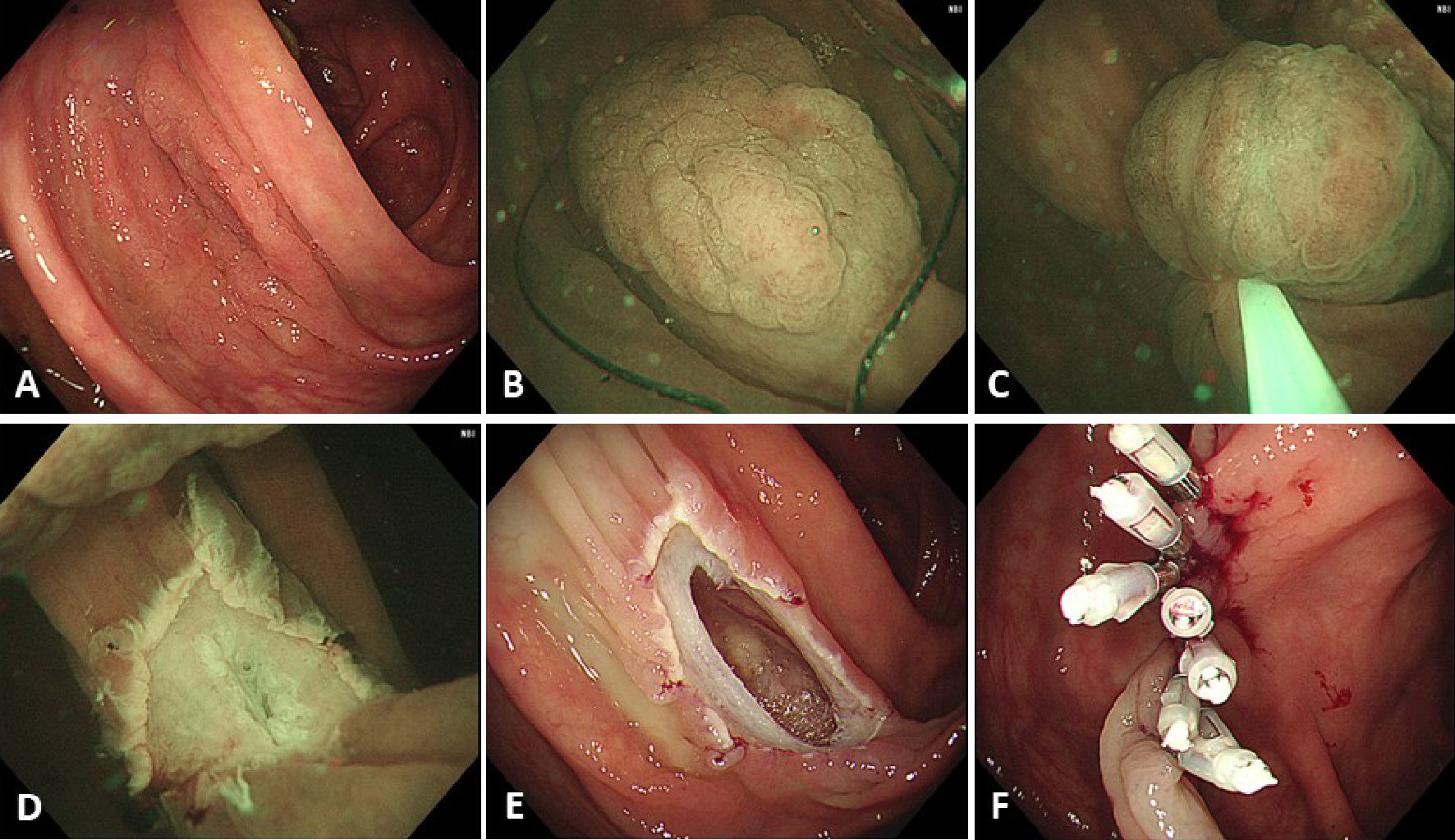
Figure 2. A case of perforation. (A) A laterally spreading, granular type lesion about 30 mm located in the ascending colon. (B) Adequate floating of the lesion could not be achieved and, therefore, submucosal injection, using normal saline, was performed before snaring. (C) The lesion was snared, using a 33-mm snare, and the lesion was tightened-up. (D) En bloc resection was achieved but the muscularis propria was slightly injured at the center of the mucosal defect. (E) An obvious perforation was identified after gas insufflation in the lumen. (F) Endoscopic clipping was performed, and surgical intervention was not required.